1. Context
The metabolic syndrome (MetS), as a complex of metabolic abnormalities could directly increase the risk of cardiovascular diseases (CVDs) and diabetes type 2 (1, 2), with a prevalence fast increasing in different populations in both the developed and developing countries (3-7). Although national data on Iranian adults indicates a decreased prevalence of MetS from 35.9% in 2007 to 32.9% in 2011 (8), it is still a considered a major health problem in our population.
Considering the World Health Organization (WHO) definition of health (9) and revolution in the medical framework of prevention and treatment of non-communicable diseases (10, 11), improving health care and health-related quality of life (HRQoL) has become the ultimate goal of health promotion programs, beyond increasing the individuals’ life expectancy (12, 13). As a patient-centered outcome, HRQoL refers to individuals’ own perceptions of their health status and life satisfaction (13, 14). Beyond the objective outcomes of MetS such as mortality and clinical functions, the negative association between MetS and HRQoL has been investigated in other countries (15-18). Among the first efforts in this field the negative association between MetS and physical or mental HRQoL have been reported mainly in Western societies, including an obese Italian population (19), an elderly Brazilian community (20) and postmenopausal Ecuadorian women (21). Considering the fact that, quality of life takes on different meanings based on the area and culture of population, there was a need to investigate the association between MetS and HRQoL in non-Western countries. To the best of our knowledge, findings of the TLGS provide the first evidence regarding this relationship in an urban Middle Eastern population (22). In this report, a summary of the TLGS findings regarding the association between MetS and HRQoL and its influential factors has been provided.
2. Evidence Acquisition
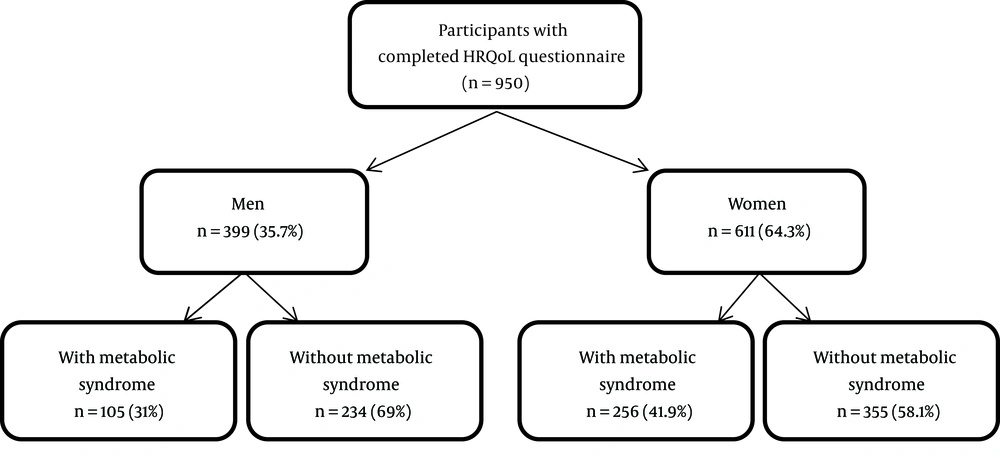
TLGS data collected between 2005 - 2007, was used to assess different aspects of the associations between MetS and HRQoL. Participants were adults aged ≥ 20 y, who were diagnosed without diabetes type 2 and had complete socio-demographic, clinical and HRQoL data (Figure 1). To assess HRQoL, we used the Iranian version of the short form health survey (SF-36), which has been validated in Iran (23); this widely used questionnaire contains 36 questions summarized into eight subscales, i.e four physical health related subscales including physical functioning, role limitations due to physical health problems, bodily pain, general health and four mental health-related subscales including vitality, social functioning, role limitations due to emotional problems, and mental health. The physical subscales constitute: (1) the physical component summary (PCS) and (2) the four mental subscales are termed as the mental component summary (MCS) (24). The score attributed to each subscale ranges from 0 to 100 as the worst and the best conditions of health respectively. Calculation of the PCS and MCS scores was done using the Quality Metric Health Outcomes Scoring software (25). The most common MetS definitions applied in the TLGS reports have been categorized in two, the insulin resistance-based- (26-28) and the waist circumference-based definitions (29-32).
3. Results
Mean age of participants was 46.5 ± 14.4 years and 64.3% of participants were female. There were significant differences in demographic and clinical characteristics between individuals with and without metabolic syndrome in both genders, except for fasting blood sugar, physical activity and smoking for women and except educational level, fasting blood sugar, physical activity and smoking and medication users in men. The findings of the association between MetS and HRQoL are presented in three main themes including: (1) the effect of gender, (2) the nature and duration of MetS and (3) the effect of definitions and measurements.
3.1. The Effect of Gender
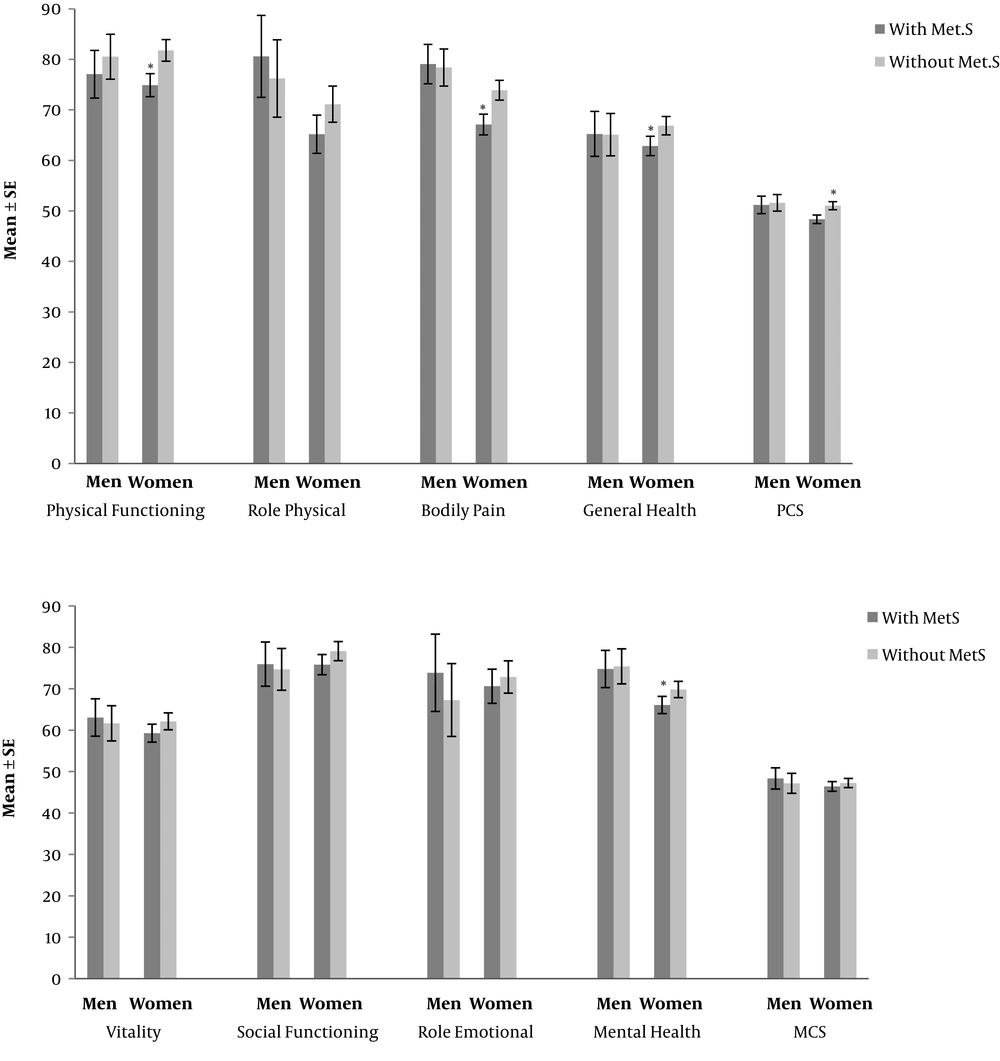
At first glance, comparing HRQoL between those with (n = 361) and without MetS (n = 589), our results showed significant differences in all HRQoL domains except for the vitality (P = 0.1) and role emotional (P = 0.06) sub-scales. After adjustment, these differences were observed only in women and not in men in all subscales (P < 0.05), except for role physical, vitality, social functioning, role emotional and MCS (Figure 2). In this regard a sex specific logistic analysis revealed MetS as a determinant of poor physical HRQoL only in women (OR: 1.78; 95% CI: 1.21 - 2.61). In addition in women, with increase in the number of Met.S components a significant decreasing trend in the PCS was observed (P < 0.001) (22).
Considering our previous findings, regarding impairment of HRQoL in the physical aspect only in women, but not in men, and the lack of evidence on the related underlying mechanism of this gender difference, menopause was hypothesized to be a potential influential factor. Hence, the association between MetS and HRQoL was further investigated in two different durations of women, including the reproductive and post-menopausal periods; the study population included 603 women, of whom 432 women were reproductive aged and the remaining were of the post-menopausal age (n = 171); findings indicated that in both groups of women, the components of MetS, including WC, TG, blood pressure and FBS were significantly higher and HDL was significantly lower than those without MetS. Comparison of HRQoL subscale scores indicated that HRQoL scores in PCS and physical subscales including physical functioning, role physical and general health were significantly lower in women of reproductive age compared to their counterparts without MetS. Neither MCS nor mental subscales scores were significantly different in both groups of women of reproductive age. In post-menopausal women, only the bodily pain subscale score was significantly higher in women without MetS compared to women with MetS. Poor HRQoL is defined as PCS and MCS scores below mean scores. In reproductive age women, ORs for poor PCS were significantly higher in those with MetS, compared to women without Mets after adjusting for age (OR: 1.7, 95% CI: 1.0 - 3.0; P < 0.05). However, ORs for MCS were not significantly different in women with and without Mets. In addition, in post-menopausal women, ORs of poor MCS and PCS did not differ significantly in women with and without MetS. To summarize, findings indicated that MetS was associated with poor HRQoL only in women of reproductive age and only in the physical aspect (19).
Previous findings of TLGS indicate that the impairment of HRQoL in those with MetS was observed mainly in women but not in men; therefore, potential influential factors responsible for gender differences in the association between MetS and HRQoL were further assessed. For this purpose, the structural equation modeling (SEM) approach was used, and findings indicated that the most physical subscales impaired by MetS in women were bodily pain and physical functioning. In addition, physical activity in both genders, age and education only in women and smoking only in men were factors directly associated with physical aspects of HRQoL. Marital status and physical activity in women and age in men were factors directly associated with mental aspects of HRQoL. Moreover, different structures of MetS and physical HRQoL constructs in men and women as well as age and smoking with significant gender-specific effects on mental HRQoL were factors responsible for gender specific pattern observed (21).
3.2. The Effect of Nature and Duration of MetS
Furthermore, the next question that arose in this regard was whether or not persistence of MetS has any influence on HRQoL. To answer this question, participants of the TLGS who had participated in all three phases of the study (n = 643) were categorized into four groups including (1) those without MetS in all three phases, (2) those with MetS in just one phase (transient) (3) those with MetS for two consecutive or intermittent phases (intermittent) and (4) those with MetS for all three phases and their HRQoL scores were then compared. The findings showed that after adjusting for confounding variables, the HRQoL scores in PCS, bodily pain and general health subscales differed significantly only in women of the mentioned study groups. However, for men, no significant differences were observed in HRQoL scores of four study groups. In the adjusted models, only women with intermittent MetS indicated higher risk for reporting poor PCS (OR: 2.75, 95% CI: 1.19 - 6.37; P < 0.001), compared to women without MetS. Whereas, men with transient, intermittent and persistent MetS did not show any difference in risk for reporting poor PCS and MCS, compared to men without MetS (33).
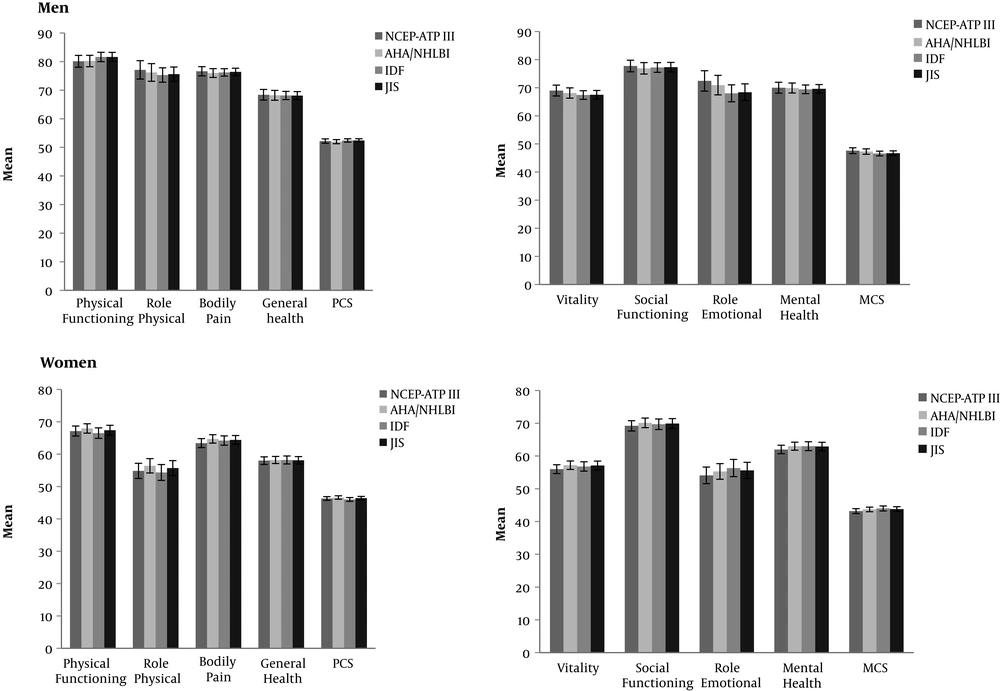
HRQoL scores according to different waist circumference-based definitions of metabolic syndrome in men and women. Data are represented as mean ± SE. AHA/NHLBI, American Heart Association/National Heart, Lung, and Blood Institute; IDF, the International Diabetes Federation; JIS, the Joint Interim Statement; MCS, mental component summary; NCEP-ATP III, the National Cholesterol Education Program Adult Treatment Panel III; PCS, physical component summary.
Based on previous studies, since glucose tolerance status could associate with impaired HRQoL (34, 35); the association between MetS and HRQoL was further investigated in TLGS participants (n = 946) considering glucose regulation impairment as an important component of MetS. The findings indicated that in both groups of women with normal and impaired glucose regulation, physical HRQoL was impaired in those with MetS compared to those without the condition. However, in both groups of men with normal and impaired glucose regulation no significant difference was observed based on presence or absence of MetS in men. To conclude, MetS was associated with poor HRQoL in physical subscales in both groups of women with normal and impaired glucose regulation(36).
3.3. The Effect of Definitions and Measurements
There are a number of definitions for MetS including IR-based and WC-based definitions, because of which the diagnostic power of these definitions of MetS in detection of poor HRQoL may differ. Therefore, the diagnostic impact of different definitions of MetS in detection of poor HRQoL as subjective measurement of health was further investigated. First, MetS was defined using four different WC-based definitions of MetS including the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III), American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI), the International Diabetes Federation (IDF) and the Joint Interim Statement (JIS). The findings indicated that in women, the highest rate of MetS was detected using AHA/NHLBI (47.0%) followed by the JIS (44.2%), NCEP-ATP III (42.4%) and IDF (40.3%) definitions. Whereas in men, the highest rate of MetS was detected by the JIS (51.9%), followed by IDF (51.3%), AHA/NHLBI (36.9%) and NCEP-ATP III (32.4%). The HRQoL subscale scores, using different definitions are provided in Figure 3, as indicated, using all WC-based definitions, HRQoL scores were higher in men, compared to women. Poor HRQoL in physical and mental aspects were defined as the first tertile of PCS and MCS, respectively. Findings of logistic regression analysis indicated that ORs (95%CI) adjusted for age, physical activity, smoking, education and marital status for poor PCS using NCEP-ATP III, AHA/NHLBI, IDF and the JIS definitions were 1.20 (0.64 - 2.13), 1.20 (0.70 - 2.11), 1.0 (0.60 - 1.70) and 0.92 (0.53 - 1.60) in men and 1.70 (1.04 - 2.63), 1.51 (1.0 - 2.40), 1.92 (1.20 - 3.10) and 1.63 (1.02 - 2.60) in women respectively. In addition, adjusted ORs (95% CI) for MCS using NCEP-ATP III, AHA/NHLBI, IDF and JIS definitions were 0.82 (0.50 - 1.50), 0.90 (0.50 - 1.54), 1.30 (0.73 - 2.20) and 1.30 (0.73 - 2.20) in men and 1.20 (0.80 - 1.90), 1.0 (0.62 - 1.52), 0.90 (0.06 - 1.40) and 0.90 (0.60 - 1.40) in women respectively. In summary, all investigated definitions of MetS were similar in detection of poor physical and mental HRQoL; furthermore, except for the AHA/NHLBI definition, all other definitions of MetS investigated significantly detected poor physical HRQoL, only in women (37).
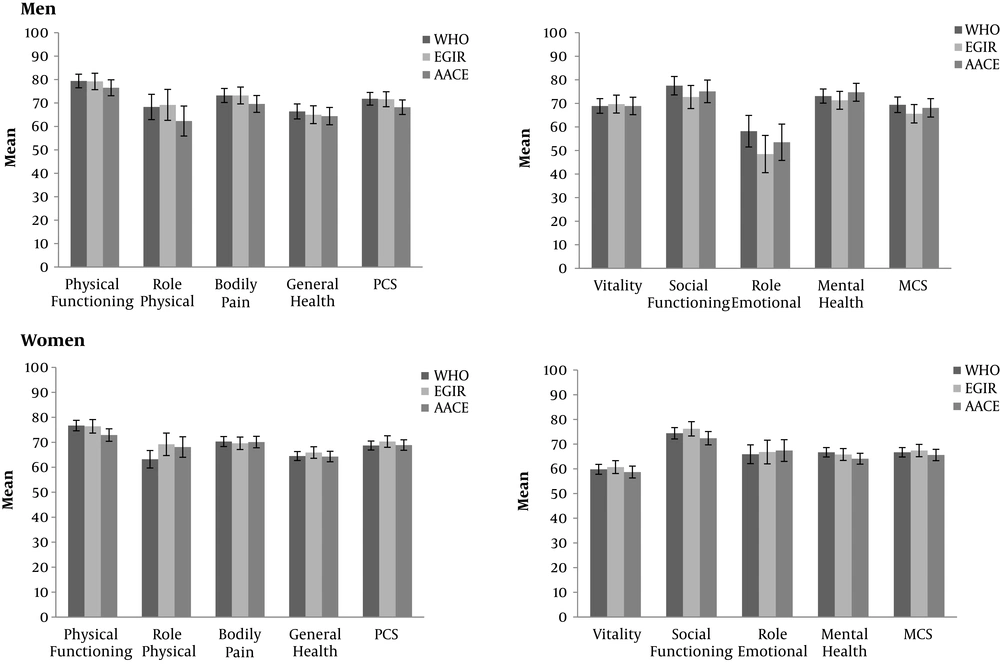
Second, the diagnostic powers of different IR-based definitions of MetS including the World Health Organization (WHO), the European Group for the Study of Insulin Resistance (EGIR), and the American Association of Clinical Endocrinology (AACE) in detection of poor HRQoL were compared. In women, the highest rate of MetS was detected using the WHO definition (40.6%) followed by AACE (29.5%) and EGIR (25.5%). In men, the highest rate of MetS was detected by WHO (44.2%) followed by AACE (33.2%) and EGIR (25.8%); HRQoL subscale scores, using different IR-based definitions are presented in Figure 4, as it is indicated, using all definitions, most of HRQoL scores were higher in men compared to women. Findings of logistic regression analysis indicated that ORs (95%CI) adjusted for age, smoking, education, marital status and menopause in women for poor PCS using WHO, EGIR and AACE definitions were 1.72 (0.88 - 3.35), 1.80 (0.69 - 4.69) and 1.95 (0.84 - 4.53) in men and 0.96 (0.57 - 1.60), 0.93 (0.48 - 1.81) and 1.01 (0.55 - 1.85) in women respectively. Adjusted ORs (95% CI) for detection of poor MCS using WHO, EGIR and AACE definitions were 0.75 (0.37 - 1.49), 0.93 (0.38 - 2.23) and 0.97 (0.41 - 2.28) in men and 0.89 (0.55 - 1.45), 0.97 (0.54 - 1.74) and 1.00 (0.56 - 1.79) in women respectively. In conclusion, as OR (95% CI) values indicated, none of (IR)-base definitions could detect poor physical and mental HRQoL in either gender (20).
HRQoL scores according to different Insulin-based definitions of metabolic syndrome in men and women. Data represented as mean ± SE. Abbreviations: AACE, the American Association of Clinical Endocrinology; EGIR, the European Group for the Study of Insulin Resistance; MCS, mental component summary; PCS, physical component summary; WHO, the World Health Organization.
4. Discussion
In summary, the current findings revealed that the association between MetS and HRQoL followed a sex specific pattern which was mainly significant only in women and in the physical aspect. Some of the gender difference observed in the association between MetS and HRQoL was due to differences in the structures of both MetS and the physical aspect of HRQoL in men and women and also, sex specific effects of age and smoking on mental aspect of HRQoL. Furthermore, the significant association between MetS and poor physical HRQoL in women, was limited to women of reproductive age. Gender difference in the association between MetS and HRQoL has also been reported in previous studies, some of which showed this association in women (15, 16) or in men (38). In addition, similar to TLGS findings, in some studies this relationship was significantly revealed only in the physical aspect (17, 39). However, other studies reported this association in mental (38) or both physical and mental aspects of HRQoL (40). Regarding the potential effects of duration and type of MetS components on the association between MetS and HRQoL, TLGS findings furthermore indicated that after considering both duration and presence of impaired glucose as an important component of MetS, the same gender specific pattern remained. In other words, irrespective of both duration of MetS and presence of impaired glucose regulation, this syndrome was still associated with poor physical HRQoL only in women. However, findings of another study in Finnish population, indicated that different glucose tolerance statuses were associated with impairment of HRQoL (35). In addition, in terms of using different definitions of MetS, findings indicated no significant gender differences in any of the applied WC-based and IR-based definitions of MetS in detection of poor physical and mental HRQoL. To the best of our knowledge, there is no similar study in this regard which has investigated the diagnostic value of different definitions of MetS in detection of poor HRQoL; based on our findings, while all WC-based MetS definitions detected poor physical HRQoL only in women with MetS, none of the IR-based MetS definitions could detect poor physical or mental HRQoL in either of genders.
The current review summarizes all TLGS findings regarding HRQoL which have been focused on MetS. This report could provide a comprehensive view regarding different aspects of the association between HRQoL and MetS in a Middle Eastern population. However, the cross-sectional nature of these studies, limits our ability to draw conclusions regarding the causal association between MetS and HRQoL. In addition not considering rural/sub-urban populations of Iran limits the generalizability of the current results. It is recommended that other possible confounders that could affect the present results, be considered in future research.
4.1. Conclusions
In the TLGS population, the association between MetS and HRQoL followed a sex specific pattern which was mainly significant only in women and in physical aspect. To confirm these findings further studies on different urban and rural populations in Iran seem essential.