1. Tuberculosis and Its Importance for Healthcare Employees
Tuberculosis is an infection caused by bacillus-type bacteria (Mycobacterium tuberculosis), and mostly affects the lungs. When individuals with pulmonary tuberculosis cough, sneeze or spit, tuberculosis droplets spread into the air and infect others. Inhaling only a few bacillus (1) is sufficient for a person to be infected with tuberculosis. Every year 10 million people are infected with tuberculosis, and although it is an entirely preventable and treatable disease, 1.5 million people die from it each year. These statics confirm that tuberculosis bacillus is one of the world’s most infectious bacteria (2).
The burden of tuberculosis is increasing globally at an alarming rate every day, and causes a significant public healthcare problem, especially in developing countries (3). According to data published by the World Health Organization (WHO), the majority of individuals that are infected live in low- and middle-income countries. It is estimated that approximately one-quarter of the world’s population is infected by tuberculosis bacteria (2). In Turkey began to be defined as tuberculosis incidence density in 2005. Incidence density is the number of cases per 1000 people. In 2005, the incidence of tuberculosis was recorded as at 29.4% in a population of 68 million. Over time, the incidence rate has decreased compared to the population growth rate. However, in 2014 the number of cases remained the same compared to the previous year. According to data from 2018, tuberculosis incidence density was determined as 14.1% a population of 82 million (4).
Tuberculosis shows significant improvement with the implementation of an appropriate treatment segement (3). During the treatment process, both the patient and their healthcare provider have a number of responsibilities. Specifically, patients play a big role in this process by following the treatment procedures given to them, and healthcare workers by preventing the breakdown of the infection chain in patient follow-up visits (3).
Healthcare professionals are at risk of accidents and disease in hospitals for the following reasons: infections, drugs, use of dangerous materials, biohazard waste, ergonomic design deficiency, lack of appropriate working conditions and materials, excessive workload, and careless behavior of other employees (5). In previous studies, it was reported that physicians, nurses and other medical staff are exposed in mechanical and physical terms to biological agents, like viruses, bacteria and fungi, due to lack safety precautions in their work environment (5, 6).
Healthcare employees treat patients from all walks of life, regardless of whether they work in primary healthcare or large complex healthcare institutions (5). Due to this, healthcare employees are at risk for a number of infections (5). Many infectious diseases, especially tuberculosis, pose a risk for healthcare employees (3, 5). There are studies that confirm that being a healthcare employee is a risk factor, especially for tuberculosis (5, 7). A study conducted in South Africa, noted that healthcare employees are at the forefront of the war against tuberculosis. There is now strong evidence that tuberculosis is a professionally acquired disease for healthcare employees due to prolonged exposure to tuberculosis patients, the inadequacy of infection control measures, and high prevalence of undiagnosed tuberculosis (8).
2. Knowledge Levels of Healthcare Employees About Tuberculosis
In many countries, healthcare employees receive regular training about infection control (1, 9). This training covers specific areas within the general infection control rules. However, specific infection training sessions do not yield the expected outcomes; due to the fact that the concept of infection is abstract in nature, and thus cannot be foreseen by people (9). In an extensive study where researchers interviewed with one hundred and thirty-eight assistant health workers, 96 community health workers and 39 nurse assistants; with 89 (66%) of participants interviewed in the last 10 years and 49 (36%) in the last 12 months, it was determined that 103 (76%) personnel lacked information on how to prevent contamination (6). Another study conducted in Turkey, which included 126 family physicians working in primary healthcare settings, found that tuberculosis knowledge did not meet the desired levels; the study researchers suggested that training programs were needed to increase awareness levels and to ensure that best practices are adopted (3). In this study, general practitioners were questioned regarding the following: duration of time spent by patients in the same waiting room as patients receiving tuberculosis treatment and their use of protective masks, approach to breastfeeding children with pulmonary tuberculosis, type and evaluation of the BCG vaccine, mask type that should be used, and initial treatment protocol for lung tuberculosis. Unfortunately, the researchers noted significant differences among the answers provided by individual healthcare practitioners. This emphasized that the education received in medical school was insufficient and that in-service training should continue (3). In another study that included 293 medical school students, it was found that students who received tuberculosis-related training had significantly more knowledge about how the disease was transmitted, risk factors, symptoms, diagnosis protocol, duration of treatment and because of this they were less concerned about being infected compared to students who did not receive such training (9).
3. Monitoring of Health Workers During Tuberculosis Infection
Healthcare employees can potentially be infected by patients with both diagnosed and undiagnosed Tuberculosis (1, 10) Within the scope of infection control measures, and as standard precaution, every patient who is admitted to any healthcare organization is considered to be infected. However, a patient infected with Tuberculosis should be approached with consideration to a number of rules, which are entirely unlike the standard approaches (1). The fact that it is not known what type of infection patients have upon hospital admission increases the risk of infection (1, 10). In this regard, it is important that respiratory isolation rules must be applied (1, 10). Since the tuberculosis bacillus is less than 5 microns and rapidly spreads in the air, the environment in which a tuberculosis bacillus carrier comes in contact with soon becomes infected. In order to protect against the rapid spread of particles in the environment in question, N95 enabled masks should be used. The fact that respiratory isolation rules are not applied in the triage area of hospitals leads to an increase in tuberculosis infections (10). Consider when a patient is admitted into the triage area, and healthcare professionals have completed all the necessary assessments, that single tuberculosis case has now infected numerous healthcare employees. When the presence of tuberculosis is confirmed in a patient, all healthcare employees in that entire treatment chain are screened for tuberculosis (1, 10, 11).
There are two main screening tools for tuberculosis, the tuberculosis skin test (PPD) and a chest x-ray, following which prophylactic treatment is started based on the condition of the person. The PPD test is done on the forearm of the test subject. If the person has previously encountered tuberculosis bacillus, hyperemia (redness) and induration (blistering) will occur at the test site within 2 - 3 days. Although the diameter of hyperemia is not important, the diameter of the relief (induration), which is determined by hardness, is important. The presence of induration (blistering) should be determined via inspection and palpation. The diameter of the induration is measured millimetrically with a transparent ruler 48 - 72 hours (2 - 3 days) after testing. Individuals that have a PPD test score at or above 15 mm are considered to be positive. At which point, the following treatment protocols are applied: 6 months Isoniazid, 9 months Isoniazid, 4 months RIF, 3 months RIF and Isoniazid or 3 months isoniazid and rifapentine (1). Training and support should be provided to individuals in order to maintain treatment adherence. If necessary, preventive treatment should be provided under direct supervision and should be continued without interruption. If any breaks are taken during the treatment protocol, the length of these breaks should be added onto the end of preventive treatment. This treatment is considered adequate if the patient completes six months of preventive treatment within 9 months, or a 9 month course of preventive treatment within a 12 month period (1).
When medical staff undergo screening for tuberculosis, it causes psychological trauma and cost for healthcare employees (1, 10). The costs associated with an examination for each staff member makes things difficult for healthcare institutions. Also, most staff members experience significant burnout during this screening process. If a member of the healthcare staff is suspected of having tuberculosis, they move away from their families to receive treatment in the hospital if necessary. This not only affects the lives of individuals but causes a loss of labor in healthcare institutions.
4. Things to Do to Protect Healthcare Employees From Tuberculosis
Healthcare employees play a central role in controlling the spread of tuberculosis (9). In this context, screening of healthcare employees is of great importance. Regular health screenings ensure the safety of all employees, and significantly benefit hospitals. Specifically, it is imperative to establish a periodic screening program and apply both environmental and personal protective measures in order to detect and monitor tuberculosis among primary healthcare workers (11). This has both sociological and economical advantages (5).
An additional challenge for healthcare employees, in the protection from tuberculosis, is a lack of knowledge. In a study conducted in England between 2009 and 2013, it was reported that healthcare employees lacked knowledge about tuberculosis (12). In another study conducted with allied healthcare employees in Brazil, although the importance of preventing tuberculosis was already known, it was found that there was a significant lack of knowledge amongst healthcare employees (6).
It is crucial that healthcare employees have qualified knowledge about protection from tuberculosis and also about using personal protective equipment. It is especially important that healthcare employees have adequate equipment in healthcare settings like primary care, emergency services, and home care services (13).
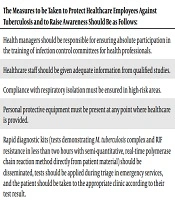
In light of this information, measures to protect health workers against tuberculosis and increase awareness are vital. These measures are listed in Box 1.
| The Measures to be Taken to Protect Healthcare Employees Against Tuberculosis and to Raise Awareness Should Be as Follows: |
|---|
| Health managers should be responsible for ensuring absolute participation in the training of infection control committees for health professionals. |
| Healthcare staff should be given adequate information from qualified studies. |
| Compliance with respiratory isolation must be ensured in high-risk areas. |
| Personal protective equipment must be present at any point where healthcare is provided. |
| Rapid diagnostic kits (tests demonstrating M. tuberculosis complex and RIF resistance in less than two hours with semi-quantitative, real-time polymerase chain reaction method directly from patient material) should be disseminated, tests should be applied during triage in emergency services, and the patient should be taken to the appropriate clinic according to their test result. |
Administrative measures, such as the implementation of an effective infection control program, as well as environmental and respiratory measures are of great significance in preventing the spread of tuberculosis. In this context, healthcare managers have important duties. Healthcare managers should manage this process within the framework of protecting healthcare professionals (13, 14). Considering the cost analysis and labor force, every measure implemented will result in considerable benefits.