1. Background
Pediatric tuberculosis (TB) is a common health problem in developing countries. It causes significant morbidity and mortality worldwide. The majority of cases in childhood present with primary pulmonary TB. Mediastinal lymphadenopathy (LAP) with or without parenchymal lesions is the significant finding of primary pulmonary TB in children and is also considered the fingerprint of the disease (1, 2). Early and precise diagnosis is mandatory for the control and treatment of pulmonary TB, yet clinical signs and symptoms of the disease are somewhat equivocal in children compared with adults. Most pediatric patients have negative smears from sputum or gastric aspirates and negative culture of Mycobacterium tuberculosis because of the paucibacillary nature of the disease in children (3). Therefore, the diagnosis of pulmonary TB is frequently based on a combination of clinical features and radiologic findings (4). Chest X-ray (CXR) is the initial step for the radiologic diagnosis of the disease; however, it has a limited capability in detecting lymph node involvement. Therefore, computed tomography (CT) is accepted as the modality of choice for detecting mediastinal LAPs and the demonstration of their localizations and characteristic features (1, 4-8).
Community-acquired pneumonia (CAP) is a potentially serious infection in children, and the rate of hospital admissions for complicated CAP is significantly high (9, 10). Therefore, imaging has an essential role in diagnosing CAP, mainly when the history and physical examination findings are inconsistent (9). In cases of complicated CAP, the sensitivity and accuracy of CT are superior to those of CXR. Therefore, it is generally the modality of choice for the definitive characterization of the features complicating CAP (10, 11).
Clinical differentiation and diagnosis of both entities may be difficult because of the overlapping features of pulmonary TB and CAP, which may result in therapy failure (12). However, imaging may help differentiate the entities, mainly based on the presence of mediastinal LAP. Therefore, it is considered that CT can suggest TB as a possible cause by demonstrating typical LAP in suspected cases of CAP (12).
A few studies in the literature determine the mediastinal LAP characteristics on a chest CT scan of children with pulmonary TB (5, 13-16). To the best of our knowledge, one study (17) compared the lymph node involvement in pulmonary TB and CAP in children.
2. Objectives
The present study aimed to describe the CT features of mediastinal lymph node involvement in pediatric pulmonary TB infection and compare these findings with those of pediatric CAP to identify discriminative features of primary pediatric TB LAP.
3. Methods
3.1. Study Population
A total of 83 patients at the age of 18 years or younger who were admitted to our hospital from May 2005 to January 2019 were included in our study. Of the 83 patients, 45 children had the diagnosis of primary pulmonary TB (group I). TB was diagnosed according to the history of contact with an infected person with TB, positive purified-protein derivative (PPD) skin test, positive QuantiFeron test, clinical and radiographic signs related to TB, no resolution of symptoms, and signs of infection after standard antibiotic treatment, pathology or bacteriology associated with TB, and response to the anti-TB treatment. In our routine practice, all children with suspected pulmonary TB underwent CXR as the initial evaluation. Chest CT scan was performed in cases in which CXR was inconclusive and clinical suspicion was high for pulmonary TB.
The other 38 children diagnosed as having CAP, who had a CT examination after CXR for suspected complications related to CAP, were included in the comparison group (group II). Symptoms and signs of pneumonia in children were the combinations of fever and cough and some other respiratory findings (e.g., tachypnea, increased work of breathing). The diagnosis was confirmed in this group by improvement with antibiotics.
Children who had underlying lung diseases such as cystic fibrosis or any immunosuppressive medical conditions (e.g., HIV infection, malignancy, immunosuppressive therapy), who had previously been treated for TB, and who had fungal or parasitic infection were excluded from the study. Only patients who had contrast-enhanced CT (CECT) of the chest at presentation were included in the study. Ethics approval for this study was obtained from the ethical committee of Uludag University review board. Due to the retrospective nature of the study, informed consent was not required.
3.2. Computed Tomography Technique
CT examinations were performed after intravenous administration of contrast medium, which was injected by hand in the first 21 patients, and by using a power injector in the remaining 62 patients afterward. The dose of contrast medium was 1.5 - 2 mL/kg.
In suspected pulmonary TB cases, contrast medium was used since children have scarce mediastinal fat causing less tissue contrast that limits accurate evaluation of mediastinal lymphadenopathies (16, 18). Additionally, contrast medium would help to reliably differentiate lymph nodes from normal vessels (5). For the first 21 patients, a single-detector helical CT scanner (Emotion; Siemens Medical System; Siemens, Germany) was used with the following parameters: 120 kV, 80 - 140 mA, 5 - 8 mm slice thickness, and 1: 1 or 1.5: 1 pitch. CT scans were obtained with 16 and 64 row multidetector CT scanners (Somatom Perspective 16 with 0.75-mm collimation; Somatom Definition AS 64 with 0.6-mm collimation; Siemens Healthcare, Forchheim, Germany) in the remaining 18 and 44 patients, respectively. The exposure settings were adjusted to patient size (range, 80 - 120 kVp, and 35 - 190 mAs).
CT scan results were interpreted by two experienced pediatric radiologists with consensus. The CT images were evaluated for the presence of LAPs, the specific location of LAPs, according to the International Association for the Study of Lung Cancer (IASLC) lymph node map (19), the presence of calcification within LAPs, the contrast enhancement pattern of LAPs, and concomitant pleural and parenchymal findings. Lymph nodes with a size ≥ 5 mm in the short axis were accepted as abnormal. All of the measurements were performed in the axial view.
3.3. Statistical Analysis
The Shapiro-Wilk test was used to assess whether the variables followed a normal distribution. Variables were reported as median (minimum: maximum) values with mean ± standard deviation. The Mann-Whitney U test, chi-square test, and Fisher’s exact test were used for between-group comparisons. The SPSS software (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.) was used for performing statistical analysis, and P < 0.05 was set for statistical significance.
4. Results
The study cohort included 45 children with TB, 21 G (46.6%) and 24 B (53.3%), with the mean age of 95.27 ± 65.8 months (range, 4-206 months), and 38 children with CAP, 19 G (50%) and 19 B (50%) with the mean age of 74.34 ± 45.79 months (range, 4 - 192 months). There was no statistical difference between the two groups in terms of sex and age (P > 0.05).
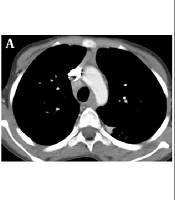
Tuberculosis was bacteriologically confirmed by smear positivity for acid-fast bacilli or culture positivity for M. tuberculosis in 13 (28.8%) patients. The remaining 32 (71.1%) patients were categorized as probable TB, according to NIH categorization (20). The used criteria for the diagnosis of TB are summarized in Table 1. All patients with TB (100%) had at least one mediastinal or hilar lymph node involvement on CT, and 41 (91.41%) of these patients had multi-nodal LAPs (Table 2) (Figure 1). Of the 38 patients with CAP, 36 (94.70%) had at least one mediastinal lymph node involvement on CT, and 35 (97.20%) had multi-nodal LAPs (Figure 2). There was no significant difference between the two groups according to the incidence of lymph node and multi-nodal involvement (P > 0.05).
| Variables | Number of Patients (n = 45); No. (%) |
|---|---|
| Confirmed TB | 13 (28.9) |
| Probable TB | 32 (71.1) |
| Documented exposure to TB | 20 (44.4) |
| Culture positivity for TB and/or smear positivity for AFB | 13 (28.8) |
| Clinically relevant sign or symptom of pulmonary TB | 45 (100) |
| Positive tuberculin skin test (> 15 mm) | 30 (66.6) |
| Positive QuantiFeron test | 11 (24.4) |
| Response to anti-TB therapy | 45 (100) |
| Chest radiologic findings consistent with TB | 45 (100) |
Abbreviations: TB, tuberculosis; AFB, acid-fast bacilli.
| Variables | Group I (n = 45) | Group II (n = 38) | OR (95%CI) | P-Value |
|---|---|---|---|---|
| Lymph node involvement | 45 (100) | 36 (94.70) | NA | 0.401 b |
| Variables | Group I (n = 45) | Group II (n = 36) | OR (95% CI) | P-Value |
| Multiple sites involvement | 0.29 (0.03 - 2.34) | 0.319 c | ||
| Total | 41 (91.41) | 35 (97.20) | ||
| Median (min-max) | 3 (1 - 6) | 3 (0 - 6) | ||
| Mean ± SD | 3.36 ± 1.33 | 3 ± 1.21 | ||
| Site of nodal involvement | ||||
| Paratracheal | 26 (57.80) | 25 (65.80) | 0.71 (0.79 - 1.74) | 0.455 d |
| Prevascular | 0 | 0 | NA | NA |
| Subaortic | 7 (15.60) | 2 (5.30) | 3.32 (0.65 - 17.03) | 0.170 b |
| Paraaortic | 3 (6.70) | 3 (7.90) | 0.83 (0.16 - 4.39) | > 0.99 b |
| Precarinal | 5 (11.1) | 2 (5.30) | 2.25 (0.41 - 12.34) | 0.445 b |
| Subcarinal | 35 (77.80) | 30 (78.90) | 0.93 (0.33 - 2.67) | 0.898 d |
| Paraesophageal | 13 (28.90) | 5 (13.20) | 2.68 (0.86 - 8.40) | 0.083 d |
| Pulmonary ligament | 4 (8.90) | 1 (2.60) | 3.61 (0.39 - 33.77) | 0.369 b |
| Right hilar | 36 (80) | 26 (68.40) | 1.84 (0.68 - 5.02) | 0.227 d |
| Left hilar | 24 (53.30) | 20 (52.60) | 1.09 (0.46 - 2.57) | 0.949 d |
Abbreviations: NA, not available; CI 95%, confidence interval.
a Values are expressed as No. (%) unless otherwise indicated.
b Fisher’s exact test.
c Mann-Whitney U test.
d Chi-square test.
Six-year-old patient with community-acquired pneumonia. Contrast-enhanced CT scans reveal enlarged lymph nodes in right paratracheal in (A) and subcarinal and right hilar areas in (B). There are right lower lobe consolidation and right-sided pleural effusion on oblique axial reformatted image. Fluid bronchograms and CT angiogram sign are seen within the affected area (C).
The most frequent lymph node enlargement in patients with TB was seen in the right hilar position (n = 36, 80%), followed by subcarinal (n = 35, 77.80%), paratracheal (n = 26, 57.80%), and left hilar location (n = 24, 53.30%). The most frequent location for LAP in patients with CAP was the subcarinal (n = 30, 78.90%), followed by right hilar (n = 26, 68.40%), right paratracheal (n = 25, 65.80%), and left hilar location (n = 20, 52.60%). No statistically significant difference was found between the two groups in the distribution of lymph nodes by stations. The mean involved lymph node station for one case in total was 3.36 (range, 1 - 6) in patients with TB and 3 (range, 0 - 6) in patients with CAP. Detailed involvement of lymph node stations of patients with TB and CAP is summarized in Table 2. Although the frequency order was different, the stations with the most frequent involvement were similar in both groups.
In the comparison between the two groups, lymph node size was larger in the TB group (P = 0.04) (Table 3). The mean size was 9.9 mm in patients with TB and 8.6 mm in patients with CAP (Table 3). Comparisons made according to the most common lymph node stations revealed that the mean lymph node size in the paratracheal station was larger in the TB group (12 mm) than in the CAP group (8 mm) (P = 0.004).
| Size (mm) | Group I (n = 45) | Group II (n = 36) | P-Value |
|---|---|---|---|
| Overall | 0.042 a | ||
| Median (min - max) | 10 (5 - 22.58) | 8.31 (6.10 - 15) | |
| (Mean ± SD) | 9.93 ± 3.53 | 8.58 ± 1.88 | |
| Paratracheal | 0.004 a | ||
| Median (min - max) | 10.45 (5 - 35) | 7.60 (5 - 15) | |
| (Mean ± SD) | 11.97 ± 6.25 | 8.05 ± 2.29 | |
| Right hilar | 0.230 a | ||
| Median (min - max) | 8.40 (5 - 25) | 7.10 (5 - 11.60) | |
| (Mean ± SD) | 9.83 ± 4.89 | 7.67 ± 2.03 |
a Mann-Whitney U test.
On contrast-enhanced CT scans, two patients with TB had LAPs with low-density centers and peripheral rim-like enhancement, whereas this feature was not identified in any patients with CAP. In patients with TB with peripheral rim-like enhanced LAP, one patient had a lymphadenopathy in the subcarinal area with a diameter reaching up to 15 mm, and the other with a diameter reaching up to 18 mm in the right hilar area. Lymph node calcification was seen in one patient with TB.
Lung parenchymal involvement was reported in 34 patients (75.6%) with TB. In contrast, it was found in all patients with CAP (100%) as expected. Pleural findings, such as effusion or thickening, were seen in 12 patients (26.7%) with TB and 15 patients (41.7%) with CAP (P > 0.05). Ten (22%) patients with TB had mediastinal and/or hilar lymphadenopathies without any concomitant parenchymal or pleural findings.
5. Discussion
In the present study, all patients with pulmonary TB showed mediastinal lymph node enlargement on CT. The most frequent location for LAP was the right hilar, followed by the subcarinal, right paratracheal, and left hilar. Of the 45 patients with TB, 41 had multiple site involvement.
To date, several studies have evaluated the CT features of mediastinal lymph nodes in pediatric pulmonary TB (5, 13-16). The total number of patients in these studies ranged from 37 to 100. Eighty-three to 97% of the patients had mediastinal lymph node involvement. Combining the results of the present study with those from previous studies suggests that mediastinal lymph node involvement is a prevalent entity in primary pulmonary TB in children and is seen in more than 80% of the patients. In addition, the paratracheal, hilar, and subcarinal areas are the most common locations of LAP in varying orders, and also multiple sites lymph node involvement is a common finding.
Studies (10, 11) that evaluated the added value of chest CT to non-contributory CXR in pediatric complicated CAP did not report any data about the mediastinal LAP and only investigated the parenchymal, pleural, and pericardial features of CAP. Mediastinal lymph node enlargement is not known as a significant feature of CAP; on the contrary, it suggests alternative diagnoses, most likely TB in children. A few studies performed in adults with complicated CAP (21-23) reported that mediastinal LAP was a frequent CT scan feature. To the best of our knowledge, no study in the English literature has assessed the presence of mediastinal LAPs in pediatric cases of CAP. A single study compared the CT findings of pediatric pulmonary TB and CAP, recorded data about mediastinal lymph node involvement in CAP cases (17). The authors reported that children with TB had a higher proportion of mediastinal lymph node involvement than children with CAP. They observed hilar or mediastinal lymph node enlargement in 11 and 10 of 26 patients with TB and two and four of 20 patients with CAP, respectively. However, they did not exhaustively describe the locations of the LAP in both groups (17). Notably, in the present cohort, 36 of 38 (95%) children with CAP had mediastinal LAP, and 35 of these patients had multiple site involvement. The most frequent site for LAP in patients with CAP was the subcarinal, followed by right hilar, right paratracheal, and left hilar. There was no statistically significant difference between the two groups in terms of the incidence of lymph node and multiple site involvement and the distribution of lymph nodes by stations. However, the lymph node size was larger in the TB group. According to the lymph node stations, the diameter of the paratracheal lymph nodes in children with TB was larger than those in children with CAP. For other stations, there was no statistically significant difference between the groups.
Apart from the frequency of lymph node involvement in primary pulmonary TB, identifying the characteristics of lymph nodes on CT is also essential. Distinct contrast-enhancement patterns have been described for TB LAP, and the peripheral rim-like enhancement due to central caseous necrosis is a typical finding (24). Kim et al. (13) documented that 71% of pediatric patients with primary pulmonary TB had LAP with rim-like enhancement. Andronikou et al. (5) showed that 67 of 92 patients with primary pulmonary TB had LAP with rim-like contrast enhancement; however, specific enhancement was ‘ghost-like’ ring enhancement rather than discreet ring-enhancing with a low-density center. In a study by Mukund et al. (15), of patients with mediastinal LAPs, 52% had heterogeneous, 34% homogeneous, and 14% rim-like contrast enhancement. Buonsenso et al. (16) reported 16% ring enhancement in their patients.
The proportion of patients with LAP showing rim-like contrast enhancement was considerably low in the present study, and only two (4%) of 45 patients had this type of enhancement on CT. The rest of the patients with TB and patients with CAP had LAPs with slight homogeneous enhancement, and no significant difference was observed between the groups in terms of contrast-enhancement patterns of lymph nodes.
Previous studies reported the prevalence of lymph node calcification ranged from 9% to 28% (5, 13, 15, 16). In the present study, only one (2%) patient with TB had lymph nodes with calcification, which appeared as specks. The incidence of lymph node calcification increases with treatment in patients with TB. In a study (25) performed on adult patients with mediastinal TB LAPs, according to biopsy and culture results, the disease was divided into active and inactive phases. Calcifications within the nodes were seen in 19% of patients with active disease and 83% of those with inactive disease (25).
The low proportion of LAP with rim-like contrast enhancement and with calcification in the TB group in the present study may be attributed to the small size (mean, 9.93 mm) of the lymph nodes, and also the early detection of the disease because of the high level of TB awareness and preparedness in our institution because TB is a common disease in our community.
In our TB group, 22% of patients had isolated mediastinal LAPs without other associated parenchymal and/or pleural involvement. It was a significantly higher rate compared to the relevant literature (13, 16). The presence of LAP without parenchymal involvement may be a good indicator for diagnosis of pulmonary TB in a relevant clinical setting. The main limitation of the present study and the other studies that investigated mediastinal lymph node involvement in pediatric pulmonary TB is the lack of size threshold criteria to identify pathologic mediastinal lymph nodes in children. Some of the studies that investigated lymph node involvement in pediatric pulmonary TB did not mention any cut-off value for lymph node diameter to accept the lymph node as enlarged or pathologic (13, 14, 16). Mukund et al. (15) accepted mediastinal lymph nodes with a diameter of > 1 cm as pathologic. Andronikou et al. (5) first accepted all visible mediastinal lymph nodes as LAP and documented that 92% of patients with primary pediatric TB had LAP. Notably, the ratio of patients with LAP decreased from 92% to 46% when they only accepted mediastinal lymph nodes with a diameter of > 1 cm as pathologic. In the study by Peng et al. (17), in which the authors compared the CT findings of pediatric TB and CAP, the cut-off threshold value to define the mediastinal LAP was determined as > 6 mm.
New scanning techniques and state-of-the-art equipment may make more normal lymph nodes visible. However, the data are very limited regarding the incidentally detected mediastinal lymph nodes in healthy children who undergo chest CT (26, 27). In De Jong and Nievelstein’s study (26), at least one lymph node was found in 115 (96%) of 120 children aged 1 to 17 years, with subcarinal, lower paratracheal, and hilar nodes being the most common. The authors proposed short-axis thresholds of 7 and 10 mm for mediastinal lymph nodes in patients up to and older than 10 years of age, respectively. In the most recent study (27), mediastinal lymph nodes were identified in 81% of 99 children aged 4 to 18 years. Although all lymph nodes measured less than 7 mm, the largest mean diameter was found 4.6 mm, which was at the subcarinal station. Ideally, size criteria for abnormal lymph nodes detected on CT in children should be defined based on pathologic correlates (28). As far as we know, there are no studies in the English literature on this issue. We defined mediastinal lymph nodes as pathologic when their diameter was ≥ 5 mm in the present study. It was likely that we considered some healthy lymph nodes to be pathologic. Nevertheless, the primary scope of the current work was to compare mediastinal lymph node involvement between children with primary pediatric TB and CAP; therefore, we suggest that the defined cut-off value did not adversely affect the reliability of the present study.
There are other limitations that should be acknowledged. First, the sample size in this study was relatively small, particularly in the CAP group. Second, given the retrospective nature of the study, we could not standardize CT equipment and acquisition parameters for CT. Additionally, the main drawback of CT scan is radiation exposure. However, the use of chest CT to assess the suspected pulmonary TB pediatric cases is increasing since it is more sensitive method for detecting lymphadenopathy and an alternative radiologic method is currently absent (16). Third, the pathogen was not identified in most of the CAP cases. However, sputum cultures are difficult to obtain, and blood culture results often do not yield a pathogen in children (9). Finally, the improvement with antibiotics with or without other therapeutic methods suggested an association with bacterial pneumonia.
5.1. Conclusions
In conclusion, the present study showed that although the lymph node size was larger in the TB group than in the CAP group, the mediastinal lymph node involvement pattern on CT is not a discriminative feature for primary pediatric TB because children with CAP may present with similar mediastinal lymph node involvement patterns. However, mediastinal lymph node involvement without parenchymal or pleural involvement on CT is seen in a significant portion of pediatric patients with pulmonary TB. Additionally, rim-like lymph node enhancement and lymph node calcifications are rare findings in primary pediatric TB.