1. Background
The rising prevalence of childhood obesity is a major health problem worldwide (1, 2). Increasing evidence reveals that overweight children are at increased risk for various chronic diseases later in life (3). The latest national data in the United States suggest a 17% prevalence of childhood obesity (4). In Iran according to the childhood and adolescence surveillance and prevention of Iranian adult non-communicable disease (CASPIAN) study, more than 8.8% of school-age children are presently overweight and another 4.5% are obese (5). Additionally, findings of recent cross-sectional studies conducted in Tehran indicated that overweightness and obesity are highly prevalent among adolescents residing in Tehran (6, 7). In the study conducted by Hatami et al. on 1157 adolescents, 20.7% were overweight or obese (6). Another study by Jalali-Farahani et al. on 465 high school students showed that 38.5% of them were overweight or obese (7). These findings have led to a widely held view that pediatric obesity interventions are urgently required.
Behavioral strategies are considered the first line of implementation for obesity prevention in the early years of life (8). Previous quantitative studies in Iran primarily have described obesity-related behaviors in adolescents, without much insight to why they are engaged in such behaviors (9-11). Accordingly, there are related reviews demonstrating significant numbers of youth obesity interventions that have demonstrated modest results so far (12-14). Hence, there is a growing need for health professionals to become capable of assessing the factors that determine lifestyle in a culturally relevant manner.
There are several instruments already developed to assess lifestyle in children and adolescents (15-18); however, prior to the Inventory Determinants of Obesity-Related Behaviors in Adolescents (IDOBA), there was no known instrument to assess the culturally relevant determinants of obesity-related behaviors in Iranian adolescents. The IDOBA was developed to fill the gap in current literature available on measures previously developed.
2. Objectives
This study aimed to develop and assess validity and reliability of the IDOBA, in a diverse sample of overweight and obese adolescent residents of Tehran, Iran.
2.1. The Conceptual Framework
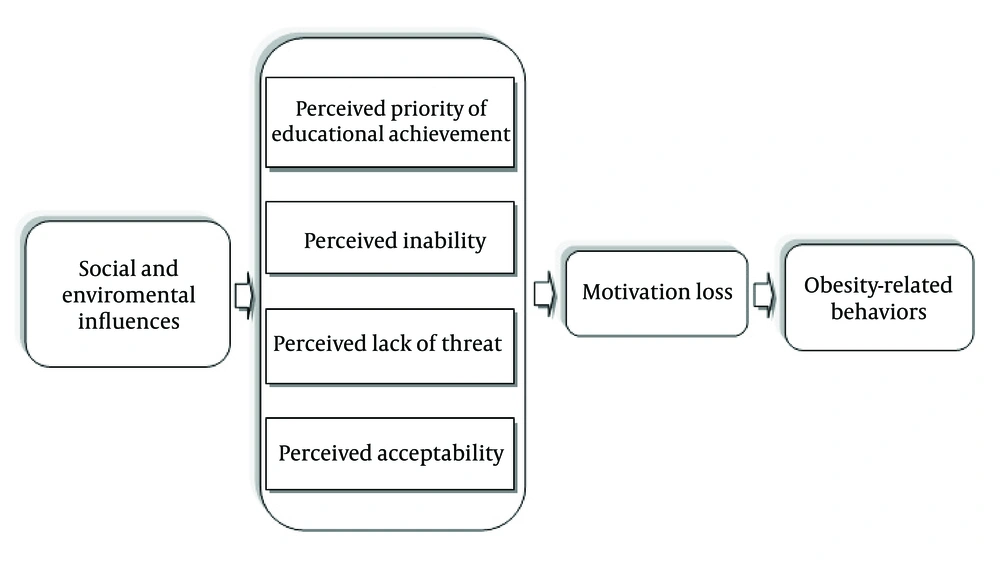
The conceptual framework for this study was based on the results of a qualitative research, using a grounded theory approach with participation of 51 overweight/obese adolescents (19). This framework hypothesizes that influenced by socio-environmental factors and personal characteristics, predisposing beliefs in adolescents form the basis, which results in their unhealthy lifestyles. These beliefs include perception of educational achievement priority, acceptability, lack of threat, and inability to control weight, which induces a psychologic condition that decreases adolescent motivation towards healthy behaviors (Figure 1).
3. Patients and Methods
3.1. Subjects and Settings
Subjects were adolescents, aged 13 to 18 years. To maximize the heterogeneity of the sample, subjects were recruited from schools of two diverse socio-economic areas of Tehran, Iran, one located in the north of Tehran, where the socio-economic status of people is mostly high, and the other, in the south of the city with low socio-economic status. These schools were informed of the study protocol and goals. Inclusion criteria were age of 13 to 18 years and being overweight or obese; an exclusion criterion was presenting with complaint of some obesity-related diseases such as thyroid disorders, based on adolescents’ reports. Participants were recruited from these schools and written parental informed consent and child assent were obtained. Overweightness and obesity were assessed by body mass index (BMI), calculated as weight in kilograms divided by square of height in meters. Based on the standardized percentile curves of BMI, suggested for Iranian children and adolescents, overweightness and obesity were defined as BMI of ≥ 85th to < 95th percentile, and more or equal than 95th percentile, respectively (20). Weight and height were measured with participants wearing light clothes and without shoes, using standard apparatus. Weight was measured to the nearest 0.1 kg on a calibrated beam scale (Seca 707; range, 0.1 - 150 kg; Hanover, MD, Germany). To measure height, a rigid tape measure was fixed to the wall, while the participant stood with heels, buttocks, shoulders, and occiput touching the vertical tape. All measurements were taken by the same person to eliminate subjective error. Adolescents completed the IDOBA themselves and a research assistant was available to answer their questions, after the instructions had been clarified. The scientific research committee of the Tarbiat Modares University (TMU), Tehran, Iran, approved the study.
3.2. Measures
3.2.1. Inventory of Determinants of Obesity-Related Behaviors in Adolescents
The 44-item IDOBA, developed through a qualitative study, encompasses the followings: 1) Unhealthy nutrition and physical inactivity; 2) Stress-related behaviors; 3) Perceived inability; 4) Perceived lack of threat; 5) Perceived priority of educational achievement; 6) Perceived acceptability; 7) Motivation loss; and 8) Lack of support.
3.2.2. Inventory of Determinants of Obesity-related Behaviors in Adolescents; Information Form
The IDOBA information form, completed by adolescents, contained demographic information on the adolescents and their families. It also asked about the adolescent’s chronic diseases, which could have affected or resulted in their obesity-related behaviors or weight gain during the past six months. Furthermore, it included questions about their experiences regarding weight control and their satisfaction with the outcomes of previous efforts to lose weight.
3.3. Scale Development Procedure
Scale development began with concept identification, and is followed by different steps including concept analysis, item writing, face and content validity, reliability assessment, and construct validity assessment (21). Accordingly, each of the theory constructs were transformed to lower level concepts and then stated as variables in quantitative terms, using the results of the initial qualitative study and literature review. Considering the theoretical definition and attributes of the concept derived from the first step, an initial blueprint consisting of 91 items was generated. Each item was rated on a five-point Likert scale anchored at one to five (always to never and strongly agree to strongly disagree).
Validity of IDOBA was assessed by face, content, and construct validity methods. To confirm face validity, ten overweight/obese adolescents completed the questionnaire and provided information such as whether the initial items were relevant to them and if so, how important each issue was in their daily lives. Regarding qualitative content validity, an expert panel of ten specialists in health education, endocrinology, nutrition, psychology, and physical activity examined the initial questionnaire. The panel was asked to comment on individual items in relation to the accuracy and style. Items were modified based on the experts’ comments. To calculate content validity ratio (CVR) and content validity index (CVI), a different panel of ten experts was asked to comment independently on the necessity, relevance, clarity, and simplicity of each item. The necessity of the items was assessed using a three-point rating scale: 1, not necessary; 2, useful, but not essential; and 3, essential. Following the experts’ assessments, a CVR for total scale was computed, according to Lawshe scores (22). The relevance of the items was also assessed, using a four-point rating scale: 1, not relevant; 2, slightly relevant; 3, relevant; and 4, completely relevant. The CVI of each question was determined by the proportion of experts rating the item as more or equal than 3 (23). After performing construct validity and detection of IDOBA subscales, the reliability was assessed, using internal consistency reliability and test-retest. For the test-retest reliability of the scale, it was re-administered to 56 individuals one month after the first completion. The average length of time it took for subjects to complete the test was 20 minutes.
3.4. Statistical Analysis
Range of measurement was based on the percentage of scores at the extremes of the scaling range, ie, the maximum (ceiling effect) and the minimum (floor effect) possible scores (24). Reliability of scale internal consistency was determined by calculating Cronbach’s Alpha coefficient. Values > 0.6 were considered as satisfactory. The test-retest reliability of the scale was evaluated using the intra-class correlation coefficient (ICC), and ICCs > 0.6 were considered acceptable.
Exploratory factor analysis (EFA) was used to assess construct validity and derivate IDOBA subscales. Kaiser-Meyer-Olkin (KMO), measure of sampling adequacy, Bartlett’s test of sphericity, and total variance explained were used for the evaluation of model adequacy. The EFA was performed by the extraction method of principal component analysis, utilizing Varimax rotation with Kaiser normalization. In this analysis, loadings over cutoff values of 0.3 were considered as important and the items remaining in the model were based on this criterion. Confirmatory factor analysis (CFA) was performed to test whether the data fit the hypothesized measurement model, which was extracted by EFA. Weighted least squares (WLS) estimation method was used at CFA. Asymptomatic covariance matrix was considered as a weighted matrix. Goodness-of-fit indices (GFIs) and reasonable threshold levels of these indices for CFA were considered as χ2/df < 3, root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR) < 0.08 as well as comparative fit index (CFI), goodness-of-fit index (GFI), and normed fit index (NFI) > 0.9 (25). Statistical analysis was performed using SPSS 22.0 (SPSS Inc., Chicago, Illinois, the United States) and LISREL 8.80 (Scientific Software International Inc, 2007).
4. Results
A total of 478 adolescents (57.7% male) aged 13 to 18 years participated in the study. Mean BMI was 30.25 ± 4.22 kg/m2. Levels of education, occupation status of parents, and their mean age are reported in Table 1. Most fathers and mothers were educated up to secondary levels (38.1% and 50.1%, respectively). Most fathers had non-governmental jobs (64.6%), whereas the highest proportions of mothers were House wife (79.9%).
| Variables | Values b |
|---|---|
| Sex | |
| Female | 202 (42.3) |
| Male | 276 (57.7) |
| Grade | |
| 1st grade | 180 (37.7) |
| 2nd grade | 123 (25.7) |
| 3rd grade | 122 (25.5) |
| 4th grade | 53 (11.1) |
| Fathers’ level of education | |
| Primary | 112 (24.1) |
| Secondary | 177 (38.1) |
| Higher | 176 (37.8) |
| Mothers’ level of education | |
| Primary | 113 (23.9) |
| Secondary | 237 (50.1) |
| Higher | 123 (26.0) |
| Fathers’ occupation | |
| Governmental job | 115 (24.7) |
| Non-governmental job | 301 (64.6) |
| Unemployed | 12 (2.6) |
| Retired | 38 (8.1) |
| Mothers’ occupation | |
| Governmental job | 50 (10.6) |
| Non-governmental job | 34 (7.2) |
| House wife | 377 (79.9) |
| Retired | 11 (2.3) |
| Body mass index, kg/m2 | 30.25 ± 4.22 |
| Fathers’ age, y | 47.75 ± 6.31 |
| Mothers’ age, y | 41.67 ± 5.53 |
a The total number of participants was 478.
b Values are presented as No. (%) or mean ± SD.
Based on the face validity results, all questionnaire items were generally easy to read and understand for adolescents; however, a few words were changed to meet participants’ considerations. Of 91 items, 89 (97.8%) were labeled as “important” to them. Qualitative content validity was confirmed by the panel of experts and findings regarding the CVR and CVI confirmed the quantitative content validity of 75 items. The CVR in this study for total scale was 0.82, indicating a satisfactory result. A satisfactory level of agreement was found (CVI = 0.92) among panelists suggesting that the scale had a good content validity. No floor effects were observed. Detected ceiling effects ranged from 2.7% for perceived priority of educational achievement subscale score to 12.9% for stress-related eating.
In case of EFA, KMO showed a reasonable fit of the model (KMO = 0.78), and the Bartlet’s test confirmed the sphericity assumption (χ2 = 5469.4, df = 946, and P < 0.001). The extracted eight factors were based on eigenvalues > 1.25. The percentage of the total variance was 49.06% by the rotated eight factors. Factor loadings and explained variance of each factor are illustrated in Table 2. All items were loaded between 0.30 and 0.89 on their corresponding factors. The results of the CFA for eight-factor hypothesized model are reported in Table 3 and indicate acceptable fit of the proposed model. Minimum factor loadings was 0.12 (t = 6.56) for question number 7 (from the unhealthy nutrition and physical activity subscale) and maximum factor loadings was 0.99 (t = 33.88) for question number 14 (from the perceived inability subscale).
| Questions | Subscales | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Lack of support | ||||||||
| Q42 | 0.703 | |||||||
| Q41 | 0.666 | |||||||
| Q38 | 0.650 | |||||||
| Q43 | 0.597 | |||||||
| Q37 | 0.556 | |||||||
| Q40 | 0.549 | |||||||
| Q34 | 0.545 | |||||||
| Q39 | 0.538 | |||||||
| Q44 | 0.521 | |||||||
| Q35 | 0.480 | |||||||
| Q36 | 0.434 | |||||||
| Motivation loss | ||||||||
| Q30 | 0.724 | |||||||
| Q32 | 0.691 | |||||||
| Q33 | 0.676 | |||||||
| Q31 | 0.662 | |||||||
| Q28 | 0.630 | |||||||
| Q27 | 0.576 | |||||||
| Q29 | 0.383 | |||||||
| Perceived priority of educational achievement | ||||||||
| Q24 | 0.751 | |||||||
| Q23 | 0.735 | |||||||
| Q25 | 0.716 | |||||||
| Q22 | 0.575 | |||||||
| Q26 | 0.432 | |||||||
| Unhealthy nutrition and physical inactivity | ||||||||
| Q3 | 0.665 | |||||||
| Q1 | 0.595 | |||||||
| Q2 | 0.578 | |||||||
| Q4 | 0.573 | |||||||
| Q8 | 0.495 | |||||||
| Q7 | 0.471 | |||||||
| Q5 | 0.441 | |||||||
| Q6 | 0.410 | |||||||
| Perceived acceptability | ||||||||
| Q17 | 0.730 | |||||||
| Q15 | 0.676 | |||||||
| Q16 | 0.654 | |||||||
| Q19 | 0.588 | |||||||
| Q18 | 0.556 | |||||||
| Perceived inability | ||||||||
| Q14 | 0.885 | |||||||
| Q13 | 0.872 | |||||||
| Q12 | 0.401 | |||||||
| Stress-related eating | ||||||||
| Q11 | 0.683 | |||||||
| Q10 | 0.668 | |||||||
| Q9 | 0.568 | |||||||
| Perceived lack of threat | ||||||||
| Q21 | 0.714 | |||||||
| Q20 | 0.652 | |||||||
| Explained variance | 8.98 | 8.38 | 6.40 | 5.93 | 5.89 | 4.94 | 4.54 | 3.99 |
| Model | χ2 | df | χ2/df | RMSEA | CFI | GFI | NFI | SRMR |
|---|---|---|---|---|---|---|---|---|
| Values | 2178.53 | 874 | 2.49 | 0.056 | 0.99 | 0.92 | 0.99 | 0.071 |
The mean of subscale scores and number of items in each subscale are presented in Table 4. To calculate subscale scores, all items in the corresponding subscale were summed and transformed to a zero to 100 scale. No ceiling effects were observed. Detected floor effects ranged from 0.2% for perceived acceptability subscale score to 18.8% for lack-of-threat subscale score. The Cronbach’s alpha was calculated for each subscale and ranged from 0.61 to 0.81. Minimum and maximum ICC of items in each subscale are reported in Table 4; question No. 16 from the perceived acceptability subscale had low ICC, which could be due to the long interval between test and retest measurement.
| Number of Items | Mean ± SD | Ceiling | Floor | Cronbach’s α | Test-Retest | ||
|---|---|---|---|---|---|---|---|
| Min | Max | ||||||
| Unhealthy nutrition and physical inactivity | 8 | 50.2 ± 12.6 | 0 | 0 | 0.66 | 0.68 | 0.91 |
| Stress-related eating | 3 | 44.0 ± 17.8 | 0.8 | 12.6 | 0.61 | 0.64 | 0.79 |
| Perceived inability | 3 | 62.2 ± 20.9 | 0 | 0 | 0.67 | 0.70 | 0.84 |
| Perceived lack of threat | 2 | 49.8 ± 23.6 | 6.5 | 18.8 | 0.62 | 0.60 | 0.80 |
| Priority of educational achievement | 5 | 52.9 ± 20.2 | 1.5 | 6.7 | 0.74 | 0.59 | 0.78 |
| Perceived acceptability | 5 | 73.8 ± 17.9 | 6.1 | 0.2 | 0.73 | 0.42 | 0.80 |
| Motivation loss | 7 | 46.4 ± 17.5 | 0.4 | 5.6 | 0.80 | 0.61 | 0.87 |
| Lack of support | 11 | 49.1 ± 16.8 | 0 | 4 | 0.81 | 0.60 | 0.80 |
a The total number of participants was 478.
5. Discussion
Our results indicated that the IDOBA facilitates a reliable and valid measurement of determinants of obesity-related behaviors in Tehranian adolescents. Its internal consistency reliabilities generally exceeded the standard of 0.70, and all subscales demonstrated satisfactory test-retest reliability, consistent with other similar self-reporting measures (17, 26, 27).
Research on explanations of the obesity-related behaviors process in adolescents has been less extensive than that on description of these behaviors, as it is hindered by a lack of related conceptual frameworks. Accordingly, there is a lack of empirical instruments to assess lifestyle determinants in the earlier years of life. Among the available instruments, each of the adolescent life style questionnaire (ALQ) and the Adolescent Lifestyle Profile (ALP) focus on seven domains of a healthy life style in adolescents (16, 17). Moreover, a recently reported questionnaire, HABITS, was developed to assess pediatric lifestyle and weight management by measuring children’s food intake and physical activity/sedentary behavior (15). There is also another instrument, the Life Style Behavior Checklist (LBC), developed to measure parents’ challenges faced in managing their children behaviors and how these challenges might be addressed in treatment (18).
As a theory-based questionnaire, the IDOBA differs from the earlier mentioned instruments, which focused mainly on measuring sedentary behaviors or barriers to healthy lifestyles in children and adolescents. Recent evidence about moderate goal achievements of childhood obesity prevention programs indicates that these efforts should be based on culture related knowledge (12-14). Based on this premise, all items of the IDOBA were designed and developed to measure potential factors that contribute to decreased adolescent motivation regarding healthy behaviors according to a context-based conceptual framework. This framework indicates the central role of motivation loss that results in obesity-related behaviors and excessive weight gain in adolescents in Tehran. This motivation loss could be a result of adolescents’ beliefs and perceptions, including prioritized educational achievement, acceptability, inability for weight control, and lack of threat, which are affected by certain socio-environmental and personal characteristic (19). However, the items of the IDOBA are not unique to Iranian adolescents and could be relevant for other ethnic groups, which would require basic but essential assessments.
The IDOBA is a simple instrument, which is developed for researchers and healthcare professionals to assist in identifying the underpinning factors of obesity-related behaviors in adolescents in Tehran and to developing prevention programs to overcome barriers to a healthy lifestyle. However, the generalizability of the current findings are limited for the following reasons:
1) The participants of this study were limited to urban Tehranian adolescents; 2) The information of nonparticipants was not available; and 3) Due to limited access to socio-economic data, the studied population could not be considered as a representative sample of adolescents from different socio-economic statuses in Tehran.
In conclusion, the IDOBA was designed to measure determinants of obesity-related behaviors in adolescents, based on the conceptual constructs that emerged from the initial qualitative study and a literature review. To confirm its current validity results, further evaluation with larger Iranian rural and urban populations with different socio-economic statuses is recommended.
| Factor 1: Unhealthy nutrition and physical inactivity |
| 1. I have high calorie foods (sandwich, pizza, French fries, cake, chips, and doughnut) for lunch and dinner. |
| 2. I have high calorie foods and drinks (sandwich, cake, chips, chocolate, cheese puffs, ice cream, doughnut, and sugary sodas) as snacks. |
| 3. I drink sugary sodas with lunch and dinner. |
| 4. I have mayonnaise with lunch and dinner. |
| 5. I have high calorie foods and snacks with friends in social gatherings. |
| 6. I watch TV for more than 2 hours per day. |
| 7. I go online or play video games for more than 2 hours a day. |
| 8. I spend more than 2 hours a day with my friends on the phone. |
| Factor 2: Stress-related eating |
| 9. I eat while studying and doing my homework. |
| 10. I overeat when I am excited or stressed. |
| 11. I overeat when I have nothing to do. |
| Factor 3: Perceived Inability |
| 12. I do not try to lose weight, because I believe obesity is hereditary. |
| 13. I do not try to lose weight, because I am not satisfied with the amount of weight I lose. |
| 14. I do not try to lose weight, because I am not satisfied with the speed of my weight loss. |
| Factor 4: Perceived Acceptability |
| 15. I can exercise as much as my peers can. |
| 16. I believe that I receive as much attention as my peers do. |
| 17. I can wear my favorite clothes like my peers. |
| 18. I am satisfied with who I am. |
| 19. I feel comfortable among people. |
| Factor 5: Perceived Lack of Threat |
| 20. I worry about my weight when I see obese relatives suffer from diseases. |
| 21. I worry about my weight because of serious consequences of obesity and dangerous related diseases. |
| Factor 6: Perceived Priority of Educational Achievement |
| 22. I do not start a diet because it affects my studies and I do not do as well. |
| 23. I do not exercise because it takes away from my study time. |
| 24. I cannot lose weight because of school exams |
| 25. I cannot lose weight because of educational competition with my friends |
| 26. I do not exercise when I am too tired or do not feel like it. |
| Factor 7: Motivation Loss |
| 27. I intend to lose weight during the next 6 months. |
| 28. I intend to decrease my intake of fatty and sweet foods during next 10 days. |
| 29. I intend to start exercising regularly during next 10 days. |
| 30. I will follow my weight loss diet even if it is difficult. |
| 31. I do not overeat even if nobody is monitoring my eating. |
| 32. I reject my friend’s food offers to lose weight. |
| 33. I maintain the weight that I have lost |
| Factor 8: Lack of Support |
| 34. I cannot lose weight because my parent do not prepare low calorie foods for me |
| 35. I cannot go for walking or exercise because my parents do not accompany me |
| 36. Media advertisements motivate me to consume fatty and sweet foods |
| 37. I have no access to the information necessary for weight loss |
| 38. I cannot exercise because of the limited space in our house |
| 39. I cannot exercise in public places because this not common |
| 40. I cannot lose weight because our school food buffet doesn’t offer healthy snacks |
| 41. I cannot go on diet because healthy foods like fruits and meats are expensive |
| 42. I cannot exercise because of the high cost of exercise classes. |
| 43. I cannot exercise because the exercise classes are either too far away or the class times do not coordinate with my schedule. |
| 44. I cannot exercise because of heavy traffic and air pollution |