1. Background
Peripheral intravenous (IV) catheterization is the most common nursing procedure in clinical practice, and it should be mastered by every registered nurse in China. Although this is a basic technique performed by nurses on a daily basis, establishing IV access is still a challenging job for many pediatric nurses because it is not easy to obtain IV access in children, especially in neonates. Some of the challenges are unique to this population.
There are several published studies addressing successful IV catheterization. A 2015 study reported a first-attempt success rate of 85% with a guidewire-associated peripheral venous catheter (GAPIV) versus 22% with the conventional peripheral venous catheter. A second attempt was required for 62% of patients with the conventional catheter compared to 15% with the GAPIV (1). IV placement can be challenging in pediatric patients; the failure rate can reach 47% on the first attempt, and 9% of patients require more than four attempts before peripheral IV access is obtained (2). The data from an emergency department reported a success rate of 67.8% on the first catheterization attempt in pediatric patients (3). Even when interventions such as venous imaging ultrasound are used, two or more attempts are still required for 15% of children to achieve access (4).
Multiple intravenous attempts cause pain, distress, anxiety, and even conflicts with patients. According to a report in China, 31% of conflicts occurring in the outpatient department of the children’s hospital were caused by failed catheterization attempts, out of which 27.3% occurred because of an unskilled puncture (5). Managing difficult venous access or applying instruments can reduce IV placement failure (4, 6, 7). However, there is no objective data from a large sample of successful catheterization attempts and influencing factors in China, and guidelines or standard management methods for this issue are still lacking. Risk factors for first-attempt failures have not been taken into consideration, and there have been no large sample studies analyzing access difficulties.
2. Objectives
The purpose of this study was to detect the success rate of peripheral venous catheterization in Chinese pediatric patients after grade management and to further detect the risk factors for failed insertion on the first attempt.
3. Methods
3.1. Study Design and Population
This is a prospective, clinical observational study conducted between December, 2014 and June, 2015 in Shanghai children’s hospital. This study involved pediatric in-patients who received peripheral venous catheterization and the pediatric nurses who established access for them. Quota sampling was used to enroll patients from the department of internal medicine, the department of surgery, and the pediatric intensive care unit. The patients’ caregivers and nurses were informed of the purpose and contents of the study, and the nurses enrolled in data collections were trained in the methods and rules concerning the information tabulation. The following patients were excluded: outpatients, patients who needed central line access (defined by the treating physician), and patients or parents who refused to participate in the data collection. Based on the procedure designed by Field (8). and the overall staff conditions at our hospital, we outlined the common practice procedure for catheterization as follows: 1, the doctor determines whether to establish venous access or not; 2, the registered nurse performs IV placement; 3, once placement fails, an evaluation is conducted again to determine whether the current nurse should continue the placement; if two attempts fail, members of the vein management group are called to attempt vascular access with or without a vein-imaging instrument. When venous access is difficult to establish, physicians should re-evaluate the need for an IV line and consider alternatives to IV therapy. The procedure mentioned in this study is in accordance with the standards defined by the ethics committee on human experimentation of Shanghai children’s hospital (decision no. 2015R027-F01).
3.2. Study Protocol
Before placement, nurses were asked to document the patients’ information, including two aspects: 1, basic information (age, gender, weight, mental status, vein palpability, vein visibility, etc.) and 2, medical history (history of operation, radiotherapy, and chemotherapy). Post-catheterization data also included two aspects: 1, infusion information (success on the first attempt [yes or no], site of failed/successful puncture, and number of total attempts); 2, nurse information (age, professional title, nurse experience, educational history, self-reported IV placement ability, and whether they received related training [yes or no]). After the documentation was completed, an experienced nurse checked the information tabulation to ensure the integrity and accuracy of the information.
3.3. Measures
Yen’s definition of successful IV catheterization is used in this study (9). An IV attempt begins from the time when the needle first touches the skin, and success is defined as an IV attempt in which the IV is placed well enough at the site that the infusion is able to be injected without swelling at the insertion site.
3.4. Analysis
SPSS 16.0 statistical software was used in this study. Demographic data was expressed as mean ± standard deviation. Outcome frequency was examined using descriptive statistics. A chi-square test or Fisher’s exact test was used for univariate analysis of the collected variables. An independent-samples t-test was used for analyzing differences between groups. Multivariate logistic regression was performed on the patients’ demographic data and on the outcome of the first IV attempt to identify demographic risk factors for failed attempts. The adjusted odds ratios (ORs) of significant variables are reported with 95% CIs. P values of 0.05 or less were considered significant.
4. Results
4.1. Subjects’ Characteristics
There were 1,100 subjects who met the inclusion criteria; 70 were excluded because of refusal, and 14 because of incomplete data, leaving 1,016 patients for analysis. The mean age of patients was 3.28 ± 3.32 years. Of the patients, 610 (60.0%) were male and 406 (40.0%) were female. All the included nurses were female, and their mean age was 27.02 ± 4.70 years (Table 1).
| Characteristics | |
|---|---|
| Patient age, Y | 3.28 ±3.32 |
| Patient weight, kg | 15.87 ±13.25 |
| Gender | |
| Male | 610 (60.00) |
| Female | 406 (40.00) |
| Department | No. (%) of patients |
| Internal medicine | 457 (44.98) |
| Department of surgery | 434 (42.72) |
| Intensive care unit | 125 (12.30) |
| Mental status | |
| Good | 856 (84.25) |
| Common | 131 (12.89) |
| Poor | 29 (2.85) |
| Nurse experience (in years) | |
| ≤ 1 | 256 (25.20) |
| 2 - 4 | 230 (22.64) |
| 5 - 9 | 375 (36.91) |
| ≥ 10 | 155 (15.26) |
| Nurse professional title | |
| Nurse | 610 (60.04) |
| Senior nurse | 373 (36.71) |
| Nurse-in-charge | 33 (3.25) |
| Educational history | |
| Technical secondary school | 48 (4.72) |
| Junior college | 650 (63.98) |
| Undergraduate or above | 318 (31.30) |
4.2. Success Rates
On the first attempt, the common locations were the dorsum of the hand (606, 59.65%), the dorsum of the foot (109, 10.73%) and the saphenous vein (93, 9.15%). A total of 776 (76.38%) catheters from Becton, Dickinson and company were used. A safety catheter was used in 189 (18.60%) subjects on the first attempt. According to the peripheral venous grading system in children designed at our hospital (Table 2), the veins of 381 (37.50%) subjects were at level 0, the veins of 364 (35.83%) subjects were at level I, the veins of 198 (19.49%) subjects were at level II, and the veins of 73 (7.19%) subjects were at level III.
| Content | 0 | 1 | 2 |
|---|---|---|---|
| Age, y | ≥ 3 | 1 - 3 | ≤ 1 |
| Combination | Good | Average | Poor |
| Visible | Visible | Vague applied tourniquets | No visible applied tourniquets |
| Palpable | Palpable | Vague applied tourniquets | No palpable applied tourniquets |
| Circulation | Good | Average | Poor |
aGrades: level 0: 0 - 2 score; level I: 3 - 4 score; level II: 5 - 7score; level III: 8 - 10 score.
The success rate of the first attempt was 86.02%, which decreased to 67.61% on the second attempt. Up to 13.98% of patients required two or more attempts to establish peripheral venous access, and 4.53% of patients needed three or more attempts. This shows that 1.21 sticks on average are required per successful placement (Table 3). No patients in our sample underwent insertion of a peripherally-inserted central catheter (PICC), an intraosseous (IO) device, or a central venous catheter (CVC).
| Results | N | Rate, % |
|---|---|---|
| Success/failure on the first attempt | 874/142 | 86.02/13.98 |
| Success/failure on the second attempt | 96/46 | 67.61/32.39 |
| Success within two attempts | 970 | 95.47 |
| Attempt count ≥ 3 times | 46 | 4.53 |
| Total no. of attempts | 1,226 | |
| Catheters per IV attempt | 1.21 | |
4.3. Influencing Factors
From the results of the univariate analysis on all variables, we can see that the success rate of the first attempt was influenced by patient age, weight, department, mental status, whether communications were effective or not, venous condition, and nurse age, experience, and professional title. A multivariate logistic regression was used to identify several independent risk factors for failed catheterization on the first attempt. The following patients were found to be at greater risk: younger children, patients admitted to the intensive care unit, patients with veins at level 0 or level I, and patients being served by nurses with experience ranging from two to four years or more than 10 years (Table 4).
| Variable | Control Group | Comparison Group | OR | 95% CI | P Value |
|---|---|---|---|---|---|
| Patient age | Continuous variables | 1.124 | 1.043 - 1.220 | 0.003 | |
| Department | ICU | Internal medicine | 2.890 | 1.584 - 5.265 | 0.001 |
| Department of surgery | 2.206 | 1.154 - 4.210 | 0.015 | ||
| Vein level | Rank variable | (level 0, I, II, III) | 2.305 | 1.827 - 2.913 | < 0.001 |
| Nurse experience, y | ≥ 10 | ≤ 1 | 1.256 | 0.639 - 2.440 | 0.517 |
| 2 - 4 | 1.344 | 0.723 - 2.463 | 0.350 | ||
| 5 - 9 | 2.347 | 1.325 - 4.167 | 0.004 |
5. Discussion
Peripheral IV access is routinely required for the diagnosis and treatment of many patients, and peripheral IV placement technique should be mastered by every registered nurse in China. However, there is still little information on the success rate of peripheral IV insertion in pediatric hospitals. Multiple IV attempts not only compromise the patients’ trust and confidence in the nursing staff and/or the hospital but also cause pain and complications for patients. For these reasons, new technology for peripheral IV catheterization has been applied to improve success rates and to avoid the problems associated with placement (7, 10-12). According to the reports, the success rate of peripheral IV catheterization with the traditional method was between 33% and 70.6%, whereas the ultrasound-guided peripheral IV access resulted in a success rate of 80.5% - 97% (11, 12). The ultrasound-guided peripheral IV access program was also reported to improve the placement of central venous catheters (13).
Our results indicate an 86.02% success rate on the first attempt at freehand peripheral IV placement, which decreases to 67.61% on the second attempt. Therefore, when the first attempt fails, a new evaluation of the patient should be performed, and whether to adjust the performer should be considered. We made a guideline by which only two insertion attempts can be placed in the same subject by any one of the nurses. In emergency situations, successful peripheral IV access is achieved within two attempts in 92% of adults (14) and in 86% of children (15). The success rate within two attempts is 95.47% in this study, which is higher than that in the reports mentioned above, meaning that 4.53% of patients require three or more attempts before success. Under these circumstances, vein management group members should be called to perform the insertion.
Several studies have attempted to predict the risk factors associated with difficult venous access. Obesity, diabetes mellitus, dehydration, and an unskilled performer may affect the success rate of the first attempt (8, 16). In our study, univariate analysis of 13 variables revealed that only nine factors (patient age, weight, department, mental status, whether communications are effective or not, venous condition, and nurse age, experience, and professional title) are significantly associated with the first-attempt success rate of peripheral IV access. In order to further explore the risk factors for failed IV insertion on the first attempt, we define whether success or failure on the first attempt is a dependent variable (1 = yes, 0 = no), define the nine factors as independent variables, and fit the non-conditional logistic regression analysis. Logistic regression analysis of nine proposed predictor variables reveals that only four factors (patient age, department, and venous condition and nurse experience) are significantly associated with the first-attempt success rate of peripheral IV access (Table 4). The average age in the success group on the first attempt is 3.46 ± 3.18, whereas it is 2.51 ± 2.93 in the failed group (P < 0.001). A history of previous stays in the intensive care unit (ICU) has a greater association with failed peripheral IV insertion than a history of general ward visits (χ2 = 17.632, P < 0.001). This demonstrates a higher success rate in patients with good venous condition (level 0, level I) (95% CI: 1.816 - 2.913, P < 0.001).
Among the six operator (nurse) variables evaluated, only nurse experience proved to be statistically associated with peripheral IV placement.
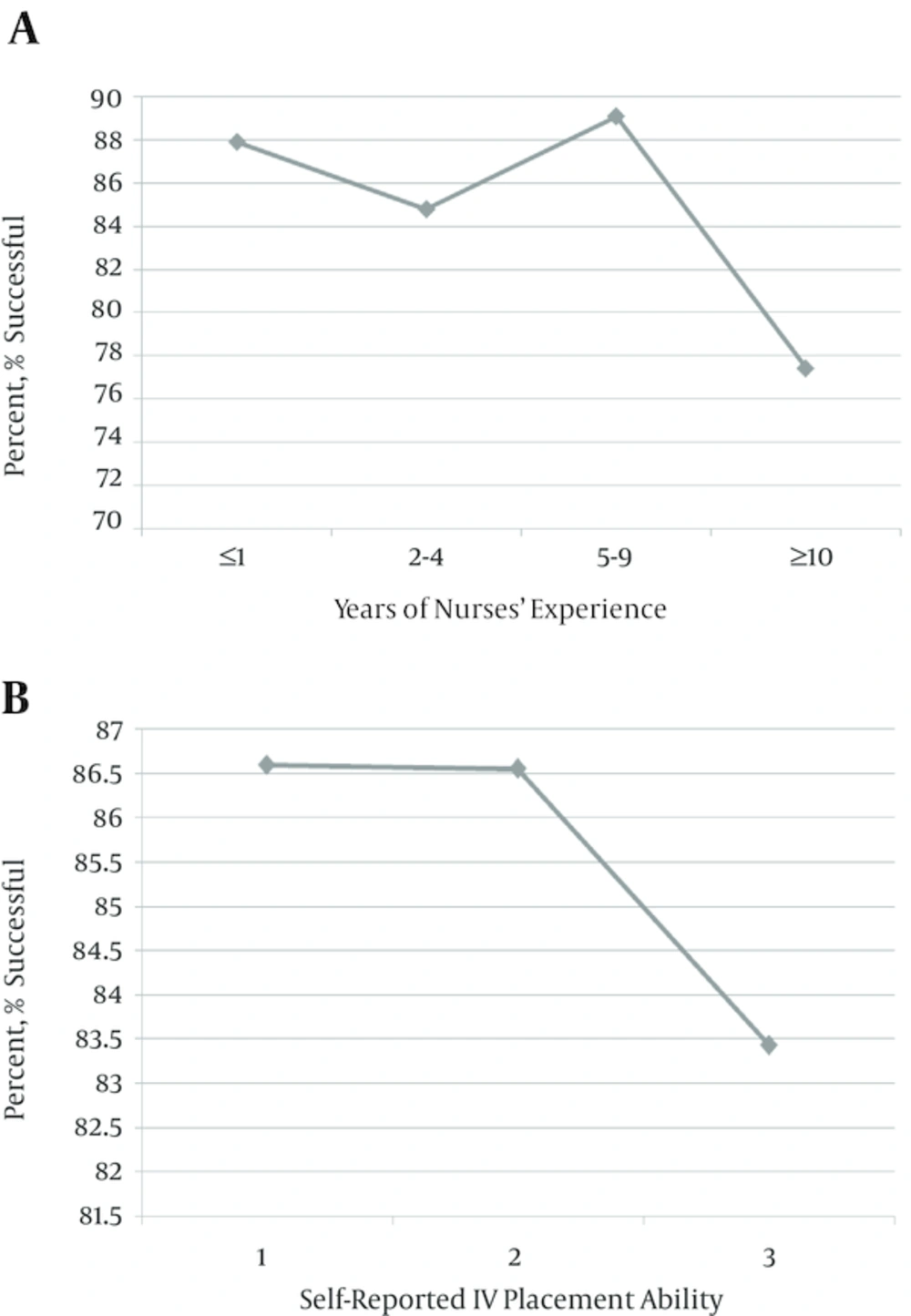
It is widely assumed that nurses with more experience in placement can achieve a higher success rate. However, contrary to our expectations, nurses with between five and nine years of experience had the highest (89.07%) success rate in our study, higher than that of the nurses with less than one year (87.89%), two to four years (84.78%), and greater than 10 years (77.42%) (P < 0.01) of experience. This may be related to the fact that experienced nurses often perform the difficult venous access attempts and assume responsibility for venous consultation (Figure 1A). In this study, the opportunities of the nursing staff to establish IV access varied according to their experience. It is an effective strategy to empower each nurse to do meaningful work and to improve their organizational commitments. There is a positive relationship between nurse experience and first-attempt success rates. Nurse managers should consider how to apply this method, as well as measures for improvement.
According to the report, higher levels of self-reported IV placement ability are always associated with a higher success rate of IV insertion (17). In this study, although the nurses who self-identified as skilled in IV placement ability achieved the highest success rate (86.59%), higher than those of the other two groups (Figure 1B), this difference was not found to be statistically significant. This indicates that nurses may have inaccurate self-assessment abilities in this context, especially less-experienced nurses. Therefore, we propose objective variables for more accurate evaluation of nurse venipuncture skill.
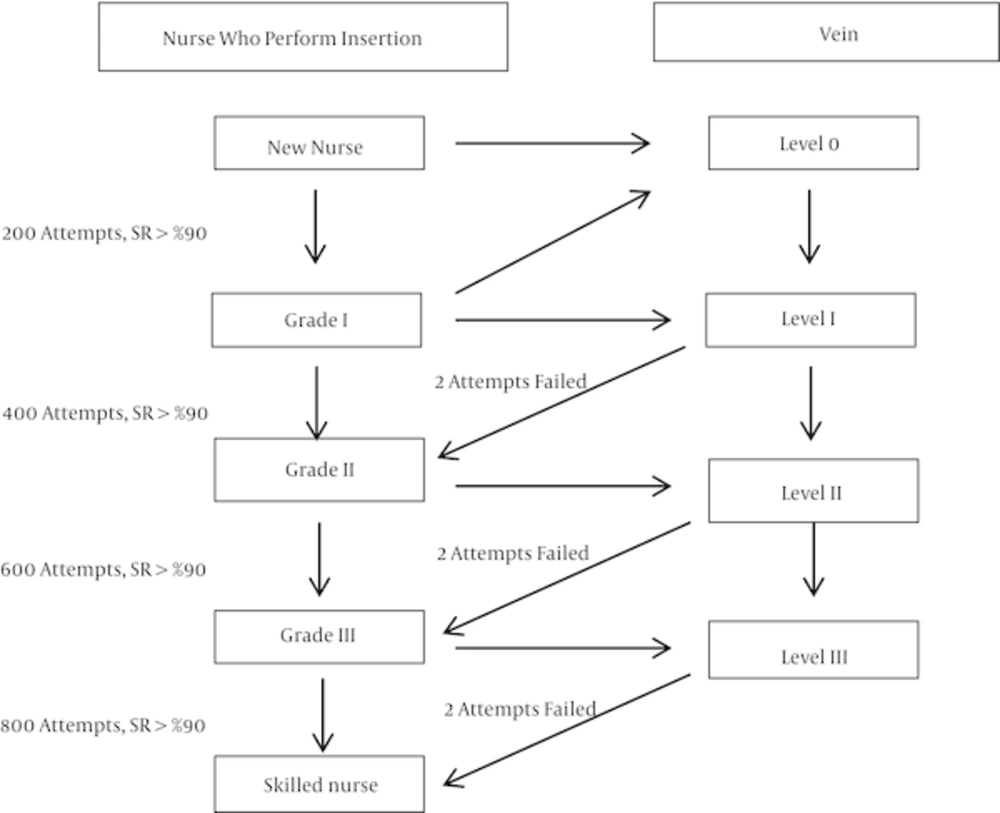
The management of peripheral IV insertion is not standardized (18). Identifying the potentially difficult venous access cases at an early stage is important for nurses to adjust their approach and staff, which can contribute to improving the success rate. There are many methods to manage peripheral IV insertion, such as anesthetizing the peripheral IV site to reduce patient pain and discomfort (19-21) using an assistive device to improve vein visualization to achieve a higher success rate (22-26) applying diagnostic tests to confirm correct intravascular placement (27) and local warming (28). Considering the fact that each registered nurse can establish peripheral IV access for pediatric patients, we proposed grades to measure the venipuncture skills of pediatric nurses (Figure 2). We assigned appropriately skilled nurses according to the peripheral vein grade of each case. Each nurse should be examined by experienced nurses from the vein management group and by the head-nurse to evaluate their success rate for first attempts at insertion on a given grade of vein. When the success rate is above 90%, a nurse should be considered qualified to perform insertions for the next level of vein.
5.1. Limitations
The major limitation of this study is that it is an observational study. Although the sample size is sufficient, selection bias may have occurred due to the fact that some patients refused to participate, although refusing to participate would likely be random. Meanwhile, all the subjects were enrolled in a single pediatric hospital. Therefore, more studies from multiple centers in this field using a prospective, randomized study design are recommended. The second limitation is that patient diagnosis, skin condition, and nutrition condition were not analyzed for risk factors in this study. In future studies, these factors should be internalized in the study design for analysis.
5.2. Conclusions
The findings of this study provide important information about the success rate of peripheral IV access and risk factors for failed placement on the first attempt in pediatric patients in China.
Grade management of veins and improving nurse venipuncture skill are feasible measures in pediatric patients. In our investigation, the success rate of the first attempt was higher than in previously reported data, but it significantly decreased on the second attempt. This illustrates that grade management can be used to guide the ordering of nurses to achieve timely vascular access and a high success rate on the first attempt. This study also establishes that management measures should be revised in the future for standard peripheral IV insertion in pediatric patients, especially when multiple intravenous attempts are needed. The risk factors for failed access on the first attempt include patient age, department, and venous condition and nurse experience, which should be considered before IV insertion.