1. Background
Hypothyroidism is a common disorder (1). Patients with hypothyroidism require thyroid hormone replacement, and levothyroxine is the preferred therapy. Most patients require approximately 1.6 mcg/kg of levothyroxine daily (1). Occasionally, patients remain hypothyroid despite being prescribed very high levothyroxine doses. One cause of apparent levothyroxine therapy failure is poor gut absorption, a well-recognized phenomenon with numerous causes, including malabsorptive conditions (e.g. celiac, pancreatic insufficiency, jejuno-ileal bypass surgery), interference by food or supplements (e.g. calcium, iron) and concomitant medications (e.g. laxatives, antacids) (2-5). Another cause is nonadherence to levothyroxine therapy (3, 6, 7). An effective way to distinguish nonadherence from malabsorption is to perform levothyroxine absorption testing. This testing is typically performed by administering a single large oral dose of levothyroxine then measuring serum FT4 levels over the subsequent 4 to 24 hours (3, 7-12).
2. Objectives
Given that levels of FT4 are at or near their peak 2 hours after levothyroxine ingestion (7-14), we hypothesized that a levothyroxine absorption test could be completed in only 2 hours. We present the successful completion of 2-hour levothyroxine absorption testing in 3 patients found to be nonadherent to levothyroxine therapy.
3. Patients and Methods
We performed a retrospective case series of 3 patients. All patients were scheduled to have levothyroxine absorption testing approximately 3 weeks after they agreed to perform the test. Patients were instructed to skip their usual dose of levothyroxine on the day of the test. They were asked arrive by 8:00 AM for the test after at least an 8 hour fast. Serum levels of TSH, FT4, and FT3 were drawn at 0, 60, and 120 minutes after administration of 1000 mcg of levothyroxine orally as 5 tablets of 200 mcg each.
4. Results
4.1. Case 1
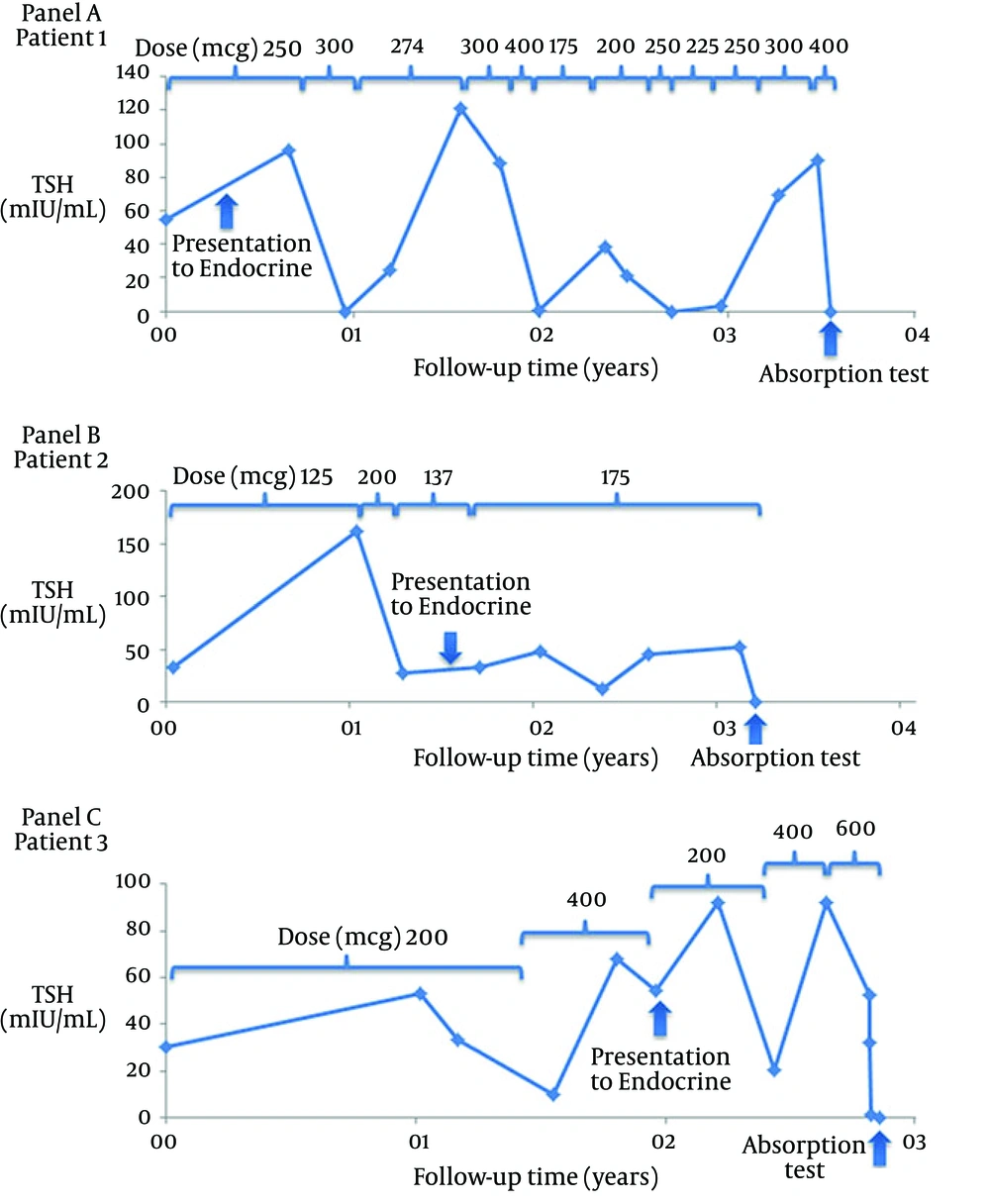
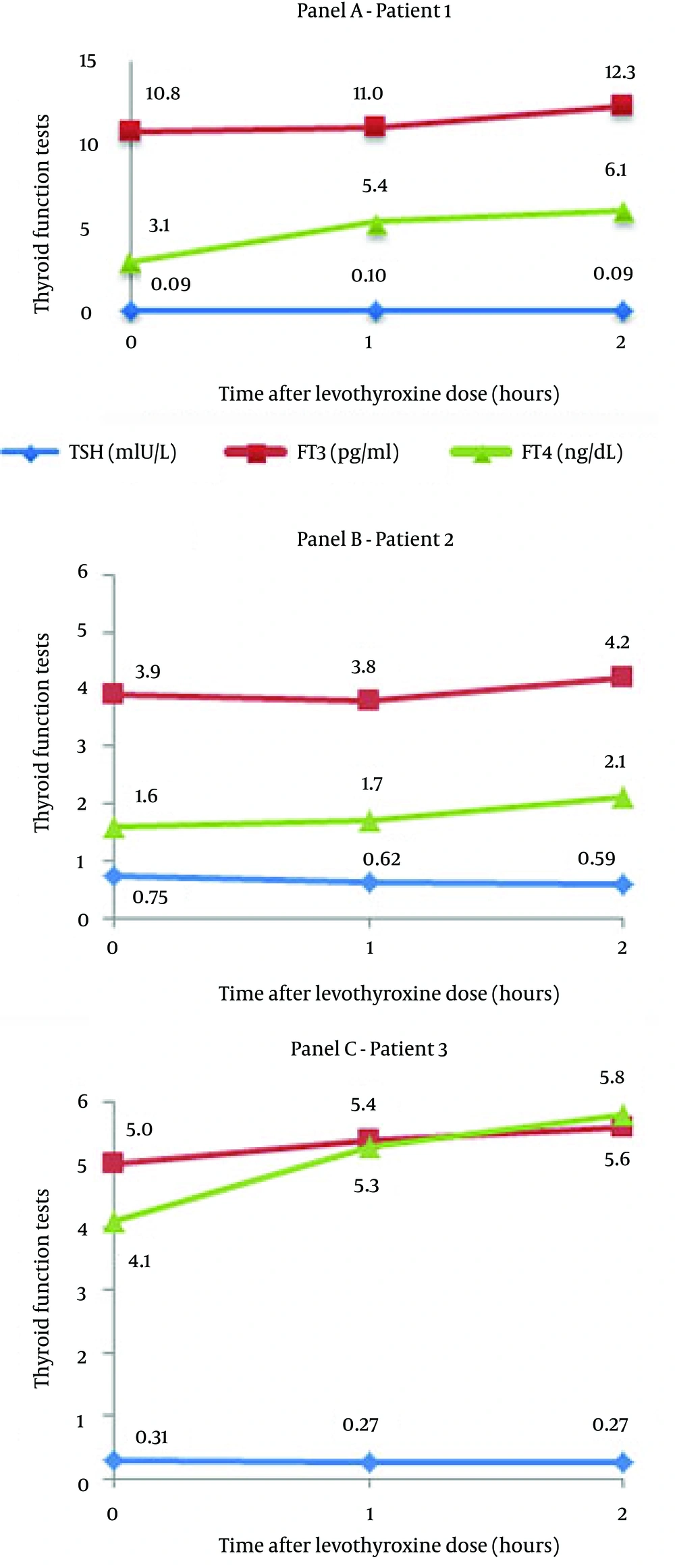
A 44-year-old, 70 kg female with a history of irritable bowel syndrome and primary hypothyroidism due to Hashimoto’s thyroiditis presented with severe hypothyroidism despite being prescribed 250 mcg (3.6 mcg/kg) of levothyroxine daily. She reported taking the levothyroxine regularly in the fasting state without other medications. TSH was 54.96 µIU/mL (normal, 0.40 - 4.50, coefficient of variation [CV] 4.7 - 6.9%) and total thyroxine (T4) was 1.8 µg/dL (normal, 4.5 - 12.5, CV 4.2 - 6.2%). Prescribed levothyroxine doses and TSH levels over time are presented in Figure 1 A. TSH levels were variably high, normal, and low on doses of levothyroxine ranging from 175 to 400 mcg (2.5 to 5.7 mcg/kg) daily. After 3 years of attempted medical management, her TSH was 90.21 µIU/mL on a levothyroxine dose of 300 mcg (4.2 mcg/kg) daily. Upon discussion with the patient, we increased the levothyroxine dose to 400 mcg daily and scheduled a 2-hour levothyroxine absorption test 3 weeks later. Despite a very high TSH level prior to the test, the patient was found to have low TSH and high FT3 and FT4 levels at baseline (Figure 2 A). Both FT4 and FT3 increased substantially during the test. Poor levothyroxine absorption was excluded, and we decreased the dose to 300 mcg daily while reinforcing the importance of adherence. Eight weeks later, the TSH was 0.01 µIU/mL and FT4 was 3.2 ng/dL (normal, 0.8 - 1.8, CV 6.0 - 8.9%). Levothyroxine was further reduced to 150 mcg (2.1 mcg/kg) daily. TSH eventually normalized on 175 mcg daily of levothyroxine.
4.2. Case 2
A 42-year-old, 66 kg female with primary hypothyroidism due to Hashimoto’s thyroiditis was referred to the Endocrinology Clinic for uncontrolled hypothyroidism. The patient reported taking levothyroxine every morning at the prescribed dose of 137 mcg (2.1 mcg/kg) in the fasting state without any other medications. She denied additional medications but did take iron supplements. Otherwise, she had no relevant medical history. Her family history was significant for primary hypothyroidism due to Hashimoto’s in her mother, sister and brother. Review of old records revealed a TSH of 160 mIU/mL while taking 125 mcg daily of levothyroxine (Figure 1 B). The primary care provider increased the levothyroxine dose to 200 mcg (3.3 mcg/kg), which resulted in a TSH of 28 mIU/mL. On this dose, however, the patient developed palpitations and the levothyroxine was decreased to 137 mcg daily. At this point, the patient presented to Endocrinology Clinic. We counseled the patient on adherence and increased the levothyroxine dose to 175 mcg (2.7 mcg/kg) daily, but the TSH remained elevated. After discussion with the patient, we scheduled a rapid levothyroxine absorption test 3 weeks later (Figure 2 B). Similar to Case 1, the baseline TSH was low-normal while peripheral hormone levels were high and became even higher 2 hours after levothyroxine. We reduced the levothyroxine dose to 150 mcg (2.3 mcg/kg) daily and counseled the patient on adherence. The TSH 6 weeks later was 0.23 µIU/mL, and the levothyroxine dose was reduced to 137 mcg daily with subsequent normalization of TSH levels.
4.3. Case 3
A 65-year-old, 87 kg male with a history of primary hypothyroidism secondary to TPO antibody-negative Hashimoto’s thyroiditis presented to the Endocrinology Clinic with uncontrolled hypothyroidism. Other past medical history included hypertension, dyslipidemia, and gout. Medications in addition to levothyroxine included amlodipine, omeprazole, labetalol, allopurinol, colchicine, aspirin, and furosemide. The patient reported taking levothyroxine 200 mcg twice daily (400 mcg daily, 4.6 mcg/kg) on an empty stomach without any other medications. Laboratory studies showed a TSH of 54.26 mIU/L, a FT4 index of 1.0 (normal, 1.4 - 3.8) and total triiodothyronine (T3) of 70 ng/dL (normal, 76 - 181, CV 6.2 - 6.8%) (Figure 1 C). Review of old records revealed variably high TSH levels on reported levothyroxine doses of 200 to 400 mcg daily. The patient was counseled on medication adherence and advised to take levothyroxine 200 mcg daily. Because the TSH was persistently elevated (range 20.21 - 93.32 µIU/mL), the levothyroxine dose was increased to 400 mcg daily then 600 mcg (6.9 mcg/kg) daily.
Ten months after presentation (after 24 months of available follow-up data, Figure 1 C), he was admitted to the hospital with chest pain and symptomatic bradycardia. TSH was 52.50 mIU/L and total T4 was 2.78 mcg/dL on hospital day 1 (HD1). The patient was given his prescribed outpatient levothyroxine dose of 300 mcg twice daily starting at 10 pm on HD1. TSH on HD2 at 6 AM was 32.04 mIU/L with FT4 0.3 ng/dL; on HD3, TSH was 1.65 mIU/L with a FT4 of 0.6 ng/dL. He was discharged on the same regimen of 300 mcg twice daily. Three weeks later, we performed a 2-hour levothyroxine absorption test to confirm adequate absorption. Similar to the other two cases, this patient also had a low TSH and high FT4 and FT3 at baseline. Also like the other cases, there was an increase in FT4 and FT3 in response to 1000 mcg of levothyroxine (Figute 2C). The levothyroxine dose was subsequently decreased to 200 mcg daily. Approximately 8 weeks later, the TSH was 0.05 mIU/L and FT4 was 2.0 ng/dL. Therefore the levothyroxine dose was further decreased to 150 mcg (1.7 mcg/kg) daily, and the TSH 10 weeks later was 0.83 mIU/L.
Each panel represents a single patient. Baseline levels of TSH were low and FT3 and FT4 were high or high normal, indicating that these patients had started taking their levothyroxine prior to the absorption test. FT4 increased during the test, further corroborating adequate levothyroxine absorption. TSH (◊, normal 0.40 - 4.50, CV 4.7 - 6.9%), FT3 (□, normal 2.3 - 4.2, CV 5.8 - 8.3%), FT4 (∆, normal 0.8 - 1.8, CV 6.0 - 8.9%).
5. Discussion
We describe a rapid (2-hour) levothyroxine absorption test performed successfully in 3 patients. All 3 patients presented with high TSH levels over a period of 24 to 36 months despite high prescribed doses of levothyroxine. Much to our surprise, all 3 patients had low or low-normal TSH levels at baseline in the absorption test, compared to levels of more than 40 mIU/mL 3 to 8 weeks before the test. Furthermore, the baseline levels of FT3 and FT4 were high or high normal, indicating that these patients had started taking their levothyroxine prior to the absorption test. The decision to perform a levothyroxine absorption test may have motivated the patients to take their medication. We are unaware of previously published cases describing this phenomenon. In all 3 cases, subsequent TSH levels normalized after decreasing the levothyroxine dose.
Levothyroxine absorption takes place primarily in the jejunum and ileum of the small intestine. Approximately 80% of an orally administered dose is absorbed in the fasting state (2, 3). Serum levels of levothyroxine are at or near their peak 2 hours after administration of an oral dose (7-14). Typical levothyroxine doses in hypothyroidism are 1.5 to 1.6 mcg/kg/day (8, 15). Doses greater than 300 mcg/day are rarely required and should prompt consideration of nonadherence or malabsorption.
There are several possible explanations for higher than typical levothyroxine requirements, including decreased gut absorption, increased metabolism, and nonadherence. Decreased gut absorption is observed in any condition that causes malabsorption, such as celiac disease, jejuno-ileal bypass procedures, severe hepatic cirrhosis, and congestive heart failure (3, 16, 17). Several drugs impair intestinal absorption of the levothyroxine including sucralfate, calcium carbonate, ferrous sulfate, and cholestyramine (2, 17). Drugs such as carbamazepine, phenytoin and phenobarbital increase the metabolism of levothyroxine, leading to higher dose requirements (2). All of these possibilities should be considered in the evaluation of a patient with an apparently high levothyroxine requirement. Before performing relatively expensive and burdensome testing for causes of malabsorption, one should consider levothyroxine absorption testing to rule out nonadherence.
Multiple protocols for clinical levothyroxine absorption testing have been published. While almost all of these protocols involve oral administration of 1000 mcg of levothyroxine, they vary in duration from 4 to 24 hours (3, 6-14, 18, 19). Herein, we describe the successful completion of levothyroxine absorption testing over 2 hours to rule out malabsorption in 3 patients. Additional studies are needed to confirm the validity and safety of rapid levothyroxine absorption testing.
In conclusion, levothyroxine absorption testing over 2 hours may offer a more rapid alternative to the commonly used longer protocols to evaluate levothyroxine absorption. Scheduling a levothyroxine absorption test may induce some patients to start adhering to levothyroxine therapy prior to the test.