1. Background
Calcipherol, also known as vitamin D, is a vital lipid-soluble vitamin in the body, helping the growth and development of bones by inducing phosphorus and calcium absorption by the intestine and decreasing calcium secretion by the kidneys. It also plays a role in gene translation in the process of cell growth (1, 2).
Sunlight, as the best source of vitamin D, induces the production of this vitamin in the skin. Direct sun radiation on the face and arms for 5 - 30 minutes can produce about 1,000 units of vitamin D, which meets daily requirements. Fish liver oil (consumed as a drug), eggs, butter, milk, and fatty fish, such as sardines, and vitamin D-enriched milk are other convenient sources of this vitamin. The quality of social life in past decades has made people feel less sunlight on their skin than before (2-4).
Predisposing factors of vitamin D deficiency are pregnancy; aged less than 5 and more than 65 years; insufficient sunlight exposure; colored skin; certain hepatic, renal, or gastrointestinal diseases; and inadequate vitamin D in the diet (1, 3).
Vitamin D deficiency in children has several adverse effects and presentations including rickets, walking alteration, tooth growth disorders, irritability, cramps or muscle spasms, seizures, and respiratory disorders. It is also known as a predisposing factor for infection, hypertension, and psychological disorders. Vitamin D deficiency has an adverse effect on the process of osteogenesis, resulting in deformity and bowing of the long bones, known as rachitisme in children and osteomalacia in adults (1, 5). Cardiomyopathy may also be seen in severe cases of vitamin D deficiency (3, 6). To prevent such problems, the most important preventative factor is to detect the deficiency at an early stage and prescribe vitamin D-containing supplements.
The aim of the present study was to assess vitamin D levels in children younger and older than 2 years referred to the hospital and to evaluate the necessity and effectiveness of prescribing supplements to these age groups. No similar study has been conducted previously in this age group in Iran.
2. Objectives
To investigate the vitamin D status in children younger and older than 2 years and determine the necessity of prescribing vitamin D supplements
3. Patients and Methods
Three hundred healthy children who attended the pediatric clinic of Baqiyatallah hospital in Tehran for routine checkups were enrolled in this study. Children with complaints of musculoskeletal pain, endocrine or infectious diseases, chronic kidney disease, or evidence of malnutrition were excluded from the study. Children with underlying diseases, such as renal and hepatic disorders, and those with a history of taking antiepileptic drugs were also excluded.
The parents were asked to complete a questionnaire, which included questions on demographics; annual family income (to assess their socioeconomic status); consumption of supplements, mother’s milk, and dairy; and duration of direct sunlight exposure. Blood levels of vitamin D, calcium, and phosphorus were then measured. All the laboratory parameters were measured using the same kit (Liuison, Diasorin Inc.), with the chemiluminescense method. Based on the level of vitamin D, it was classified as: deficiency (less than 30 ng/mL) or normal (more than 30 ng/mL) (7).
The assessment of dairy consumption was qualitative. Daily consumption of two glasses of milk or one glass, together with an adequate amount of other dairy products, such as cheese or ice cream, was considered sufficient. An appropriate amount of sunlight exposure was considered 1.5 hours per week (8).
All the parents were asked to sign an informed consent form, and they were informed that they could leave the study at any time. This study was approved by the ethics committee of Baqiyatallah University of Medical Sciences. All the personal data remained anonymous.
The data were analyzed using the statistical package for social sciences (SPSS), version 16 (SPSS Inc. Chicago, IL, USA) for Windows. Quantitative variables are presented as means and standard deviations. Qualitative variables are expressed as percentages. A Chi-square test was used to compare categorical variables. A P value of less than 0.05 considered statistically significant.
4. Results
The final study consisted of 286 (140 males and 146 females) individuals, with a mean age of 4.46 ± 2.82. Table 1 summarizes the demographic characteristics of the subjects. The mean vitamin D level of the study group was 20.08 ± 15.27 ng/mL. In males, the mean vitamin D level was 20.70 ± 14.85 ng/mL, and it was 20.98 ± 15.27 ng/mL in females. There was no significant association between the vitamin D level and gender (P = 0.75).
| Vitamin D Deficient (N = 218) | Normal Vitamin D Level (N = 68) | P Value | |
|---|---|---|---|
| Age | 5.09 ± 2.82 | 2.58 ± 1.88 | 0.001 |
| Gender | |||
| Male, n (%) | 107 (50) | 33 (48.5 ) | 0.16 |
| Female, n (%) | 111 (50) | 35 (51.05) | |
| Low socioeconomic level, n (%) | 72 (33) | 22 (32.4) | |
| High socioeconomic level, n(%) | 146 (6.9) | 46 (67.6) | 0.91 |
| Vitamin D level, ng/mL | 13.80 ± 7.38 | 44.02 ± 0.43 | 0.0001 |
| Calcium level, mg/dl | 9.27 ± 0.65 | 9.92 ± 0.67 | 0.22 |
| Phosphorus level, mg/dl | 5.19 ± 0.74 | 5.06 ± 0.68 | 0.43 |
| Alkaline-phosphatase level, mg/dl | 421.58 ± 188.64 | 557.59 ± 169.54 | 0.7 |
aValues are expressed as mean ± SD or No. (%).
Table 1 presents the laboratory data. The mean calcium level was 9.77 ± 0.65. In children with severe vitamin D deficiency (less than 10 ng/mL), the mean calcium level was 9.21 ± 0.63, which was not significantly different from the level in the normal vitamin D group (P = 0.22). The phosphorus level was 5.09 ± 0.7 in the case individuals. There was no significant correlation between the phosphorus level and vitamin D level in either group (P = 0.43). Levels of alkaline phosphatase were also the same in the two groups (P = 0.7).
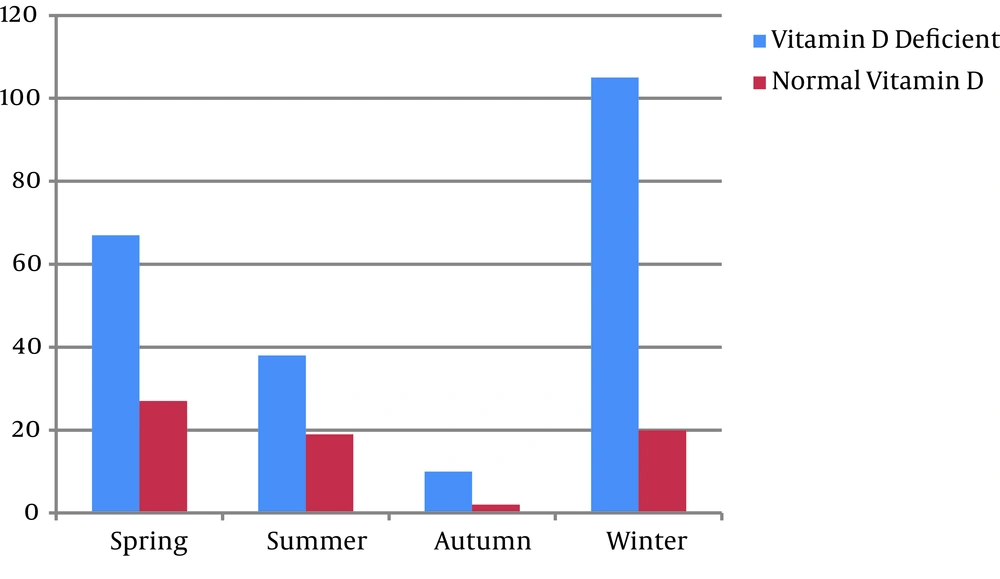
As shown in Table 2, based on eta squared, the vitamin D level was associated with the seasons (0.6). In a post hoc test, there was a significant difference between the winter and summer levels of vitamin D (P = 0.005).
| Season | Vitamin D Deficiency (N= 218) | Normal Vitamin D Level (N=68) | Mean Vitamin D level, ng/mL | P Value |
|---|---|---|---|---|
| Spring | 67 (30.7) | 27 (39.7) | 22.11 ± 14.63 | 0.005 |
| Summer | 38 (16.5) | 19 (27.9) | 29.37 ± 18.74 | 0.005 |
| Fall | 10 (4.6) | 2 (2.9) | 20.44 ± 16.36 | 0.005 |
| Winter | 105 (48.2) | 20 (29.4) | 17.21 ± 13.61 | 0.005 |
aValues are expressed as mean ± SD or No. (%).
In the study, 94 (32.9%) individuals had a low socioeconomic status, and the socioeconomic status of 192 (67.1%) individuals was average or high. The mean vitamin D level in those with a low socioeconomic was 18.27 ± 14.61 ng/mL, whereas it was 21.39 ± 15.15 ng/mL in those with an average or a high socioeconomic status. There was no significant correlation between the vitamin D level and socioeconomic status (P = 0.918).
In the study group, 154 (53.8%) children had direct sunlight exposure of less than 1.5 hours per week, and 132 (46.2%) had sunlight exposure of more than 1.5 h, and the mean vitamin D level was 17.23 ± 13.76 ng/mL and 24.07 ± 15.67 ng/mL, respectively. There was a significant association between vitamin D levels and the duration of direct exposure to sunlight (P = 0.001).
Mother’s milk was consumed by 132 (60%) children in the vitamin D-deficient group and by 60 (88.2%) children in the normal vitamin D group, who had a mean vitamin D level of 19.45 ± 11.18 ng/mL. Eighty-six (40%) children with vitamin D deficiency and 8 (11.8%) children with normal vitamin D levels were fed powdered milk. The mean vitamin D level of these children was 8.6 ± 4.04 ng/mL (P = 0.001). A total of 110 (38.46%) subjects had sufficient dairy consumption, with a mean vitamin D level of 14.89 ± 11.66 ng/mL, whereas those with insufficient dairy consumption had a mean vitamin D level of 13.46 ± 10.23 (P > 0.05).
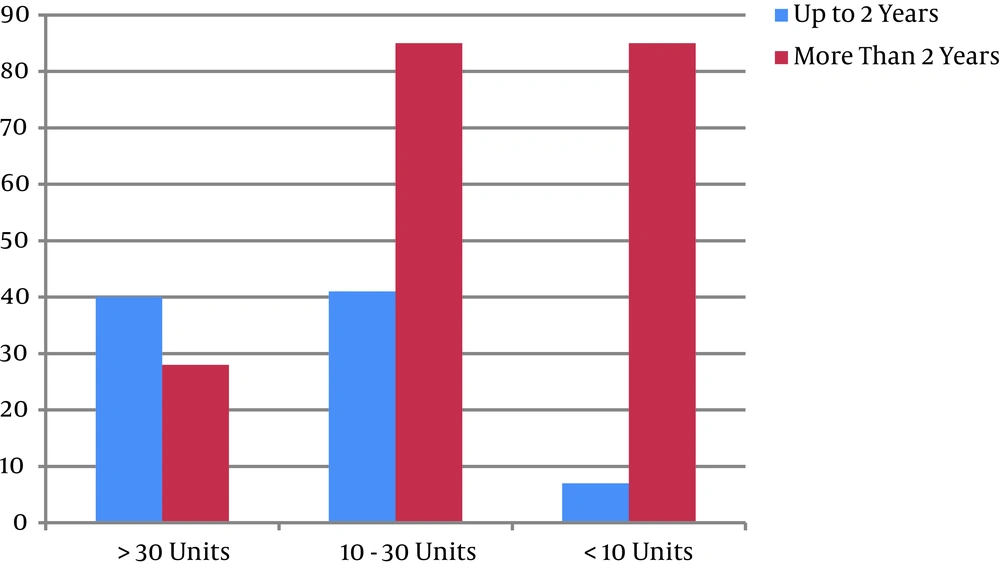
In the present study, 88 (30.8%) children were younger than 2 years, and 198 (69.2%) were older than 2 years. The level of vitamin D was significantly different between the two age groups (P = 0.0001) (Table 3, Figures 1 and 2).
Consuming vitamin D supplements was significantly effective in increasing vitamin D levels in the children older than 2 years Twenty-four (12.12%) children who consumed vitamin D supplements had a mean vitamin D level of 31.13 ± 5.9 ng/mL, whereas the level was 14.05 ± 8.09 ng/mL in the children who did not consume supplements (P = 0.0001).
| Level of Vitamin D | Younger Than 2 Years (N = 88) | Older Than 2 Years (N = 198) | P Value |
|---|---|---|---|
| Mean level, ng/mL | 29.71 ± 14.42 | 17.11 ± 14.02 | 0.0001 |
| > 30 ng/mL (Normal) | 40 (45.5) | 28 (14.1) | 0.0001 |
| 10 - 30 ng/mL (Insufficient) | 41 (46.6) | 85 (42.9) | 0.001 |
| < 10 ng/mL (deficient) | 7 (7.9) | 85 (42.9) | 0.0001 |
aValues are expressed as mean ± SD or No. (%).
5. Discussion
Based on the significantly higher level of vitamin D among those who consumed supplements and the lower level of vitamin D in the children older than 2 years, the consumption of vitamin D supplements is highly recommended in this age group. In Iran, children younger than 2 years routinely receive 400 units of vitamin D daily. This may be the main cause of the higher levels of vitamin D in this age group in the present study.
In the current study, there was no significant difference in the vitamin D levels of males and females among children aged 1 - 10 years, and socioeconomic status was not significantly associated with vitamin D levels. Regarding socioeconomic status and the significant association between the duration of sunlight exposure and high vitamin D levels in the present study, it can be concluded that the vitamin D level is more associated with direct contact with sunlight rather than personal diet. The findings of the present study also demonstrated that vitamin D levels were higher in summer than in winter. Thus, vitamin D supplements are more necessary in the winter, especially for those older then 2 years.
Significant seasonal variations were reported in vitamin D levels among people aged 10 - 70 years old living in Sari, Iran (9). In that study, the prevalence of vitamin D deficiency was 87.5% in winter and 78.6% in summer (P < 0.05). A study of ethnic aspects of vitamin D deficiency concluded that a major part of production and saving of vitamin D is related to sunlight exposure and that vitamin D deficiency was more frequent in countries with high geographic latitudes (10). However, the same study found no significant difference in 25-hydroxyvitamin D level between people with more sunlight exposure and those with less, especially in areas with abundant sun. Vitamin D deficiency is common in Iran, which is located at relatively high latitude over a tropical line.
In a study of 1,111 school-aged children, there was a high prevalence of vitamin D deficiency (86%) in both genders but especially in girls (11), in contrast to the findings of the present study. The previous study also mentioned a direct correlation between vitamin D levels and sun exposure (11). A high prevalence of vitamin D deficiency was also reported in children of preschool age living in Isfahan, Iran. The duration of sunlight exposure and daily intake of vitamin D were reported to have positive effects on vitamin D levels (12). The prevalence of vitamin D deficiency was reported to be 53.6% in females and 11.3% in male children and adolescents in Tehran (13), a finding that was in concordance with a similar study in North Khorasan, Iran (14) but in contrast to that of the present study as regards gender and vitamin D levels. A high prevalence of vitamin D deficiency was found in children between 1 and 16 years, and supplements were suggested (15), which is in agreement with the findings of the current study. A study of the frequency of vitamin D deficiency in children concluded that the mean level of vitamin D was significantly higher in males than in females (16), in common with the findings of the present study. However, that study did not find any significant seasonal variation in vitamin D levels, unlike the current one.
In accordance with the results of the present study, previous research concluded that prophylactic vitamin D was necessary for children of school age (17). Furthermore, children aged between 1 and 3 years who did not take vitamin D supplements were found to have insufficient vitamin D levels (18).
In the present study, the levels of calcium, phosphorus, and alkaline phosphatase were not significantly different between the children with vitamin D deficiency and those with normal vitamin D levels. A previous study of the status of vitamin D in healthy schoolchildren detected no significant difference between children with normal, insufficient, and deficient levels of vitamin D in calcium, phosphorus, and alkaline phosphatase levels (19).
We found that children older than 2 years had lower vitamin D levels in comparison with those younger than 2 years. We also found that children who consumed vitamin D supplements had higher levels of vitamin D. Sunlight exposure was effective in increasing vitamin D levels. Thus, prescribing vitamin D-containing supplements to children older than 2 years and those who have low direct sunlight exposure may be beneficial, especially in cold seasons. Further studies are needed to evaluate the role of vitamin D supplements in normalizing vitamin D levels in these age groups, as well as the role of sunlight exposure.