1. Background
Hypertension is a well-known factor for cardiovascular complications (1). A worldwide report in 2000 showed that over 26% of individuals of all ages have hypertension, a prevalence likely to reach 29% by 2025 (2). Although hypertension has attracted much attention due to its high morbidity and mortality, complications of high blood pressure occur at lower values than those that are currently used to be classified as hypertension (3). In 2003, a new classification of blood pressure status, termed pre-hypertension, was introduced and was defined as having either a systolic blood pressure (SBP) of 120 - 139 mmHg and/or diastolic blood pressure (DBP) of 80 - 89 mmHg in the absence of antihypertensive medications (4). This condition is associated with an increased risk of cardiovascular and cerebrovascular diseases as well as total mortality (5). Pre-hypertension is highly prevalent in Iran (about 46% of Iranians aged 25 - 64) and considering its high progression rate of 56% over seven years to hypertension, it predicts an alarming trend (6, 7). The data highlights the need for identifying the predisposing factors of pre-hypertension in Iranian populations.
The associations of pre-hypertension with different socio-behavioral and cardio-metabolic factors have been investigated previously. Although among the socio-demographic factors, there is a consensus on the positive association of age and pre-hypertension (7-9), there are conflicting results regarding the association of marital status and education with pre-hypertension. Despite some studies reporting that marital status does not have a significant association with pre-hypertension (7), being married was found to be associated with a lower risk of pre-hypertension in others (8, 10). Moreover, several studies have reported the protective effect of education on pre-hypertension (9, 11); however, a study in Iran revealed that educational attainment does not have any significant association with pre-hypertension (7). Among behavioral factors, physical activity is reported to have no association with pre-hypertension in men or women (11); yet interestingly, a sedentary lifestyle was found to be negatively associated with pre-hypertension in men but not women (12). On the other hand, poor dietary patterns, serum triglyceride levels (TG), and waist circumference (WC) are known to be predisposing factors of pre-hypertension (11, 13, 14).
Although it has been extensively shown that men are at a higher risk of developing pre-hypertension (7-10), there are relatively few studies investigating gender differences in assessing risk factors of this disorder (11). Limited socio-behavioral and cardio-metabolic factors have been investigated in most previous studies, most of which have applied first generation of multivariate techniques, which preclude a holistic approach to identify mediators of the association of each factor with pre-hypertension. As one of the first investigations, using a statistical approach of structural equation modeling (SEM), the current study aimed to examine sex-specific models of factors related to pre-hypertension, based on the available literature. Using SEM allowed us to investigate different direct and indirect associations of socio-behavioral and cardio-metabolic factors with pre-hypertension to provide a comprehensive view of their associations and interactions in a non-hypertensive population of Tehranian adults.
2. Methods
2.1. Study Design and Participants
The Tehran Lipid and Glucose Study (TLGS) is a large scale community based prospective study performed on a representative sample of residents of district-13 of Tehran (15). A total of 6016 adults (≥ 20 years old), who participated in the fourth phase of TLGS, between 2009 and 2011, were included in this study. Of these, after excluding 1104 individuals with hypertension and 272 individuals with extreme or missing date values 4640 individuals were considered for the final analysis. Remaining participants had completed data on socio-demographic factors, leisure time physical activity, dietary patterns, and cardio-metabolic risk factors. They signed a written consent form and the Ethics Committee of the Research Institute for Endocrine Sciences approved this study, which has been conducted in accordance with the 1964 Helsinki declaration.
2.2. Definitions and Measures
Modifiable Activity Questionnaire (MAQ) was used to assess information on leisure time physical activity and MET-min/day calculation (16). Finally, five groups were defined for leisure time physical activity; one group consist of those who had no leisure time physical activity and four groups were categorized, according to quartiles of daily calculated MET for leisure time physical activity. A validated 168-item semi-quantitative food frequency questionnaire (FFQ) (17) was used by trained dietitians to collect dietary data of participants. The usual intake (portion size) of each food item was obtained based on a daily, weekly, monthly and yearly basis during the last year, then it was converted to daily intakes (gram). Exploratory Factor Analysis (EFA) was used to detect dietary patterns using the information of 23 food groups. Blood pressure was measured twice using a standardized mercury sphygmomanometer on the right arm, after a 15 min rest in a sitting position; the mean of these two measurements was considered as the subject’s blood pressure. Pre-hypertension was defined as having either a SBP of 120 - 139 mmHg and/or DBP of 80 - 89 mmHg in the absence of antihypertensive medication (4).
2.3. Statistical Analysis
Mean ± SD for continuous variables and the frequency (percent) distribution of categorical data for responders, with and without pre-hypertension have been reported. To compare continuous and categorical data between those with and without pre-hypertension, independent sample t-test and Chi-Square test were used, respectively. The latent constructs of “poor dietary pattern” and “healthy dietary pattern” were explored separately on 50% randomly selected responders, using EFA. To estimate factor loadings of observed variables (food groups) for each latent construct, Principal component analysis (PCA) with orthogonal varimax rotation was conducted.
2.4. The Measurement Model or CFA
To verify the latent constructs of “poor dietary pattern” and “healthy dietary pattern”, Confirmatory Factor Analysis (CFA) was used to examine the hypothesized associations between a set of food groups. The food groups had been already explored by EFA and those who had absolute loadings ≥0.30 remained in the CFA of “poor dietary pattern” or “healthy dietary pattern” constructs.
2.5. The Structural Model or SEM
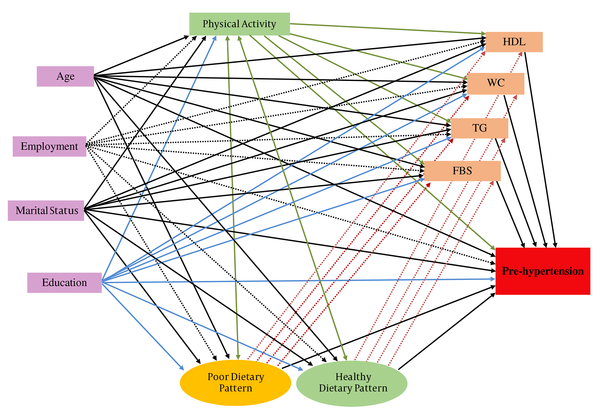
The socio-demographic characteristics were considered as exogenous variables and behavioral factors including leisure time physical activity, dietary patterns, and cardio-metabolic risk factors including HDL, FBS, TG, and WC were considered as mediators. The presence of pre-hypertension (yes/no) was an endogenous variable (Figure 1). Using the structural model, gender-specific relations between the above-mentioned factors were examined.
The structural model: Testing the association of socio-behavioral and biochemical factors with pre-hypertension. Age, employment and marital status and education are exogenous independent variables. Behavioral factors including physical activity and dietary patterns are mediators and affect cardio-metabolic risk factors. Cardio-metabolic risk factors as another set of mediators affect on pre-hypertension. Pre-hypertension status considered as final dependent variable. Abbreviations: FBS, fasting blood sugar; HDL, high density lipoprotein; TG, triglycerides; WC, waist circumference.
All of the SEM models were fitted by the Maximum Likelihood Estimation method; model fit measures could then be obtained to assess how well the proposed models captured the covariance between all the measures in the models. Some of the model fit indices assessed included χ2, the ratio of the χ2 to degrees of freedom (CMIN /DF), the Comparative Fit Index (CFI), the Root Mean Square Error of Approximation (RMSEA), the normed fit index (NFI), goodness of fit index (GFI), and incremental fit index (IFI); CFI ≥ 0.90 and the RMSEA ≤ 0.08 are generally considered to represent a reasonable model fit to the data. We used SPSS v20 for data management, descriptive statistics, and comparisons as well as Amos v20 software for CFA and to test the structural model. P-values < 0.05 were considered statistically significant.
3. Results
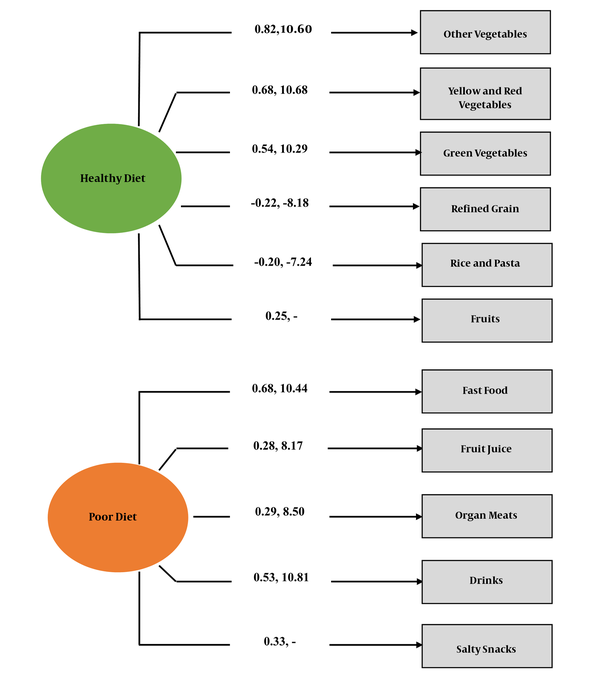
The mean age of participants was 38.61 ± 12.14 years and 56.6% of them were female. More than one third of studied participants had pre-hypertension (35.4%) with significantly higher prevalence in males compared to females (46.5% vs. 26.9%; χ2 = 190.7, P < 0.001). Further descriptive statistics of observed variables, comparing those with and without pre-hypertension, are presented in Table 1. As a whole, age, education, marital, and employment status were significantly associated with pre-hypertension, however, further analysis by sex groups indicated that education and employment status were not significantly associated with pre-hypertension in males; WC and cardio-metabolic risk factors were significantly related to pre-hypertension in both sexes (P < 0.001). The distribution of pre-hypertension did not differ significantly with varying levels of leisure time physical activity in both sexes. Based on eigenvalues > 2, two dietary patterns were detected using EFA including, 23 food groups of 2320 subjects. A total of 42% of total variance were explained by two detected healthy and poor dietary patterns. The factor loadings of each food group can be found in the online supplementary material. The CFA was conducted on the other half of the subjects (n = 2320) (Figure 2). Goodness of fit indices for evaluating CFA of dietary pattern constructs are reported below Figure 2. All of them are within acceptable levels.
χ2 = 118.07, df = 33, χ2/df = 3.58, RMSEA = 0.033, RMR = 0.03, GFI = 0.99, CFI = 0.99, IFI = 0.97, NFI = 0.98, TLI = 0.97. Fit indices of the CFA model display appropriateness of measurement model of dietary patterns. The standardized factor loadings and related t statistics to evaluate the explained variances of food groups reported on path ways. All factor loadings are significant for healthy and poor dietary patterns (p < 0.001). According to factor loadings, healthy dietary pattern is defined as higher vegetable (yellow, red, green and other vegetables), higher fruits, lower refined grain and lower rice/pasta. Poor dietary pattern explained by high intake of fast foods, fruit juice, organ meats, drinks and, salty snacks. Abbreviations: CFA, confirmatory factor analysis; RMSEA, root mean square error of approximation; RMR, root mean square residual; GFI, goodness of fit index; CFI, comparative fit index; IFI, incremental fit index; NFI, normed fit index; TLI, Tucker-Lewis Index.
| Total (n = 4640) | Male (n = 2014) | Female (n = 2626) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Non pre-hypertensive (N = 2998) | Pre-hypertensive (N = 1642) | P Value | Non pre-hypertensive (N = 1078) | Pre-hypertensive (N = 936) | P Value | Non pre-hypertensive (N = 1920) | Pre- hypertensive (N = 706) | P Value | |
| Age | 36.63 ± 11.20 | 42.21 ± 12.92 | < 0.001 | 37.90 ± 12.13 | 42.05 ± 13.63 | <0.001 | 35.91 ± 10.59 | 42.43 ± 11.92 | < 0.001 |
| Education | |||||||||
| Elementary | 535 (57.8) | 391 (42.2) | < 0.001 | 199 (53.5) | 173 (64.5) | 0.15 | 336 (60.6) | 218 (39.4) | < 0.001 |
| Secondary school | 1422 (64.5) | 781 (35.5) | 486 (51.5) | 458 (48.5) | 936 (74.3) | 323 (25.7) | |||
| Undergraduate | 941 (70.1) | 401 (29.9) | 339 (57.3) | 253 (42.7) | 602 (80.3) | 148 (19.7) | |||
| Postgraduate degree | 99 (58.6) | 70 (41.4) | 54 (50.5) | 53 (49.5) | 45 (72.6) | 17 (27.4) | |||
| Marital status | |||||||||
| Single | 738 (72.1) | 286 (27.9) | < 0.001 | 326 (62.5) | 196 (37.5) | < 0.001 | 412 (82.1) | 90 (17.9) | < 0.001 |
| Married | 2259 (62.5) | 1357 (37.5) | 752 (50.4) | 741 (49.6) | 1507 (71.0) | 616 (29.0) | |||
| Employment | |||||||||
| Unemployed | 1684 (65.5) | 776 (31.5) | < 0.001 | 199 (49.5) | 203 (50.5) | 0.07 | 1485 (72.2) | 573 (27.8) | 0.04 |
| Employed | 1313 (60.2) | 867 (39.8) | 879 (54.5) | 734 (45.5) | 434 (76.5) | 133 (23.5) | |||
| FBS, mmol/L | 5.08 ± 0.52 | 5.29 ± 0.61 | < 0.001 | 5.18 ± 0.56 | 5.35 ± 0.66 | < 0.001 | 5.02 ± 0.49 | 5.20 ± 0.53 | <0.001 |
| TG, mmol/L | 1.30 ± 0.72 | 1.68 ± 0.89 | < 0.001 | 1.51 ± 0.85 | 1.83 ± 0.95 | < 0.001 | 1.18 ± 0.60 | 1.49 ± 0.76 | <0.001 |
| WC, m | 0.88 ± 0.11 | 0.96 ± 0.11 | < 0.001 | 0.91 ± 0.10 | 0.97 ± 0.11 | <0.001 | 0.86 ± 0.11 | 0.93 ± 0.11 | <0.001 |
| HDL, mmol/L | 1.27 ± 0.29 | 1.19 ± 0.28 | < 0.001 | 1.12 ± 0.24 | 1.09 ± 0.23 | <0.001 | 1.36 ± 0.29 | 1.32 ± 0.29 | <0.001 |
| Leisure time physical activity | |||||||||
| No | 1439 (65.4) | 761 (34.6) | 0.38 | 494 (55.4) | 398 (44.6) | 0.47 | 945 (72.2) | 363 (27.8) | 0.17 |
| Q1 | 388 (63.7) | 221 (36.3) | 149 (51.4) | 141 (48.6) | 239 (74.9) | 80 (25.1) | |||
| Q2 | 429 (66.5) | 216 (33.5) | 158 (54.7) | 131 (45.3) | 271 (76.1) | 85 (23.9) | |||
| Q3 | 383 (62.5) | 230 (37.5) | 126 (51.9) | 117 (48.1) | 257 (69.5) | 113 (30.5) | |||
| Q4 | 358 (62.5) | 215 (37.5) | 151 (50.2) | 150 (49.8) | 207 (76.1) | 65 (23.9) | |||
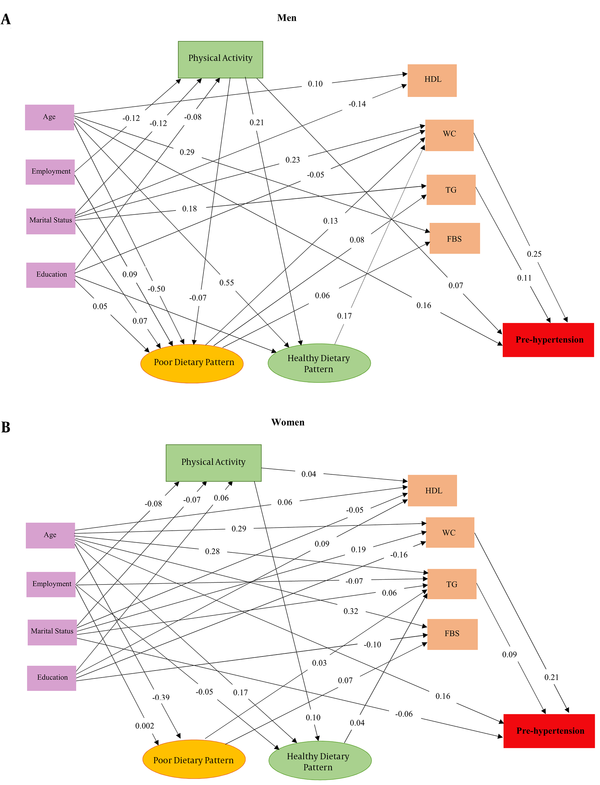
The standardized coefficients and t-statistics for each pathway, indicating the influence of predictors on responses, are shown in men and women separately (Table 2). Among studied cardio-metabolic factors, WC and TG, in both genders (P < 0.01), were directly associated with pre-hypertension. The association between poor and healthy diet with pre-hypertension were indirect in men and women via WC and TG, respectively. Physical activity in men was the only behavioral factor which was found to be directly associated with pre-hypertension (β=0.069, p < 0.01). Among socio-demographic factors, age in both genders (p < 0.01) and marital status, only in women (p < 0.01), showed direct associations with pre-hypertension. As shown in Figure 3, all other associations among socio-demographic factors and pre-diabetes were indirect in both genders, mostly via TG and WC.
| Response | Male | Female | Difference C.R# | ||
|---|---|---|---|---|---|
| Coefficient | C.R | Coefficient | C.R | ||
| Physical Activity | |||||
| Age | -0.051 | -1.75 | 0.014 | 0.59 | 1.70 |
| Employmentb | -0.124 | -5.29** | -0.076 | -3.49** | 1.72 |
| Marital statusc | -0.163 | -5.70** | -0.068 | -3.13** | 2.44* |
| Education | -0.079 | 3.54** | 0.064 | 2.68* | -0.43 |
| Healthy diet | |||||
| Age | 0.549 | 8.77** | 0.168 | 4.36** | -6.95** |
| Employment | -0.002 | -0.04 | -0.047 | -11.11** | -0.51 |
| Marital status | -0.071 | -1.50 | 0.027 | 1.39 | 1.77 |
| Education | 0.183 | 4.69** | 0.029 | 1.52 | -4.20** |
| Physical Activityd | 0.213 | 4.90** | 0.100 | 3.78** | -3.52** |
| Poor diet | |||||
| Age | -0.502 | -10.05** | -0.393 | -11.11** | -0.31 |
| Employment | 0.091 | 3.40** | 0.002 | 4.36** | 1.03 |
| Marital status | 0.067 | 2.10* | 0.001 | 1.52 | -2.04* |
| Education | 0.052 | 2.10* | -0.009 | -0.45 | -1.78 |
| Physical activityc | -0.071 | -2.54* | 0.029 | 1.42 | 2.85** |
| HDL | |||||
| Age | 0.101 | 2.31* | 0.055 | 2.22* | -0.41 |
| Employment | -0.046 | -1.90 | 0.005 | 0.22 | 1.46 |
| Marital status | -0.140 | -4.73** | -0.052 | -2.40* | 1.63 |
| Education | 0.010 | 0.43 | 0.090 | 3.76** | 2.70** |
| Physical activity | 0.027 | 1.10 | 0.044 | 2.24* | 0.82 |
| Poor diet | -0.033 | -1.03 | -0.014 | -0.66 | 0.48 |
| Healthy diet | -0.077 | -1.58 | -0.010 | -0.59 | 0.76 |
| WC | |||||
| Age | 0.008 | 0.18 | 0.290 | 3.53** | 6.83** |
| Employment | 0.031 | 1.29 | -0.025 | -1.33 | -1.84 |
| Marital status | 0.225 | 7.68** | 0.194 | 10.34** | 0.24 |
| Education | -0.051 | -2.11* | -0.160 | -7.76** | -3.88** |
| Physical activity | -0.023 | -0.92 | 0.021 | 1.28 | 1.50 |
| Poor diet | 0.130 | 3.84** | -0.016 | -0.88 | -3.82** |
| Healthy diet | 0.170 | 3.27** | 0.015 | 1.00 | -2.16* |
| TG | |||||
| Age | 0.067 | 1.57 | 0.276 | 12.27** | 3.49** |
| Employment | 0.031 | 1.31 | -0.072 | -3.48** | -2.98** |
| Marital status | 0.184 | 6.31** | 0.062 | 3.00** | -3.98** |
| Education | 0.031 | 1.28 | -0.040 | -1.76 | -2.10* |
| Physical activity | -0.032 | -1.32 | -0.033 | -1.79 | 0.26 |
| Poor diet | 0.083 | 2.56* | 0.030 | 4.44** | -1.96 |
| Healthy diet | 0.008 | 0.17 | 0.040 | 2.39* | 1.00 |
| FBS | |||||
| Age | 0.290 | 6.89** | 0.316 | 14.19** | 0.17 |
| Employment | 0.025 | 1.05 | 0.001 | 0.05 | -0.83 |
| Marital status | 0.038 | 1.34 | 0.015 | 0.75 | -0.71 |
| Education | -0.021 | -0.91 | -0.096 | -4.29** | -2.04* |
| Physical activity | 0.006 | 0.26 | -0.001 | -0.45 | -0.29 |
| Poor diet | 0.062 | 1.98* | 0.065 | 7.53** | -0.50 |
| Healthy diet | 0.059 | 1.27 | -0.015 | -0.91 | -1.56 |
| Pre-hypertension | |||||
| Age | 0.158 | 3.75** | 0.156 | 6.11** | 0.04 |
| Employment | -0.035 | -1.49 | 0.018 | 0.86 | 1.70 |
| Marital status | -0.038 | -1.31 | -0.064 | -3.05** | -0.73 |
| Education | 0.020 | 0.88 | 0.006 | 0.24 | -0.48 |
| HDL | 0.034 | 1.43 | 0.013 | 0.64 | -0.89 |
| WC | 0.245 | 10.27** | 0.213 | 9.35** | -2.31* |
| TG | 0.106 | 4.34** | 0.090 | 4.21** | 0.13 |
| FBS | 0.040 | 1.77 | 0.031 | 1.52 | -0.22 |
| Physical activity | 0.069 | 2.94** | -0.005 | -0.27 | -2.53* |
| Poor diet | 0.051 | 1.63 | 0.022 | 1.05 | -0.97 |
| Healthy diet | -0.018 | -0.38 | 0.015 | 0.95 | 0.84 |
Results of Structural Model: Sex Specific Associations Between Socio-Behavioral, Biochemical Factors and Pre-Hypertensiona
4. Discussion
In this study, WC and TG were the most important factors that were directly associated with pre-hypertension in both genders. Compared to women, the association of WC with pre-hypertension was stronger in men. Abdominal obesity and hypertriglyceridemia have previously been known as factors, which commonly co-occur and increase each other (18): some authors refer to the occurrence of these two factors as “hypertriglyceridemic waist”, which can result in high blood pressure through an atherogenic process (18). In the current study, although we have not investigated the inter-relation of cardio-metabolic factors, previous studies report that WC has a stronger positive association with TG in men compared to women (19), which may cause the stronger association of WC with pre-hypertension observed in men. Regarding other biochemical factors, in our study, FBS and HDL-C were not associated with pre-hypertension findings in agreement with those of Rahmanian and Shojaie in the south of Iran (20). Previous reports have shown the negative association of HDL-C and WC as well as correlation of high blood glucose and hypertriglyceridemia using SEM (21). Hence, instead of a direct association, FBS and HDL-C may have indirect associations with pre-hypertension through WC and TG.
Dietary modifications with focus on adherence to a healthy diet rich in fruits and vegetables and avoiding poor diets rich in salt were found to be effective in decreasing the risk of pre-hypertension (13). However, in our population, both poor and healthy diets increased pre-hypertension through WC and TG in both genders. While energy balance is an important factor in the prevention of pre-hypertension (13), previous reports of TLGS referred to higher energy intakes among Tehranians with a healthy diet compared to those with poor diet (22); a finding which could shed more light on our current results regarding the relations observed of the healthy dietary pattern with WC and TG in the studied population. In this study, physical activity was directly associated with pre-hypertension among men. Our findings support the results of the Janghorbani et al., study conducted on Iranian men and women (11) and another report from a Western population (23), which showed no protective effect of physical activity on pre-hypertension. Guidelines recommend that all individuals should try to accumulate at least 30 minutes of moderate physical activity per day, 5 or more days a week, to benefit from the effects of physical activity; however, almost half of the individuals known to be physically active in our population had less than 30 min/week physical activity (24), an amount that cannot possibly lower the risk of pre-hypertension. Among socio-demographic factors, age, in both genders, and marital status, only in women, were directly associated with pre-hypertension. Previous studies suggest that married women may be at a health advantage compared to their unmarried counterparts due to increased availability of socioeconomic resources (25), which may mediate the negative association of marital status and pre-hypertension in women. However, married men and women are less conscious of their body weight compared to single ones (26), which can yield the positive association between being married and WC and TG in our study. In addition, married men, but not women, have a poorer diet, which in turn, increases pre-hypertension through WC and TG. Overall, it is important to advise married people, especially men, to engage in weight management programs and control their TG to prevent pre-hypertension.
In this study, compared to educated individuals, men and women with low education levels were predisposed to pre-hypertension, especially due to their higher risk of abdominal obesity. Highly educated people have a higher rate of doctor visits, which, in addition to education per se, may cause an increased awareness of the mechanisms of good health, body weight, and blood pressure; this, in turn, leads to better weight management and lower incidence of pre-hypertension (27, 28). Moreover, nutrition knowledge of educated individuals improves their quality of diet (29), which is consistent with results of our study, i.e. education increased a healthy diet in men; however, it should be noted that education could also increase poor diet less strongly in this study. The latter result underscores the need for translation of nutrition knowledge into better dietary practices to prevent pre-hypertension at least in part of the educated people. Regarding employment status, being employed was associated with a decrease in healthy dietary patterns in women. Recent findings suggest that employed women spend less time cooking compared to their housekeeping counterparts, which leads to lower diet quality and increased pre-prepared food consumption (30, 31). However, being employed was a protective factor against hypertriglyceridemia in women. Data, in accordance with those of previous studies (31), may be related to the stress of unemployment and its consequences on mental health (32).
This is one of the first efforts to test the sex-specific pathways of interrelated factors leading to pre-hypertension among a large Eastern-Mediterranean population without hypertension. However, certain limitations should be considered in the interpretation of the results of this study. First, this study has been conducted on an urban population, so its results may not be generalizable to rural populations. In addition, there are other predisposing factors that could affect pre-hypertension, which have not been considered in the current study.
In summary, a sex-specific conceptual model quantifying the association of socio-behavioral and cardio-metabolic risk factors with prehypertension has been presented in this study. Among the cardio-metabolic factors, only high WC and TG were directly associated with pre-hypertension in both genders, which could be considered as the cornerstone of tailored prevention programs for pre-hypertension in Tehranian men and women.