1. Context
Cohort studies are used to determine the incidence of some defined outcomes, identify their risk and prognostic factors, assess the natural history of the disease and verify the impact of pragmatic interventions. The main strength of the cohort design for epidemiologic studies is that there is little doubt about the temporal relation between the exposures and the outcomes which are under study. Identification and classification of outcomes in cohort studies is a complex and challenging issue. Well-defined, -detected, and -classified outcomes are of characteristics of a well-established cohort study (1, 2).
Cohort studies have the capacity to evaluate multiple and different outcomes; however, this capacity is more substantial in longitudinal compared to life-table designs. The life-table design summarizes the effect of baseline exposures on the outcome over a period of time, whereas, the longitudinal design, which is potentially more expensive and complex, considers the time dependence of exposures and outcomes to address individual heterogeneity, changes during the time, and transitions between states of health and disease (3). Although population-based longitudinal cohort studies were established in western countries decades ago, numbers of such studies are rare and limited in low- and middle-income regions. The Tehran lipid and glucose study (TLGS) is one such a study, providing knowledge about the incidence and risk factors of some non-communicable diseases (NCDs) in West Asia which hitherto was relatively scarce (4). A part of this study has been dedicated to education for lifestyle modification, making the TLGS a pragmatic community trial (5). In this paper we will review the results from the TLGS regarding the incidence of some NCDs outcomes and the effect of educational interventions on some of these outcomes.
2. Evidence Acquisition
Among 580 papers published in English and 289 in Persian, up to March 2018, we only focused on papers which directly addressed the incidence of NCDs including cardiovascular disease (CVD), coronary heart disease (CHD), stroke, type 2 diabetes, pre-diabetes, hypertension, pre-hypertension, metabolic syndrome, chronic kidney disease, thyroid disorders, CVD-mortality and all-cause mortality. We also reviewed papers which reported the effect of educational interventions on cardiometabolic outcomes. Furthermore, as examples, we included some studies concerning the trend and change of cardiometabolic disorders during the follow-up in the TLGS.
3. Results
3.1. A Summary of the Methods
3.1.1. Study Population and Examinations
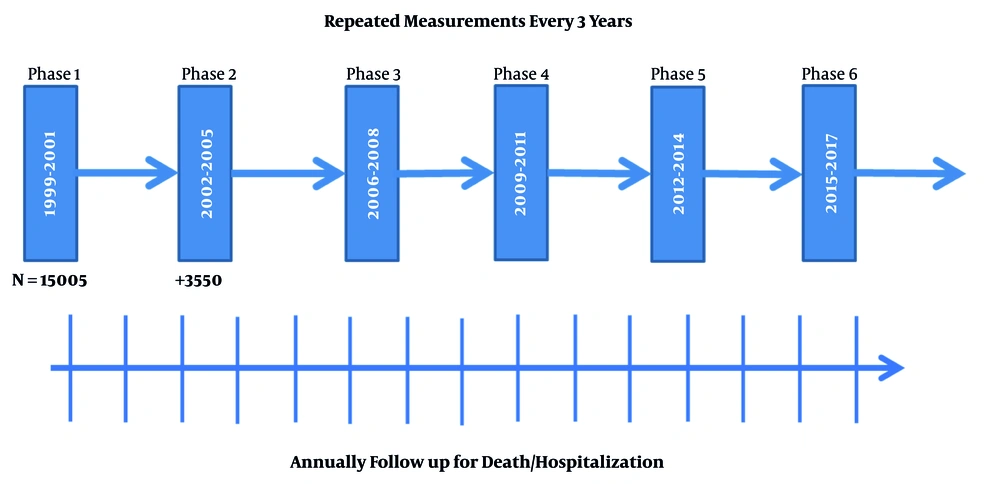
The first phase of the TLGS was initiated in 1999 - 2001 on a population under the coverage of three health centers in district no. 13 of Tehran. Totally, 15005 individuals, aged ≥ 3 years, participated in the first examination (response rate: 57.5%) (4). Reexaminations were conducted in a triennial manner and 3550 individuals were added in the second examination (Figure 1). To complete the pedigree of families, newborn children were added to the study population after they completed three years of age during the follow-ups. After completing baseline measurements (phase 1), participants under the coverage of one of the three health centers were assigned to an educational program for life style modification as a pragmatic community trial (5). Details of methods of sampling and measurements used at each examination, including demographics, medical and drug history, family history, physical exam, ECG, physical activity, nutrition and lab measurements, have been published before (4, 5). Many of the protocols have been based on the WHO and MONICA protocols for population surveys (4, 6).
3.2. Outcome Measurements
Besides the triennial reexaminations during in-person visits, all participants were followed up annually by telephone call to them or their family and asked about any medical event leading to hospitalization during the past year (Figure 1). In case of positive responses, related data were collected by a trained physician using hospital records or, if needed, a home visit. Moreover, in the case of mortality outside the hospital, data were collected from the death certificate, the report of forensic medicine and if needed a verbal autopsy from witnesses. All documents collected were reviewed by an adjudication committee and the final diagnosis was recorded, using a predefined coding protocol. The committee consisted of the physician who collected the data, an internist, an epidemiologist, a cardiologist, an endocrinologist, and other experts invited as needed. Response rate for follow-up was approximately 55 - 75 percent for in-person visits during different reexaminations and around 80 - 90 percent in annual telephone call follow-ups.
3.3. Educational Intervention
Interventions for lifestyle modification were carried out through primary prevention for cardio-metabolic disorders by improving dietary patterns, increasing physical activity, and encouraging smoking cessation. Primary educational interventions were classified in three categories, family-based, school-based and community-based interventions. The design of the TLGS for lifestyle interventions has been described previously (5); large and well-known interventional studies such as the North Karelia project and an international controlled trial in the multifactorial prevention of coronary heart disease and the American Heart Association guidelines were used in designing the intervention programs (7, 8). Table 1 shows a summary of interventions implemented up to the fourth triennial examination of the TLGS.
| Intervention | Method of Delivery | Providers | Compliance | |
|---|---|---|---|---|
| Family-based programs | Educational sessions | A 2-hour session with video and slide presentation and face-to-face consultation held with an average of 12 participants including family members, especially mothers, between baseline and 1st reexamination. Contents were mainly about healthy food preparation and nutritional values, benefits of physical activity, and harms of smoking. | Dieticians, general practitioners | About 50% of participants (70% of which were women) participated in the educational sessions |
| Publications | “Courier of Health”, published every 3 months, containing health-related topics (e.g. diet, nutrition, physical activity, smoking). Pamphlets, booklets and brochures (e.g. stress management techniques for students and parents). | Delivered by “health liaison” | Delivered to about 50% of households | |
| Community-based programs | Educating key persons | Educating socially significant figures (law enforcers, clergymen etc.). | Dieticians, general practitioners, cardiologist and diabetologist | More than 80% of the households participated in at least one of public gatherings for national or religious holidays between each two examinations |
| Public and group meetings | Providing health-related lectures during religious ceremonies (including Ramadan), 2 - 4 events annually. Conducting large-attendance seminars with the aim of presenting healthy lifestyles, 2 - 4 conferences annually. | |||
| School-based programs | Classroom curriculum | “Living tobacco-free” intervention program. Educational classes for students | Dieticians and trained teachers | Nearly 70% of the school-based intervention program was successfully implemented |
| Peer education | Forming school “health team” by students with the aim of peer education | Peer trained educator | ||
| Anti-smoking policies | Smoking prohibition for all the schoolchildren, teachers and employees inside the school | School supervisor | ||
| General policies | Labeling snacks, sold at school’s shop regarding their healthiness. Educating school principals and volunteer teachers for lifestyle modification. Educational sessions for parents regarding healthy lifestyle | Dieticians | ||
3.4. A Summary of the Outcome Results
Table 2 shows a review of the incidence of NCDs and related risk factors reported in the TLGS during 15 years of follow-up for men and women separately. For the outcomes of death and hospitalized events including cardiovascular diseases, the results were obtained by annual phone call follow-ups, confirmed by the adjudication committee. For other outcomes comprising diabetes, hypertension, metabolic syndrome and chronic kidney disease, the incidence are results of triennial in-person visits determined by drug history and/or confirmed by physical exam and lab measurements; details of methods have been provided for each outcome in its own specific paper, in which the predictors of related outcomes have also been explored (9-20). Appropriate follow-up time and detecting various outcomes enabled us to work on clinical prediction models regarding different cardiometabolic outcomes, CVD and diabetes in particular (15, 21-26). Future projects on validating, updating and developing new prediction models for using in health care services in national level is ongoing. Pooling data from the TLGS with other large population-based cohort studies in the Iran Cohort Consortium (www.irancohorts.ir) will be resulted in more comprehensive information and research projects in this regard (27).
| Event/Study Population | Mean Age (SD), y | Median Follow-up, y | Incidence Rate (95% CI), Per 1000 Person-Year | Ref. | |
|---|---|---|---|---|---|
| Men | |||||
| CVD | 458/2280 | 55.5 (10.73) | 11.9 | 19.2 (17.5 - 21.0) | (9) |
| Premature CVDa | 117/2235 | 40.0 (6.74) | 11.74 | 5.68 (4.74 - 6.81) | (10) |
| CHD | 320/2889 | 47.5 (12.3) | 10.3 | 11.9 (10.6 - 13.2) | (11) |
| Stroke | 90/1311 | 61.1 (7.8) | 13.9 | 5.9 (4.8 - 7.2) | (12) |
| DMb | 303/3620 | 42.2 (14.6) | 9.5 | 10.2 (9.13 - 11.4) | (13) |
| Pre-DMc | 853/2408 | 40.6 (13.9) | 9.14 | 46.1 (43.0 - 49.2) | (14) |
| HTNd | 40.7 (13.2) | 6 | 30.9 (27.8 - 34.3) | (15) | |
| Pre-HTNe | 705/1466 | 38.1 (12.11) | 9.2 | 76.4 (70.9 - 82.2) | (16) |
| ISHf | 113/1908 | 40.1 (13.2) | 9.57 | 6.6 (5.5 - 7.9) | (17) |
| IDHg | 262/2057 | 38.8 (12.2) | 9.57 | 14.5 (12.8 - 16.3) | (17) |
| MetSh | 565/1161 | 40.6 (14.9) | 9.3 | 74.9 (69.0 - 81.35) | (18) |
| CKDi | 206/1454 | 41.3 (13.4) | 9.9 | 13.26 (11.6 - 15.2) | (19) |
| Hypothyroidismj | 61/2258 | 40.0 (14.0) | 6.0 | (20) | |
| Hyperthyroidismk | 15/2258 | 40.0 (14.0) | 6.0 | (20) | |
| Thyroid autoimmunityl | 77/2171 | 40.0 (14.0) | 9.0 | 4.2 (3.4–5.3) | (28) |
| CVD-mortality | 131/2280 | 55.5 (10.73) | 11.9 | 5.5 (4.6 - 6.5) | (9) |
| All-cause mortality | 341/2532 | 55.5 (10.73) | 11.9 | 13.0 (11.7 - 14.5) | (9) |
| Women | |||||
| CVD | 331/2774 | 53.2 (9.36) | 11.9 | 11.0 (9.9 - 12.3) | (9) |
| Premature CVDa | 176/3703 | 43.9 (9.42) | 11.74 | 4.71 (4.07 - 5.47) | (10) |
| CHD | 236/3803 | 46.3 (11.4) | 10.3 | 6.5 (5.7 - 7.3) | (11) |
| Stroke | 64/1436 | 58.8 (6.8) | 13.9 | 3.6 (2.9 - 4.7) | (12) |
| DMb | 433/4780 | 39.3 (13.1) | 9.5 | 11.0 (9.99 - 12.0) | (13) |
| Pre-DMc | 902/3051 | 37.9 (12.1) | 9.25 | 36.8 (32.6 - 39.1) | (14) |
| HTNd | 37.6 (11.4) | 6 | 29.3 (26.7 - 32.1) | (15) | |
| Pre-HTNe | 735/2131 | 34.6 (10.05) | 9.2 | 48.9 (45.5 - 52.6) | (16) |
| ISHf | 122/2666 | 37.1 (11.2) | 9.57 | 5.06 (4.2 - 6.04) | (17) |
| IDHg | 208/2752 | 36.5 (10.6) | 9.57 | 8.4 (7.3 - 9.6) | (17) |
| MetSh | 552/1697 | 36.1 (12.1) | 9.3 | 43.35 (39.9 - 47.12) | (18) |
| CKDi | 517/1859 | 38.3 (12.0) | 9.9 | 28.5 (26.2 - 31.1) | (19) |
| Hypothyroidismj | 183/2803 | 40.0 (14.0) | 6.0 | (20) | |
| Hyperthyroidismk | 25/2803 | 40.0 (14.0) | 6.0 | (20) | |
| Thyroid autoimmunityl | 223/2849 | 40.0 (14.0) | 9.0 | 9.3 (8.2 - 10.7) | (28) |
| CVD-mortality | 69/2280 | 53.2 (9.36) | 11.9 | 2.3 (1.8 - 2.9) | (9) |
| All-cause mortality | 208/2986 | 55.5 (10.73) | 11.9 | 6.5 (5.6 - 7.4) | (9) |
Abbreviations: CHD, coronary heart disease; CKD, chronic kidney disease; CVD, cardiovascular disease; DM, type 2 diabetes; HTN, hypertension; IDH, isolated diastolic hypertension; ISH, isolated systolic hypertension; MetS, metabolic syndroms.
a Premature CVD was defined as having a CVD event before the age of 55 and 65 years in men and women, respectively.
b DM defined as fasting plasma glucose ≥ 126 mg/dL or 2-h postchallenge plasma glucose ≥ 200 mg/dL or medication for diabetes.
c Pre-DM defined as fasting plasma glucose ≥ 100 mg/dL or 2-h postchallenge plasma glucose ≥ 140 mg/dL without overt diabetes.
d HTN defined as systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg or antihypertensive medication.
e Pre-HTN defined as systolic blood pressure ≥ 120 mmHg or diastolic blood pressure ≥ 80 mmHg without overt hypertension.
f ISH defined as systolic blood pressure ≥ 140 mmHg and diastolic blood pressure < 90 mmHg.
g IDH defined as systolic blood pressure < 140 mmHg and diastolic blood pressure ≥ 90 mmHg.
h MetS was defined using the joint interim statement and national cutoff for waist circumference.
i CKD was considered an eGFR below than 60 mL/min/1.73 m2.
j Including both overt and subclinical hypothyroidisim. Total incidence rate (in men and women together) was 9.62 per 1000 person-year.
k Including both overt and subclinical hyperthyroidisim. Total incidence rate (in men and women together) was 1.6 per 1000 person-year.
l TPOAb-positive defined as TPOAb levels > 40 IU/mL.
Since the TLGS is a longitudinal cohort with repeated measurements for exposures, it gave us the opportunity to investigate the effect of changes of risk factors on outcomes. For instance, we demonstrated that the three-year increase in systolic and diastolic blood pressure were associated with increased risk of CVD independently (29); or this rise in fasting plasma glucose could help identify high risk populations for incident type 2 diabetes, independent of important traditional risk factors (30). We also showed the effect of changes in anthropometric measures on the incidence of diabetes, CVD and total mortality (23, 31, 32). On other occasions, we studied the variability or trend of risk factors, by unravelling age effect and period effect, and in addition, the effect of some risk factors in childhood or adolescence on outcomes in adulthood (33-36).
Finally, the effect of educational interventions for life style modification on the outcomes of diabetes, metabolic syndrome and its components have been investigated in both short-and long-term periods. After 3 years, life style modification in the intervention group decreased the incidence of diabetes by at least 30%, compared to the control (37). The intervention could prevent the incidence of pre-diabetes in men by around 20% (14). The effect of intervention on decreasing the incidence of metabolic syndrome, as a cluster of NCDs risk factors, lasted up to 3 - 6 years by reducing the incidence by 20%. The effect of intervention was more prominent in the reduction of lipids and glucose, than in other components of metabolic syndrome (38).
4. Conclusions
The TLGS is a much-cited longitudinal population-based cohort study with fascinating results regarding the incidence of NCDs and their related risk factors. It is also a pragmatic community trial which showed the effectiveness of some educational interventions in a middle-income country.
The results of the TLGS show a higher risk of NCDs in our population in comparison to Western and Asia-Pacific countries. For instance, the incidence rate of CHD and diabetes in Tehran is around one percent per year. This rate for incidence of hypertension is around three percent per year. Total CHD incidence in our population is comparable to that of the US in the seventies and much higher than that in China with around 1 - 2 events per 1000 person-years (11). The high incidence of pre-diabetes and pre-hypertension of around four and six percent per year respectively, indicates a peak of diabetes and hypertension incidence in near future if we do not improve our primary health care system.
Since the TLGS follows a population with a wide age range, in future follow-ups, we will be able to investigate the trajectory of risk factors and diseases from childhood to adulthood. Furthermore, more follow-up will provide the opportunity to study NCDs with longer latent periods like cancers. Although our annual follow-up rate of 80% - 90% for hospitalizations and death events in the giant metropolis of Tehran seems fascinating, we need to try and improve the triennial follow-up rates for in-person visits. The Tehran thyroid study (TTS) and the Tehran cardiometabolic genetic study (TCGS) have conducted in the framework of the TLGS. TTS aims to evaluate the prevalence, incidence and natural course of thyroid diseases and their long-term consequences in terms of cardiometabolic disorders and all-cause mortality (39). TCGS seeks to identify relevant patterns of genetic polymorphisms related to cardiometabolic risk factors which will allow exploration of gene-gene and gene-environment interactions regarding NCD outcomes (40). Nevertheless, new measurements for detecting intermediate outcomes like intima media thickness, aorta velocity, DXA and MRI as well as biomarkers can widen our research horizons.
Although the TLGS gives us an opportunity to detect the effect of community education on lifestyle modification in a real world, randomization in such a population-based community trial is difficult and is considered as a limitation for our interventions. Lost to follow-up and crossing between participants in intervention and control areas are other limitations of the TLGS. Appropriate epidemiological and statistical methods, such as using different statistical models, propensity score and inverse probability weighting for non-respondents, considering both intention-to-treat and per-protocol analysis and time and duration of exposure and time to event in analysis, are being taken into account to address these shortcomings.
In conclusion, the TLGS, as the oldest population-based cohort study in Iran besides the other Iranian large cohort studies, with precise detection of different outcomes has provided valuable evidence for prediction and prevention of NCDs in Iran and with some novelties in the world especially in the middle-income countries.