1. Background
Tracheostomy was first observed in Egyptian drawings in 3600 BC and performed frequently during the 1800’s diphtheria epidemic (1, 2). In the 1900’s, due to the development of endotracheal intubation and diphtheria vaccine, the need for tracheostomy was reduced. Between 1970 and 1980 infection related airway obstruction was the most common indication for tracheostomy. With the development of vaccines for upper airway infections and an increase in the number of patients being treated in pediatric intensive care unit, prolonged intubation is now the most common reason for tracheostomy (3-5).
For those patients with an expected intubation period longer than two weeks, tracheostomy is preferred, not only in order to limit the risk of possible intubation related laryngeal trauma (resulting in glottic and subglottic stenosis), but also to decrease the length of hospital stay, the need for sedation as well as the number of health care workers required to take care of the patient (6). Even ın adult patients there is insufficient evidence to establish consensus for timing of the procedure (7). It is known that pediatric patients tolerate intubation for a longer period than adults do. Since there is no certain time for tracheostomy for children after prolonged intubation, there is no established criteria for children, and so each patient has to be evaluated individually (8). Any decision to apply tracheostomy is affected by the predictability of disease course, the experience and equipment of the center, and parental anxiety.
The upper airways are the cause of 50% of airway resistance during inspiration (9). Since the upper airways are by-passed by tracheostomy, for those patients with weaning failure or who have a neurological disease, tracheostomy may be helpful for weaning by decreasing the work of respiration. It may also allow patients with chronic respiratory insufficiency to get mechanical ventilation at home. Hence it decreases the length of stay in pediatric intensive care unit (PICU) and hospital (10).
Nowadays tracheostomy procedures are often performed at bedside without any additional risk of complications (11). Age, cricoid position on the neck of the patient and experience of surgeon are important factors in deciding to choose the place of procedure.
2. Objectives
Here we review our experience with a group of patients who underwent tracheostomy over a 12 year period. We have evaluated the demographics, tracheostomy indications, related complications, decanulation rates and the effect of mechanical ventilation on weaning and the length of stay in PICU.
3. Materials and Methods
This was a retrospective review of 152 pediatric patients who underwent tracheostomy in our PICU between January 2000 and January 2012. Tracheostomy indications were determined by a pediatric intensivist, a pediatric pulmonologist, and an otorhinolaryngologist. Tracheostomy was performed by standard technique, under midazolam, fentanyl at bedside and vecuronium anesthesia or general anesthesia in the operating room.
The medical records of those patients included were reviewed. The age, gender, diagnosis at admission, indications for tracheostomy, complications, mortality rate, length of preoperative stay, length of PICU stay, length of hospital stay, and duration of tracheostomy were all noted.
This study was approved by the ethical committee of Hacettepe university non-interventional clinical research ethics board.
4. Results
A total of 152 patients were included in the study. The mean age of patients was 3.8 years (median 15 months) ranging between 1 month and 17 years. Fifty seven percent of patients were below 2 years of age. The male female ratio was 1.25/1.
Tracheostomy indications were prolonged intubation in 107 (70.4%) patients, upper airway obstruction in 43 (28.3%) patients, and endotracheal intubation failure in 2 (1.3%) patients.
Forty five percent of the tracheostomy procedures were performed at bedside. Younger tracheostomy patients were preferably treated in the operating room (33.46 months vs. 62.8 months, P < 0.05). There was no increased risk of complications on bedside tracheostomy (P = 0.622).
In our institution when all mechanically ventilated patients were analyzed ıt was found that successful extubation was performed within 10 days of mechanical ventilation and patients died within 10.5 days of mechanical ventilation. Whereas the mean duration of mechanical ventilation before tracheostomy was 23.8 days (median 19 days). The minimum time before tracheostomy was 1 day, whereas the maximum was 130 days. There was a negative correlation between patients’ age and the length of mechanical ventilation before tracheostomy (P < 0.01). The younger the patients were, the longer was the duration of mechanical ventilation. Although it has not been confirmed statistically, we have observed that complication rate was higher in patients in whom tracheostomy was performed after averagely 25 days of mechanical ventilation comparing to the procedure when it was performed earlier (52% vs. 43%, P = 0.062).
After tracheostomy 54 (35%) patients weaned and mechanical ventilation was discontinued. Rest of the patients either died or were discharged on mechanical ventilation. Days spent with mechanical ventilation before tracheostomy were significantly less in patients who were weaned compared to those who were discharged (18.6 days vs. 26.7 days, P < 0.05). Patients on mechanical ventilation were followed for mean 20 days before tracheostomy and 10 days after tracheostomy. Tracheostomy indication in 29 (54%) of these patients was linked to airway obstruction, 25 (46%) of whom had prolonged ventilation. Fifteen of them were decanulated after operation.
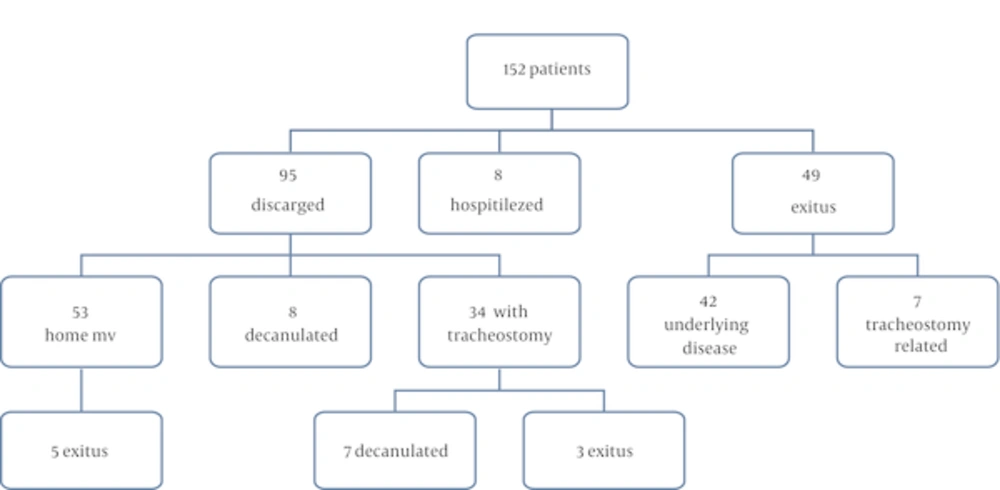
Ninety five of the 152 patients were discharged from hospital, 34 patients with tracheostomy, 8 patients without tracheostomy, 53 patients whose mechanical ventilation requirement continued were discharged with home ventilation. The outcome of all patients can be seen in Figure 1.
We observed 114 (40.1%) complications in 59 patients, 60% of complications occurred in the first week after the tracheostomy procedure. Tracheostomy related complications and its timing can be seen in Table 2. Most of them (14 cases) were due to decanulation and obstruction of the tube (27 cases). During the procedure 11 complications occurred. Cardiopulmonary resuscitation was required in 6 patients and 2 patients died during the procedure. Neither the place of treatment nor the age had any effect on the development of complications (P = 0.701, P = 0.622 respectively).
| Diagnosis | N |
|---|---|
| 75 | |
| 30 | |
| 14 | |
| 20 | |
| 8 | |
| 2 | |
| 3 |
| During Procedure | 0 - 48 h | 48 h-1 w | > 1 w | |
|---|---|---|---|---|
| NA | 9 | 9 | 9 | |
| NA | 2 | 4 | 8 | |
| 5 | 6 | 3 | 4 | |
| 3 | 8 | 3 | 3 | |
| NA | 4 | 1 | 4 | |
| 1 | 3 | 1 | 2 | |
| 2 | NA | NA | 5 | |
| NA | NA | NA | 1 | |
| NA | NA | NA | 1 | |
| NA | NA | NA | 1 | |
| NA | NA | NA | 1 | |
| NA | NA | NA | 2 | |
| NA | NA | NA | 2 | |
| NA | NA | 2 | 3 | |
| NA | 2 | NA | NA |
Abbreviations: NA, not available.
Mortality related with tracheostomy procedure and its complications was 5% (= 9 patients), and overall mortality was 37%. Two patients died during the tracheostomy procedure because of the airway loss, five died during hospital stay before discharge because of ventilation problems, and two died at home after discharge because of decanulation.
5. Discussion
Tracheostomy is a surgical procedure that has been used from ancient times. Its surgical procedure and indications have changed over time. In 1650 the first pediatric tracheostomy was performed because of upper airway obstruction (12). In recent years following the development of intensive care knowledge and equipment ventilation time and the length of PICU stay have been prolonged, and this prolonged ventilation has become the most common reason for tracheostomy.
Although there is consensus that tracheostomy has to be performed in one or two weeks of ventilation in adult patients, early tracheostomy is still in debate (7). But there is no determined time for pediatric patients. According to pediatric intensivists in Canada, the average timing for elective tracheostomy was 21 days, whereas in USA the time for insertion of a tracheostomy tube was in average 14.4 days although it varied significantly in units (4.3 - 30.4 days) (13, 14). In the same survey, factors associated with significant longer time to apply tracheostomy are having cardiac or infectious disease or having two or more re-intubations. The only factor associated with shorter tracheostomy timing was postoperative status. After 2 weeks of intubation the patient should be evaluated for tracheostomy, it should be kept in mind that newborns and infants can tolerate intubation for longer time periods (15). Comparing early and late tracheostomy (within ten days) in adult patients, although early tracheostomy has been reported to have no effect on incidence of ventilator-associated pneumonia among mechanically ventilated adult ICU patients (16). The early tracheostomy patients had lower risk of mortality as well as less time spent in the ICU and higher probability of being discharged from ICU (7). There is no need to wait in patients who are expected to be intubated for long time periods. The decision for tracheostomy is influenced by underlying conditions, co-morbidities, risk of complications, parental factors, size, age and prognosis. Tracheostomy should be considered for patients stabilized on ventilator who may benefit from it.
The main advantages of tracheostomy are patient comfort, effective airway aspiration, a decrease in airway resistance, an increase in patient mobilization, the ability to speak and oral feeding, as well as stable airway (17, 18). It also enables patients to undergo home ventilation. These advantages theoretically lessen the time of ventilation and PICU and hospital stay, but clinical research contradicts this. Although Lesnik and colleagues emphasize that tracheostomy opened in 4 days may ease the weaning of ventilation in blunt traumas, Blot and colleagues reported that tracheostomy in neutropenic patients prolongs hospital stay and the duration of ventilation (18, 19). Rodriguez as Lesnik have agreed that tracheostomy lessens ventilation time, hospital and intensive care stay (20). In concordance with these studies, we found that the weaning is more successful in patients with tracheostomy performed earlier. Furthermore for those patients who were victims of chronic respiratory failure, neuromuscular disease, or congenital heart disease and who will require lifelong mechanical ventilation, tracheostomy allows them to be discharged and put on home mechanical ventilation. Patients requiring home ventilation compose one third of all patients in our study, and tracheostomy enabled 62% of our patients to go their home and grow in their natural environments.
In our institution, tracheostomy was opened after mean 23.8 days of mechanical ventilation. According to the records in our department extubation was performed successfully within ten days of mechanical ventilation and also patients died within 10.5 days of mechanical ventilation. When we compare these results, three weeks is considered to be long enough for the choice of tracheostomy. We also found that after a median time of 19 days of intubation any complication rates increased from 31% to 46%. Successful weaning from mechanical ventilation observed in patients whose tracheostomy procedure performed with a mean 18.6 days of ventilation. These information showed us that within two weeks patients should be evaluated for tracheostomy, in 2 - 3 weeks a decision should be taken, and carried out before 4 weeks of intubation. The decision for tracheostomy should not be made as early as in adult patients. Early tracheostomy should be avoided in pediatric patients but not in patients with high expectation of long term mechanical ventilation requirement such as neuromuscular diseases.
Although tracheostomy procedures have traditionally been performed in operating rooms, nowadays they are often performed at bedside. As reported, Klotz performed a study on 57 pediatric patients and found no difference concerning the development of complications (11). Moreover, a reduction in both cost and time seems to be the real advantage of bedside tracheostomy. Over a ten year period half of the tracheostomy procedures in our department were performed at bedside, and there was no observed increase in the risk of any complication. However, the selection of patients may have had an effect on this result. The age of the patient is an important factor in deciding to choose the site of procedure. We have observed that the mean age of those patients whose tracheostomy was performed in the operating room was lower than that of the bedside group (33.46 months vs. 62.8 months, P < 0.05). Husein and Massick have shown that cricoid palpation is also an important factor in the choice of location (21).
Tracheostomy in pediatric patients has higher complication rates compared to when performed on adults (19). Complications developed in 40% of the patients. There was no increase in the risk of complications in relation to age in our unit. In literature complication rates have a variability of between 30% - 51%. Patients in intensive care units may have a higher risk of complications because of mucosal blood flow disruption due to sepsis, organ failure, shock or pneumonia (22). Severe complications such as cardiopulmonary arrest and pneumothorax have been seen in 5 - 40% (22, 23). The major complication rate after the bedside tracheostomy was reported as 6.4% which has occurred in most series of pediatric tracheostomy (24). Mortality has been reported as being between 0.5 - 3.2% in different studies (25). This ratio increased to 28% when mortality related to primary disease was included. Silva et al found overall mortality to be 52% in long term follow up (26). Tracheostomy related mortality is reported to be as high as 6% (27). As we have observed, the overall mortality was 37%, and tracheostomy related mortality 5%. In our study a high mortality rate was due to problems related to the primary diseases of patients. Different mortality rates in different studies are related to varying mortality rates of primary diseases.
Our study does have certain limitations. It is retrospective from a single center and the fact that some data was not recorded that would enlighten the biased issues such as timing and place of tracheostomy and selection criteria of the patients.
5.1. Conclusions
In our PICU, we have observed that tracheostomy facilitates discharge from PICU, weaning of mechanical ventilation for patients whose weaning has been unsuccessful, and allows patients who need long-term mechanical ventilation support to be discharged and stay at home. Although the timing of tracheostomy has to be determined for each individual patient, three weeks of ventilation requirement seems to be a suitable period for tracheostomy. Tracheostomy can be performed in PICU safely but patient selection should be made carefully.