1. Background
β-Thalassemia is the most prevalent hereditary blood disorder. Thalassemia is caused by quantitative problems (lack or partial reduction of globin chains), which lead to ineffective erythropoiesis (1). Patients with β-thalassemia major need regular blood transfusion, as well as iron chelating agent in order to have a normal life (1). It is more common in the Mediterranean and tropical regions near the equator in Asia and Africa (2). Thalassemia disorders are classified into three categories as minor, intermediate, and major. They need regular blood transfusion and their survival depends on repetitive transfusion (1). The purpose of transfusion is to correct anemia and suppress excessive erythropoiesis (1). Hepatitis C virus (HCV) is a transfusion transmitted disease and one of the major health problems in the world (3-6). Approximately 170-200 million people are infected with the virus in the world. The prevalence of HCV is approximately 0.2% to 40% (4-8). Hepatitis B virus (HBV) is the most common one in the world and about 1 million cases die from this infection every year (9). Careful screening of donors and also several laboratory tests on donor's blood decreased the incidence of the transfusion transmitted diseases such as HBV and HCV infections (10). Based on different studies, the prevalence of HCV infection in patients with thalassemia is approximately 4.4% - 85% in the world (11, 12). The incidence of HCV infection in children with β-thalassemia major in Egypt is reported 40% (13). In another study in Pakistan, the prevalence of HBV and HCV infections in patients with thalassemia was reported 1.7% and 35%, respectively (14). Since blood transfusions in patients with β-thalassemia major is vital and necessary and HBV and HCV are the major complications of blood transfusion, the current study aimed at determining the prevalence of the surface antigen of the HBV (HBsAg), HB core antigen (anti-HBc), and antibodies to HCV (anti-HCV) in patients with thalassemia major with frequent blood transfusions. Therefore, all the blood bags were checked for HBV and HCV and then transfused to patients. The current study mainly aimed at evaluating the prevalence of HBsAg, anti-HCV, and anti-HBc in patients with β-thalassemia referred to Blood Banking Department of Ghaem Hospital.
2. Methods
The current study was conducted at Ghaem hospital of Mashhad on 50 patients with β-thalassemia major including 25 males and 25 females in the age range of 2 - 46 years, and the mean age of 17; the study was financially supported by the Research Deputy of the School of Medicine, University of Mashhad, Mashhad, Iran. demographic data such as age, gender, interval between transfusions, and also the age at beginning of transfusion were derived from patient`s records. In the current study, variables included HBsAg, anti-HBc, anti-HCV, ALT (alanine aminotransferase), and AST (aspartate aminotransferase). The samples were the serum of the patient separated from the blood existing in pipes lacking anti-coagulant agents. Before taking blood sample, the informed consent form was signed by the subject. If the patient was under 18 years old, the consent form was signed by the parents. After sampling by laboratory experts, blood samples were kept in sterile tubes at room temperature for 30 minutes for blood clot forming. Then, serum was separate and stored at 20°C. Liver enzymes (ALT, AST) were measured by the auto analyzer (Hitachi, Japan).Also, the enzyme-linked immunosorbent assay (ELISA) was used to evaluate viral infection (HBsAg, anti-HBC, and anti-HCV). The current study was approved by the Ethics Committee of Mashhad University of Medical Sciences. The collected data were analyzed by SPSS version 21. Descriptive variables, chi-square, and t test were used to analyze the data.
3. Results
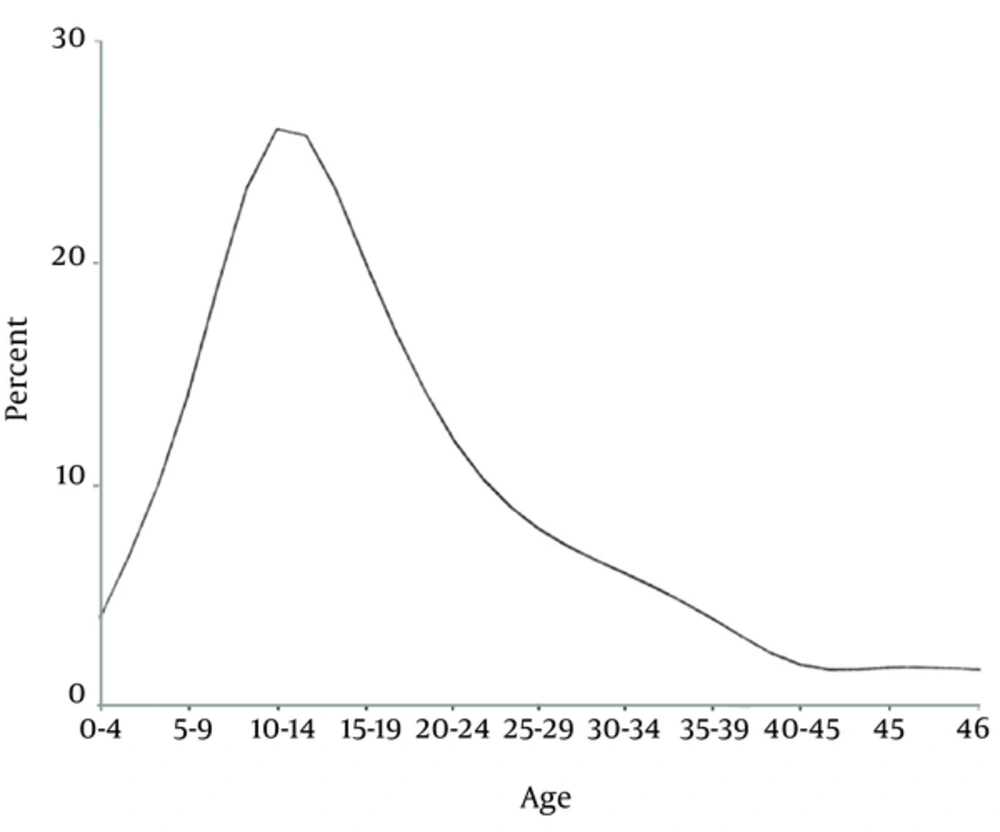
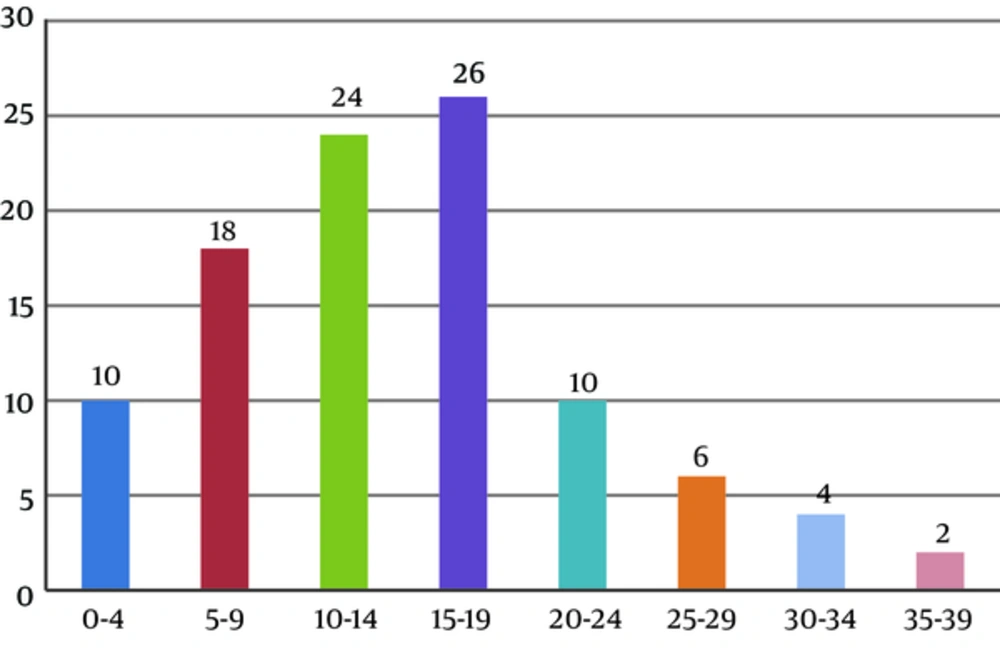
The current study was performed on 50 patients with thalassemia major at Ghaem hospital affiliate to Mashhad University; 25 (50%) cases were male and 25 (50%) female within the age range 2 - 46 years. The mean age was 17 and most patients were in the age range of 10 - 12 years (Figure 1). The patients had blood transfusion once a month in this center and received blood products for 1 - 35 years (Figure 2). In the current study, four cases were positive for HBsAg (8%), two males and two females. The age range of the infected patients positive for HBsAg was 15 - 25 years, and duration of transfusion in the patients was 15 - 19 years. There was no significant difference between HBsAg and duration of transfusion (Table 1). Eight cases were positive for anti-HCV (16%), five males and three females. The age range of patients with a positive serology for HCV was 10 - 20 years, and duration of transfusion in the patients was 15 - 17 years (Table 2). Also, three patients were positive for anti-HBc (6%) and duration of transfusion in the patients was 5 - 19 years. There was no statistically significant difference between anti-HBc and duration of transfusion (Table 3). Liver enzymes (AST and ALT) were measured in 30 patients and the others (20 cases) missed follow-up. ALT level varied 24 to 342 U/L. ALT was more than 40 U/L in four patients with positive test results for HBsAg. ALT levels were higher than 40 U/L in seven patients positive for anti-HCV. Levels of AST varied from 19 to 255 U/L and in 75% of the patients were more than 85 U/L. AST and ALT levels were more than 40 U/L in three patients.
| Number of Transfusion | HBsAg | Total | |
|---|---|---|---|
| - | + | ||
| 0 - 4 | 5 (100) | 5 (10) | |
| 5 - 9 | 9 (100) | 9 (100) | |
| 10 - 14 | 12 (100) | ||
| 15 - 19 | 9 (69.2) | 4 (30.8) | 13 (100) |
| 20 - 24 | 5 (100) | 5 (100) | |
| 15 - 29 | 3 (100) | 3 100) | |
| 30 - 34 | 2 (100) | 2 (100) | |
| 35 - 39 | 1 (100) | 1 (100) | |
| Total count | 46 (92) | 4 (8) | 50 (100) |
a Values are represented as No. (%).
| Number of Transfusion | Anti -HCV | Total | |
|---|---|---|---|
| - | + | ||
| 0 - 4 | 5 (100) | 5 (100) | |
| 5 - 9 | 8 (88.9) | 1 (11.1) | 9 (100) |
| 10 - 14 | 12 (100) | 12 (100) | |
| 15 - 19 | 6 (46.2) | 7 (53.8) | 13 (100) |
| 20 - 24 | 5 (100) | 5 (100) | |
| 15 - 29 | 3 (100) | 3 (100) | |
| 30 - 34 | 2 (100) | 2 (100) | |
| 35 - 39 | 1 (100) | 1 (100) | |
| Total count | 42 (84) | 8 (16) | 50 (100) |
a Values are represented as No. (%).
| Number of Transfusion | Anti-HBc | Total | |
|---|---|---|---|
| - | + | ||
| 4 - 5 | 5 (100) | 5 (100) | |
| 5 - 9 | 8 (88.9) | 1 (1.1) | 9 (100) |
| 10 - 14 | 11 (91.7) | 1 (8.3) | 12 (100) |
| 15 - 19 | 12 (92.3) | 1 (7.7) | 13 (100) |
| 20 - 24 | 5 (100) | 5 (100) | |
| 15 - 29 | 3 (100) | 3 (100) | |
| 30 - 34 | 2 (100) | 2 (100) | |
| 35 - 39 | 1 (100) | 1 (100) | |
| Total count | 47 (94) | 3 (6) | 50 (100) |
a Values are represented as No. (%).
4. Discussion
In the current study, the prevalence of HBsAg, anti-HCV, and anti-HBc in the patients with β-thalassemia major was 8%, 16%, and 6%, respectively. In recent years, many studies are conducted to evaluate HBV and HCV status in patients with β-thalassemia major. Also, the average of ALT and AST in positive HBsAg cases was highly identical with the results obtained in the current study.
Karimi et al., studied HCV antibodies among 466 multi- transfused children with thalassemia in Shiraz, Iran and reported the prevalence of anti-HCV as 15.7%, which was approximately similar to the results of the current study (15). Mirmomen et al. (14), in a multicenter study on 732 patients with β-thalassemia major reported the prevalence of anti-HCV and HBsAg as 19.6% and 1.5%, respectively. In comparison with the current study that reported the prevalence of 16%, there was significant increase that maybe due to high volume of patients in Mirmomen's design with respect to that of the current study. Another study in Isfahan, Iran revealed that the prevalence of HCV positive among patients with thalassemia was 11%. In comparison with the current study that reported the prevalence of 16%, there was significant increase. Mishra et al. (16), in India studied 66 patients with β-thalassemia major that had repetitive transfusion and reported the prevalence of anti-HCV and HBsAg as 18.2% and 3%, respectively. Also, the average levels of ALT and AST in positive anti-HBc subjects were highly identical with the results obtained in the current study.
Chakrabarty et al. (17), studied 200 patients with β-thalassemia major. They used rapid immunochromatographic test and their sera were tested for HBsAg and HCV-Ab. The positive HBsAg and HCV-Ab results were confirmed by ELISA; four (2%) patients were HCV-Ab positive and 13 (6.5%) HBsAg positive. Univariate analysis showed that older age, longer transfusion duration, HBsAg seropositivity, and higher serum ferritin levels were significantly associated with a higher prevalence of HCV. Blood screening strategies and HBV vaccination led to a dramatic decrease in the prevalence of HBV during the last decades in Bangladesh. However, post-transfusion transmission of HCV is still a major health concern in multi-transfused patients. As the prevalence of HCV infection is much higher among patients with β-thalassemia compared with HBV infections, routine screening of donated blood for HCV by ELISA is highly recommended (17). In comparison of the current study results with those of Chakrabarty, the incidence of anti-HCV was higher in the current study and there was no statistically significant difference between HBsAg and duration of transfusion. The other studies from some other countries reported an HCV infection rate of 40.5% in Jordan (17), 30% in India (18), 35% in Pakistan (19), 33% in Kuwait (20), and 14.5% in Egypt (21).
The reason for these wide ranges can be due to difference in the type and sensitivity of testes, the prevalence of HCV in the relevant population and the time of screening. In comparison with other developing countries, the prevalence of HCV infection among patients with β-thalassemia was lower in Iran. The countries with a higher HCV prevalence in general population had a higher prevalence rate among patients with thalassemia, too.
In the current study on 50 patients with thalassemia major referred to Ghaem Hospital in Mashhad, no one had any record of dialysis, hepatitis, surgery, and injecting drug addiction. Also, none of the patients were married. In recent years, prevailing wide filtering toward reduction of transmitting infections through transfusion is done and also high efforts were made to eradicate HCV, detect HBV, and treat them in order to reduce the number of such patients. But, special acts such as employing PCR to identify infected people in order to decrease infection transition should be made.
4.1. Conclusion
Since ELISA was employed in the current study to evaluate HBV and HCV status, it is advised that the techniques with higher sensitivity such as PCR be used to reduce receptive positive cases.