1. Context
Celiac disease (CD), gluten - induced atrophy of the small intestine, is an autoimmune condition, which can be seen in the context of other autoimmune disorders including Type 1 diabetes (T1D). T1D may be diagnosed in association with CD as high as six times of healthy individuals. On the other hand, T1D patients may be seen with concurrent CD in 8% of cases (1). Children with T1D represent higher propensity to CD. Geographical distributions, consumption of gluten - containing regimes, ethnical origins, and environmental factors are among CD contributing factors in T1D patients. Here we have reviewed the pathogenesis, diagnostic biomarkers, risk factors, and prognosis of CD in the context of pediatric T1D.
2. Evidence Acquisition
Literature published in the Web of Science, PubMed, Scopus, Google Scholar, and Cochrane Library between 1990 up to the October 2017 where studied. The main keyword used were celiac disease, Type 1 diabetes, and pediatrics. The star; “*” truncation was applied as “C*eliac” to recruit the differentially spelled form; coeliac disease.
3. Results
3.1. CD and T1D Juxtaposition, the Role of Immune System
Gluten - induced auto - reactive antibodies and cell mediated cytotoxicity orchestrate the main pathological events in CD (2). Of the all intraepithelial T lymphocytes (IELs) in patients with concurrent CD and T1D, nearly 12.5% have shown CD 25+, CD 39+, and Forkhead box P3 (FoxP3) + T regulatory phenotype (3, 4). Another characterized regulatory lymphocytic population in children with concurrent CD and T1D is CD3-/CD103+ cells, which further highlights the pivotal role of immunoregulation in the development of CD in the context of T1D (5).
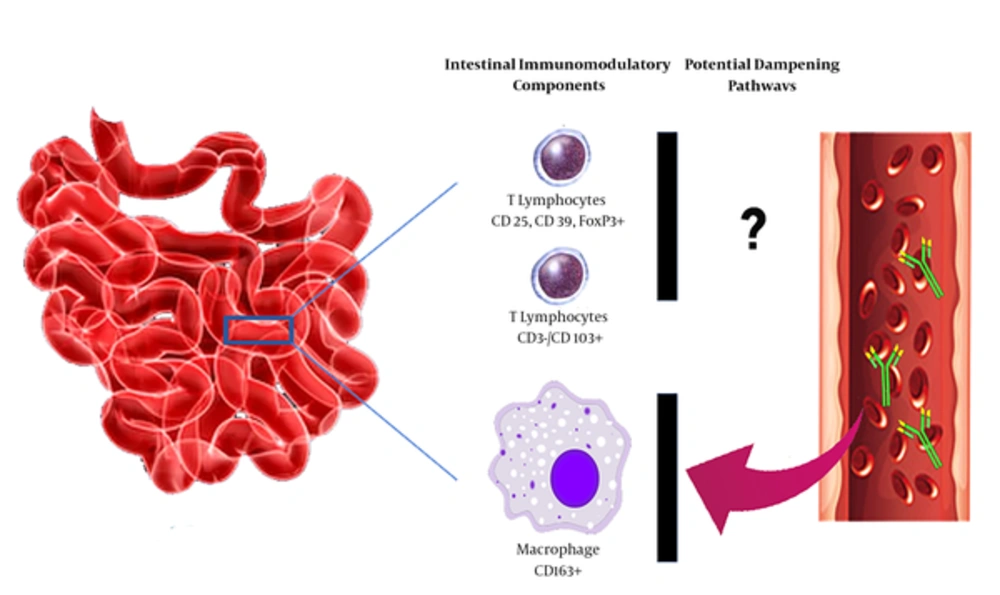
This higher regulatory function, however, seems to be functionally incompetent to prevent tissue damage in CD (4). Depressed local immunoregulatory function may be in part due to decreased activity of regulatory intestinal macrophages (CD163+). Some unspecific antibodies have been identified in patients with concurrent CD and T1D to represent binding specificity to these macrophages facilitating tissue damage by depleting these cells (Figure 1) (6). The role of immunomodulatory and inflammatory mediators in progress of CD in the context of T1D needs further evaluations.
Potential intestinal immunomodulatory components executed in patients with T1D and CD. Suppression of CD163+ macrophages by high - affinity auto - reactive antibodies can suppress activity of these cells. Incompetent immunoregulation can result in higher level intestinal mucosa damage in patients with concurrent T1D and CD. Abbreviations; T1D; type 1 diabetes, CD; celiac disease.
3.2. Clinical Features of CD in Children with T1D
Isolated childhood CD presents with malnutrition and malabsorption, vitamin deficiencies, iron deficiency anemia, growth failure, short statue, diarrhea, anorexia, constipation, nausea, and abdominal distention. These clinical features can help in better identification of CD in the context of T1D. However, gastrointestinal symptoms could be very mild in T1D patients with CD, it can hinder the growth in affected children (7). Growth failure and malabsorption have been suggested as well representatives of possible CD in the context of pediatric T1D (8). In those children who present none of the classic signs of CD, the diagnosis is amenable using serological assessments.
3.3. Screening of CD in Children with T1D
3.3.1. Recommended Intervals
Although routine screening for CD has been recommended in T1D, there is no consensus on the appropriate intervals for performing such tests. The American Diabetes Association and the International Society for Pediatric and Adolescent Diabetes recommended CD screening at the time of diabetes diagnosis (9, 10). In the follow up, however, the American Society has proposed performing screening tests whenever suggesting symptoms are evident. On the other hand, the International Society has suggested the screening program to be carried out annually for the first five years and biannually thereafter (10). The European and North American Societies for pediatric gastroenterology, hepatology, and nutrition have noted the ages of 2 and 3 years old, respectively, as the recommended time points in which the first CD screening tests should be performed in children with T1D (11, 12). For following up, however, the recent two societies have stated no specific requirements (11, 12).
3.4. Screening Biomarkers
There is a rough estimation by Australian Gastroenterology Society on the rate of undiagnosed CD ranging from 75% - 83% (13). Currently, the screening tests fall into either serological evaluation, biopsy examination, and human leukocyte antigen (HLA) typing.
3.5. Serological Markers of CD
The most commonly used serological tests designed to detect gluten induced autoantibodies include anti - gliadin (anti - GA), anti - endomysial (anti - EM), anti - transglutaminase (anti - tTG), and anti - deamidated gliadin peptide (anti - DGP) antibodies (1). The most sensitive and specific serological tests for CD include IgA antibodies against either tTG or EMA, and both IgA and IgG antibodies for DGP (14). It seems that detection of IgG isotypes of anti - tTG or anti - DGP does not augment sensitivity for CD diagnosis in the conditions with high titer IgA isotypes (15). Overall, serologic tests are useful to exclude CD in children with T1D with a negative predictive value of 98% (16).
Anti - tTG antibody is the most commonly ordered test for screening CD recommended by American, European, British, and North American societies for both diagnosis and follow up purposes (10-12, 17). Anti - tTG rendered a 90% positive predictive value, which was correlated with the antibody titer with higher titers correlating with higher predictive values (15, 18). In addition, Elitsur et al., noted that anti - tTG antibody titer is three times higher than upper limits is not a good representative of CD in children (19). Anti - tTG antibodies have been reported in a close relationship with HLA-DQB1*02 (20) and HLA - DQ2.5 (21).
IgA anti - EM antibodies are also highly specific for diagnosis of CD associated with childhood T1D (22). IgG1 isotypes of anti - EMA have been strongly associated with biopsy diagnosed CD in T1D (23). These antibodies may also be used as predicting factors for future CD development (24). On the other hand, anti - GA antibodies can be useful for diagnosis of late - onset CD in high risk populations (24). Some new serological markers have been proposed such as antibodies against serum albumin (25) and reticulin (26), which may be useful in screening the progression of CD in at risk populations.
3.6. Intestinal Biopsy Examination
Diabetic children with positive CD serology may demonstrate different histopathological features as compared with their non - diabetic counterparts. Intestinal histological changes in children with concurrent CD and T1D showed erythematous alternations resembling reflux esophagitis, which was different from the pattern seen in isolated CD (27). Intestinal biopsy, as the gold standard, could assist in CD diagnosis in asymptomatic cases.
3.7. HLA Typing
HLA - DQ2 has been mapped in 95% of patients with CD (28, 29), while HLA - DQ8 is seen in the remained 5% (30). HLA - DQ inheritance has been observed in one - third of patients with T1D (28). Accordingly, HLADQ2 comprised the most common allele identified in children with co - existence of CD and T1D (31). In fact, the inheritance of HLA - DQ is one of the main predisposing factor for development of CD in childhood T1D (32). The most significant association between HLA haplotypes and concurrent CD and T1D has been noted for HLA - DR3 - DQ2 and DR4 - DQ8 combinations, as well as presence of DQB1*06:02 allele (33). The role of HLA molecules, also known as Class II major histocompatibility complex (MHCII) - falls into their gliadin - derived antigens presenting activity to CD4+ lymphocytes (34, 35).
HLA typing has been recommended as the screening test for CD in high risk children by the British (17) and European (11) societies for pediatric gastroenterology, hepatology, and nutrition. Screening for HLA - DQ2/DQ8 alleles is recommended as a reliable negative predictor of CD in individuals with suggesting symptoms, as well as at risk populations such as T1D (36, 37). Despite these notions, using HLA - DQ2/DQ8 typing as a routine screening test is hindered owing to their high penetrance in general population, which limits their positive predictive values (38). Furthermore, applicability of this approach for screening CD in populations with low penetrance of these alleles is not recommended as results in high rate of undiagnosed cases (39).
3.8. Non - HLA Genetic Risk Factors of CD in T1D
According to a Genome - wide association study (GWAS), CD susceptibility is modified by at least 70 potential genes mapped within 42 non - HLA loci (40). Seven shared genetic loci between CD and T1D have been addressed by Smyth et al., (41). The list of shared genetic loci between CD and T1D are likely to be increased by more comprehensive studies. Some other genetic polymorphisms that have been associated with an elevated risk of CD in the context of T1D include rs10754558 and rs358294199 SNPs of NLRP3 (42), polymorphisms in IL - 6 (43, 44), CD14 (45, 46), and IL12A/SCHIP, CCR1, CCR2, CCr3, LPP, IL-17 (44, 47-49).
3.9. New Potential Biomarkers for Diagnosis and Screening CD
Some new potential markers for diagnosis of CD include Ischemia - modified albumin (IMA), Soluble Syndecan - 1 (SSDC1), Regenerating gene Iα (REGIα), Neurotensin (NT), Zonulin, and n - 3 polyunsaturated fatty acids (n - 3 PUFA). IMA is a metal - binding modified albumin and a marker of oxidative stress. Clinical significance of elevated levels of IMA has been evaluated in some disorders such as ischemic heart disorders, thalassemia, renal failure, and diabetes (50-52). SDC1 roles as a mediator derived from intestinal mucosa glycocalyx involved in maintaining permeability of intestinal epithelium. The role of SDC1 in regulating intestinal permeability makes it a potential marker with a central role in pathogenesis of CD (53-55). REGIα is a molecule with a substantial role in tissue remodeling processes that its levels have been high in active CD (56, 57). NT is an intestinal hormone synthesized and released by specialized cells located mainly in jejunum and ileum of small intestine (58). NT can promote inflammatory responses through inducing nuclear factor kappa B (NF ‐ κB) signaling pathway and production of proinflammatory cytokines (59, 60). Zonulin is another mediator directly involved in regulation of intestinal permeability by dissociating tight junction complexes (61-63). Belonging to n - 3 long - chain polyunsaturated fatty acids (n - 3 LCPUFA) family, n - 3 PUFA and its abnormal abdominal absorption in CD could pave the route for recruiting the molecule as a diagnostic marker in this condition (64). Table 1 has summarized studies assessing diagnostic applicability of these markers.
| Biomarkers | Authors, Year | Population | Implications | Ref |
|---|---|---|---|---|
| IMA | Yuksel et al., 2017 | 65 patients with CD and 65 healthy control | IMA levels were higher in celiac patients respective to controls. Among CD patients, those with positive serological test had significantly higher IMA levels | (54) |
| Sayar et al, 2015 | 37 children with CD and 29 healthy controls | IMA levels were significantly higher in patients. IMA level showed moderately positive correlation with t - TGA and Marsh Score. The level of IMA dropped significantly following a GFD. | (55) | |
| SD - 1 | Yablecovitch et al., 2017 | 49 children with CD and no history of treatment, 15 children with abdominal pain and no evidences of CD | The levels of soluble SD - 1 were significantly higher in CD children at the time of diagnosis compared to controls. The levels were significantly correlated with the degree of villous inflammation | (53) |
| REGIa | Planas et al., 2011 | 40 patients with CD, 35 healthy controls | REGIa showed significantly elevated levels compared to control subjects. The levels decreased following GFD which was correlated with reduction in tTG antibodies. I comparison, those patients with T1D showed normal levels of REG Ia. | (57) |
| Zonulin | Vorobjova et al., 2017 | 40 subjects with CD, and 40 individuals with small intestine functional syplasia as control | Serum zonulin levels were significantly higher in CD patients and were associated with Marsh score III. This correlation was prominent in CD patients with concurrent T1D. | (63) |
| Pro NT | Monten et al., 2016 | 96 children with CD and 89 healthy controls | The plasma level of pro - NT was higher in CD compared to non - diseased cases. The levels were correlated with intestinal damage degree, and anti - tTG antibodies | (60) |
| n - 3 PUFA | Tarnok et al., 2015 | 20 children with CD, 8 children with coexistence of CD and T1D, and 21 healthy children | The plasma levels of docosapentaenoic, docosahexaenoic, n - 3 PUFA, and long chains (n - 3 LCPUFA) were significantly lower in CD+T1D group compared to CD alone or controls. | (64) |
Abbreviations: CD, Celiac disease; IMA, Ischemia - modified albumin; NT, Neurotensin; PUFA, n - 3 polyunsaturated fatty acidsn - 3; REGIa, regenerating gene I alpha; SD - 1, Solouble Syndecan - 1.
3.10. Prognostic Impacts of CD on Childhood T1D
Abnormal lipid profile such as decreased HDL - C and elevated LDL - C in patients with concurrent CD and T1D has been noted, which may contribute to the higher risk of cardiovascular incidents in these patients (65). CD can also exaggerate complications such as nephropathy, retinopathy, as well as other auto immune disorders in children with T1D (37). CD may contribute to lower bone density, renal insufficiency, and quality of life of affected children and adults with T1D (66-68). Both Vitamin D deficiency (69) and antibodies against bone regulatory hormone - osteoprotegerin - participate in lower than optimal bone density in patients with CD (70). CD may also increase the risk of gastrointestinal tumors (71).
On the other hand, neither nutritional status, nor life quality of children with concurrent CD and T1D were different compared to individuals with T1D alone (72). In another study, patients with T1D who developed CD revealed no increase in complication rate in comparison to their counterparts without CD (73, 74). Accordingly, diagnosis of CD in the context of T1D showed no significant impact on HbA1c levels in another study (75). However, Leeds et al., argued that children with T1D associated with active CD or high levels of anti - tTG antibodies have a higher risk for diabetes associated complications (76). In general, timely diagnosis and management of CD in the context of T1D could protect patients from reduction in bone density and anemia, as well as deterioration in gastrointestinal functions, and provide them with a better quality of life.
4. Conclusions
Immune cytotoxic reactions with dampen immune regulatory functions can contribute to CD pathogenies in the context of T1D. The most common screening tests for CD include anti - GA, anti - EM, anti - tTG, and anti - DG antibodies. Typing for HLA of DQ - 2 and DQ - 8 can assist in diagnosis of silent CD in children with T1D. Newly proposed biomarkers of CD including IMA, SSDC1, REG Iα, pro - NT, Zonulin, and n - 3 PUFA can be used for diagnosis and screening CD in childhood T1D. Overall, active seropositive CD seems to be of clinical importance in T1D with significant impacts on the quality of life of the patients and occurrence of diabetes associated complications. Adherence to GFD is recommended in T1D children with active or silent CD to ameliorate related complications.