1. Introduction
Thyroid nodules disease is one of the most common endocrine disorders. Thyroid nodules are commonly incidental findings (1-3), following noninvasive methods such as radionuclide thyroid scans and thyroid ultrasound. Fine needle aspiration (FNA) is a simple, reliable, inexpensive and generally safe procedure in the diagnosis of thyroid nodules (2, 4, 5). However, like other mini-invasive procedures, FNA may cause several, usually mild complications (2). In this paper, for the first time to our knowledge, we report a severe retropharyngeal cellulitis probably due to the procedure.
2. Case Presentation
We report a case of 35-year-old female presented to an emergency room with a 3-day history of hoarseness, laryngeal stridor and dyspnea without fever, after execution of FNA.
Recently, thyroid ultrasound showed a right-side, solid, hypoechoic nodular formation with areas of intraparenchymal liquefaction (30 × 20 mm): overall size 51 mm (maximum diameter). Under prescription from her regular doctor, thyroid function and calcitonin were evaluated (all within the normal range). The patient was in her usual health until the first diagnostic cytology examination with FNA, which occurred 3 days before admission. After the procedure, the patient felt her voice became hoarse and 1 day before presentation began to have dyspnea, without fever. It had become difficult for her to swallow solids and she felt as if food was sticking in her throat. The patient's history included non-insulin-dependent (type 2) diabetes mellitus diagnosed 3 years ago and first degree obesity (BMI 31 kg/m2). Medication was only metformin (1.5 g every day). She had no known allergies, did not smoke, drink alcohol or use illicit drugs and there was no history of unusual ingestions.
On examination, the patient appeared obese. Her temperature was 37.3°C, the blood pressure 120/70 mm Hg, the pulse 78 beats per minute, and the respiratory rate 18 breaths per minute.
Oxygen saturation was reduced (88% while she was breathing ambient air); therefore, she required oxygen therapy without intubation. The abdomen was without tenderness or distention, with normal bowel sounds. The patient had strong pain on superficial palpation on the anterior neck region.
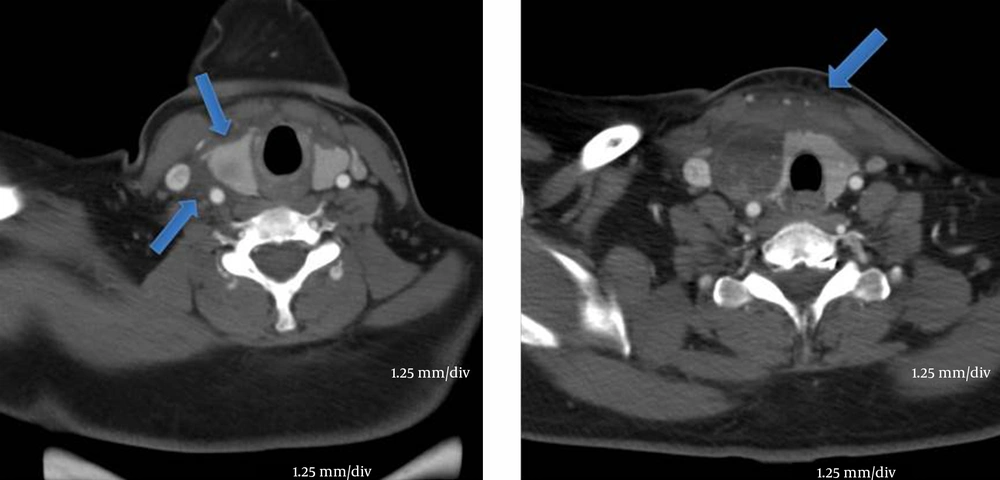
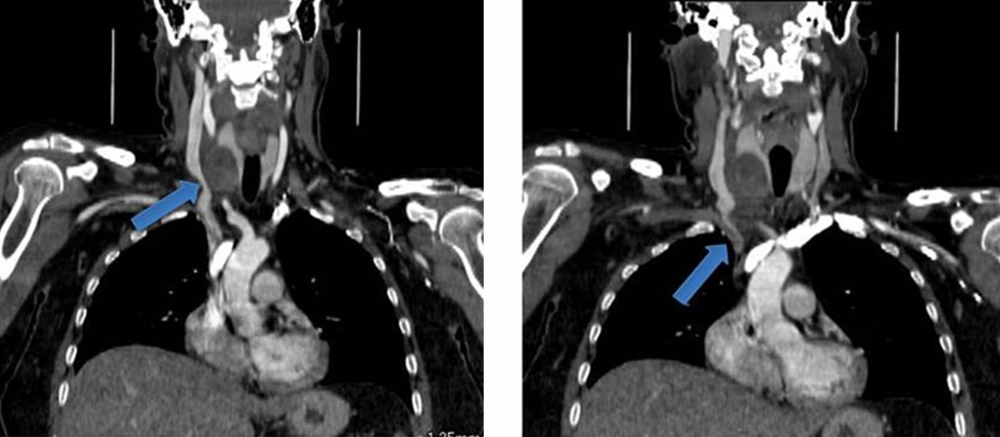
The emergency department carried out blood tests, which highlighted leukocytosis with neutrophilia and elevation of erythrocyte sedimentation rate (92 mm/hr). Computed tomography (CT) of the neck and mediastinum, without the administration of intravenous or oral contrast material, revealed a severe cellulitis framework with involvement of the laterocervical neck area and, in particular, the invasion of retropharynx and upper mediastinum (Figures 1 and 2). In the right side of the thyroid, it confirmed the existence of right nodular formation recently examined by FNA (Figure 2). Probably due to compressive phenomena, a mild reduction of oxygen saturation was recorded, though it did not require intubation and/or oxygen therapy. After the infectious disease specialist’s consultation, the patient was admitted to the hospital. Antibiotic therapy with meropenem plus teicoplanin and anti-inflammatory therapy with methylprednisolone were started. Furthermore, blood cultures were negative.
After 2 days of therapy, a progressive improvement of the clinical picture was noted and by the fourth day, ultrasound reassessment of the neck area did not reveal any more marks of cellulitis. The patient was discharged home on the fifth day on metformin, steroid and antibiotic therapy.
The result of cytological examination detected a suspicious framework for malignant follicular proliferation (TIR 3b), therefore a subtotal thyroidectomy was performed after 20 days.
The intervention did not involve any complications and a histopathological examination showed a benign follicular lesion framework. The patient thus began a substitution therapy with levothyroxine (1.6 g/kg/day).
3. Discussion
To our knowledge, this is the first case report to deal with a retropharyngeal cellulitis as a potentially severe complication of FNA. Retropharyngeal cellulitis represents an infection in one of the necks deep spaces. It is rare in adults and usually occurs as a result of local trauma, such as instrumental procedures, foreign body ingestion (fishbone) or in the particular context of an associated disease (6, 7). Retropharyngeal cellulitis requires prompt diagnosis and early management (8). Retropharyngeal cellulitis can be caused by many organisms such as aerobic organisms (beta-hemolytic Streptococci and Staphylococcus aureus), anaerobic organisms (species of Bacteroides and Veillonella), or Gram-negative organisms (Haemophilus parainfluenzae and Bartonella henselae) (9).
The retropharyngeal cellulitis high mortality rate is due to its association with airway obstruction, mediastinitis, erosion into the carotid artery, aspiration pneumonia, jugular venous thrombosis, necrotizing fasciitis and sepsis (10). A German study on 234 adults with deep space infections of the neck shows a mortality rate of about 2.6% (11). The main cause of death was sepsis with multi organ failure. Diagnostic criteria of retropharyngeal cellulites involve laboratory findings and radiological examinations. Laboratory findings usually support the infective origin, demonstrating a slight leukocytosis with neutrophilia, and augmentation of inflammatory indexes. Radiological examinations such as CT scan and magnetic resonance imaging (MRI) scan provide assessment of the extent of the involvement, topographical limits, detection of abscesses, and presence of air within tissues (12).
Thyroid nodules FNA became one of the most helpful, reliable and accurate tools in diagnosis of thyroid pathology. Thyroid nodules, which should be taken into account for FNA include palpable, solitary nodule or nodules associated with particular clinical features (palpable or ultrasonographically abnormal cervical lymph nodes with fast growth). Other features of nodules that should also be the subject of FNA are microcalcification, rounded shape, predominantly solid composition, dominant or atypical nodules in multinodular goiter (4). The most common complications after FNA are minor hematomas, with a morbidity that is usually negligible. Massive hematomas are rare, but sometimes life-threatening (13).
Another complications reported in the literature are local pain and/or discomfort during or after FNA, transient and well-tolerated by the patient. Moreover, other rare complications have been reported: one case of cervical neuritis following a post- FNA hematoma; one case of pseudoaneurysm (puncturing of the superior thyroid artery) and one of subendothelial carotid hematoma along with several cases of acute or delayed transient swelling of the entire thyroid gland (5).
There are various mechanisms that protect against thyroid infection, even in immunocompromised patients, including rich lymphatic drainage, the protective capsule surrounding the gland and high iodine content (5). It has been described in some cases of thyroid abscess, one of them represented by an acute suppurative thyroiditis (14). Recurrent laryngeal nerve injury, vasovagal reactions, persistent discharging sinus at the needle insertion site and destructive thyrotoxicosis have also been rarely reported following FNA (5).
It has been well demonstrated that patients with diabetes mellitus have infections more often than those without diabetes mellitus. The course of the infections is also more complicated in this patient group. Defects in immunity may represent one of the possible causes of this increased prevalence of infections. Besides some decreased cellular responses in vitro, no disturbances in adaptive immunity in diabetic patients have been described. Low complement factor 4, decreased cytokine response after stimulation in humoral innate immunity have been described in diabetic patients. However, the clinical relevance of these findings is not clear. Concerning cellular innate immunity most studies show decreased functions of diabetic polymorphonuclear cells and diabetic monocytes/macrophages compared to cells of controls. Moreover, some microorganisms become more virulent in a high glucose environment. An increased adherence of microorganisms to diabetic compared to nondiabetic cells could be another mechanism which can lead to the increased prevalence of infections in diabetic patients (15). Anyway, as many diabetic subjects undergoes FNA without any complication, diabetes seems to not justify the onset of the severe retropharyngeal cellulitis.
We undertook the FNA in accordance with the international guidelines (1). The patient was in a supine position but with the neck extended to facilitate access to the thyroid. The patient was instructed not to swallow or speak during the insertion of the needle. We located the lesion with a high-resolution (10 MHz) linear-array transducer, after which we cleaned the skin with a 2% alcohol solution. We performed the procedure using nonsterile ultrasound gel on the linear transducer covered with a non-sterile material, placed over the head.
Cellular material was obtained by the cutting action of the trailing edge of the needle, retained in the needle lumen by forward motion and capillary tension, without aspiration by needle alone (25 gauge needles). The needle oscillated back and forth approximately three times per second. In total we performed three passes in several places within the nodule, and between each pass, we applied a local pressure for an appropriate hemostasis. The collected material was placed on glass slides, smeared, and fixed with alcohol (16, 17).
3.1. Conclusions
For the first time to our knowledge, we have reported a severe retropharyngeal and upper mediastinum cellulitis, probably due to the FNA procedure in an immunocompetent young woman.