1. Background
Considered the second most common cyanotic congenital heart disease [CHD], D-looped transposition of the great arteries (D-TGA) consist of 5% - 7% of all CHDs (1), 860 cases of which are diagnosed each year in the united states (2). The arterial switch operation (ASO) is the surgical procedure of choice for the TGA. Jatene and colleagues first introduced this operation in 1975 (3), considerable progress have been achieved in surgical techniques and perioperative management since then. The anatomic correction of the TGA at the ventricular or arterial level, with or without coronary transfer (1, 4) is the cornerstone of ASO. This is one of the most complex cardiac surgeries, with coronary artery transfer being the most important factor determining the success of the surgery (5). Despite major improvements of the procedure, it seems that there is still room for improvement.
2. Objectives
This study aims to investigate the outcomes of ASO operated by a single surgeon and assess the accuracy of echocardiography in identifying the coronary artery pattern before the ASO, this may lead to a better familiarization with ASO.
3. Methods
3.1. Study Design and Data Collection
This study was performed as a retrospective study by reviewing the operative and postoperative case notes from March 2015 to March 2018 in Children’s Medical Center, Tehran, Iran. Echocardiographic reports, clinical inpatient notes and surgical notes were assessed. All of the patients were assessed by echocardiography done by one physician using Vivid E9 General Electric Ultrasound machine. The coronary artery pattern identified by echocardiography prior to the surgery was recorded. The usual coronary pattern was defined as originating from left anterior descending artery (LAD) and left circumflex artery (LCX) from first aortic coronary sinus and right coronary artery (RCS) from the second one. First coronary sinus is the closest one to the surgeon. The anatomic complications (including different valvar disturbances, myocardial stunning, presence of the effusion and endocarditis), arrhythmia (including atrial flutter, cardiac block and ventricular tachycardia) and neurologic complications (including intracranial hemorrhage (ICH], intraventricular hemorrhage (IVH), subarachnoid hemorrhage (SAH), seiz (ICU) stay and lactate level before and after surgery were recorded, as well.
3.2. Simple vs. Complex, IVS vs. VSD
The patients were classified as the simple and complex DTGA and those with and without intact interventricular septum (IVS). DTGA with atrial septal defect (ASD), patent ductus arteriosus (PDA) and small ventricular septal defects (VSD) were considered as the simple DTGA and those with other concomitant cardiac anomalies were considered as the complex DTGA. Patients in whom VSD closure, besides the ASO, was performed, were considered as the patients without intact IVS and others who did not undergo VSD closure, were considered as intact IVS.
3.3. Surgical Method
ASO is defined as the main surgical solution for the complete TGA. The procedure includes detachment of the native aortic and pulmonic roots and replace them with each other. The coronary arteries are harvested and replaced to the neoaortic root. ASO can be performed in one-stage or two-stage method according to the left ventricular mass obtained by echocardiography. For the two-stage method, one can use pulmonary artery banding, septectomy with or without Blalock-Taussig shunt (left ventricular training method). In the current study all surgeries were performed by a single surgeon, using the same surgical technique in all patients.
3.4. Ethical Consideration
This study was approved by the Research Deputy and the Ethics Committee of Tehran University of Medical Sciencess on April 22, 2019 (Reference number: IR.TUMS.CHMC.REC.1398.017).
3.5. Statistical Analysis
All data were analyzed using SPSS version 22. The quantitative variables were expressed by mean and standard deviation and the qualitative variables by number and percent. For parametric variables, independent samples t-test and for non-parametric variables, Mann-Whitney test was applied. Chi-square test was used to evaluate the difference between two qualitative variables. A P value below 0.05 was considered statistically significant.
4. Results
4.1. Demographic and Patients’ Features
One hundred twenty-five patients, known case of DTGA, were recruited in the study. The mean age and weight of the patients were 29.09 (1 - 80) days and 3.5 (0.4 - 9.7) kilograms. 80 (64%) patients were male and 45 (36%) were female. The average CPB time and ICU stay were 202.73 (110 - 310) minutes and 11.2 (1 - 70) days. Intact IVS was present in 111 (88.8%) patients. Simple DTGA and complex DTGA were observed in 105 (84%) and 20 (16%) subjects. the mortality rate among our patients was 4% (5 patients). Patients with intact IVS had a higher age, compared to those without intact IVS (P value = 0.031). Five patients underwent this type pf surgery, with the average age and weight of 162 (± 105.21) days and 5758.88 (± 3485.219) grams.
4.2. Anatomic Complications
The anatomic complications and arrhythmia were present in 92 (73.3%) and 32 (12.8%) patients. The cardiac complications (including anatomic and arrhythmic complications) are summarized in Tables 1 and 2. Rate of anatomic complications did not differ between different genders and patients with and without intact IVS (P value = 0.833 and 0.999), similar to arrhythmic complications (P value = 0.579 and 0.18). The prevalence of AR was not associated with the type of DTGA (P value = 0.389), but AR was more prevalent in patients with intact IVS (P value = 0.011). The rate of anatomic complications was not associated with the type of DTGA and intact IVS (P value = 0.999 and 0.999).
| Anatomic Complications | Number (Percent) |
|---|---|
| Mild AS | 3 (2.4%) |
| Trivial PR | 5 (4%) |
| Mild PR | 56 (44.8%) |
| Trivial AR | 16 (12.8%) |
| Mild AR | 34 (27.2%) |
| Moderate AR | 2 (1.6%) |
| Mild PS | 5 (4%) |
| Mild LPA stenosis | 1 (0.8%) |
| Mild PPS | 3 (2.4%) |
| Endocarditis | 1 (0.8%) |
| LV failure | 1 (0.8%) |
| Moderate left pleural effusion | 1 (0.8%) |
| Tamponade | 1 (0.8%) |
| Mild myocardial stunning | 5 (4%) |
| Global myocardial stunning | 1 (0.8%) |
| Arrhythmic Complications | Number (Percent) |
|---|---|
| Atrial flutter | 1 (0.8%) |
| Long QT syndrome | 1 (0.8%) |
| Paroxysmal supraventricular tachycardia | 2 (1.6%) |
| Venkebakh | 1 (0.8%) |
| Right bundle branch block | 8 (6.4%) |
| Sick sinus syndrome | 1 (0.8%) |
| Ventricular tachycardia | 2 (1.6%) |
4.3. Coronary Artery Pattern
The observed coronary pattern before the surgery and during the surgery is summarized in Table 3, which indicates the sensitivity and specificity of echocardiography for diagnosis of the coronary pattern is 42.9% and 88.1% (P value = 0.052).
| Coronary Artery Pattern | Before Surgery (by Echocardiography) | During the Surgery (Eye Ball Assessment) |
|---|---|---|
| Usual | 108 (86.4%) | 118 (94.4%) |
| Unusual | 17 (13.6%) | 7 (5.6%) |
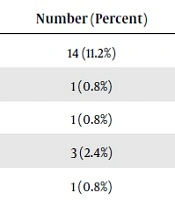
4.4. Neurologic Complications
Neurologic complications were observed in 20 (16%) subjects (Table 4). The rate of neurologic complications did not differ significantly between different genders, with and without intact IVS and different types of DTGA (P value = 0.999, 0.123 and 0.999). Patient with simple and complex DTGA did not differ significantly regarding the rate of seizure and different types of hemorrhage (including ICH, IVH and SAH) (P value = 0.999 and 0.198). The same changes were observed between patients with and without intact IVS (P value = 0.223 and 0.957).
| Neurologic Complications | Number (Percent) |
|---|---|
| Seizure | 14 (11.2%) |
| Intracranial hemorrhage (ICH) | 1 (0.8%) |
| Intraventricular hemorrhage (IVH) | 1 (0.8%) |
| Subarachnoid hemorrhage (SAH) | 3 (2.4%) |
| Chorea | 1 (0.8%) |
4.5. CPB Time, ICU Stay, Lactate Level and Mortality
The length of ICU stay was not associated with the type of DTGA and presence of intact IVS (P value = 0.944 and 0.928). The average CPB time among patients with simple and complex DTGA was 195.85 (± 32.48) and 237.8 (± 39.48) minutes. The average CPB time among patients with and without IVS was 199.27 (± 34.96) and 299.43 (± 42.54) minutes. The CBP time was not associated with arrhythmic complications (P value = 0.084), complex DTGA had more prolonged CPB time (P value < 0.0001); furthermore, patients without intact IVS had more prolonged CPB time than those with intact IVS (P value = 0.004).
Mortality rate did not differ between different genders and patients with and without intact IVS, types of DTGA (P value = 0.999, 0.999 and 0.999). Mortality rate was not associated with the unusual coronary pattern observed during the surgery and arrhythmic complications (P value = 0.999 and 0.999). The average lactate level before and after surgery was 2.62 (± 2.11) and 7.17 (± 9.8). The lactate level after surgery was significantly higher than lactate level before the surgery (P value < 0.0001).
5. Discussion
Society of Thoracic Surgeons has determined the major morbidities of the ASO as the renal failure, neurological complications, arrhythmia, phrenic nerve injury and unplanned re-operation before discharging from the hospital (6). As was observed in the current study, 16% of the patients had neurologic complications and 12.8% had arrhythmia. The optimal age of surgery was suggested 3 days (7) or within the hours following the birth (8). The average age of our patients was 29 days, our center is a tertiary referral center, delayed surgical time in performing ASO is due to referral interval, from the diagnosis time to the referral time. ASO in TGA/intact IVS after 3 weeks of age has not been recommended, due to deconditioned left ventricle which is not able to support the systemic circulation (9), although some studies have indicated that ASO is useful for TGA/intact IVS even beyond 1 month of age (10). Our study also indicated that patients with TGA/intact IVS had a lower age, compared to those without intact IVS. Weight is one of the other challenging issues; low birth weight is associated with increased mortality (11, 12). Infection, renal failure, respiratory diseases, neurological problems are associated with lower weights (13). Delayed surgery dose not result in better outcomes (14), recent studies demonstrate that the success of the surgery performed in lower weights is comparable to that in normal weights (15). The average weight at the time of the surgery in the present study was 3.5 kg with the range of 2.4 - 9.7, indicating the study included both lower weights and higher ones. We assume that performing surgery earlier with a lower weight does not lead to higher complications; therefore, ASO is suggested as soon as possible.
One-third of TGA patients have VSD (12, 16). In the current study, VSD was observed in 11% of patients. Some studies have indicated that patients with VSD have higher mortality (12, 17, 18), Quaegebeur et al. in 1986 reported the mortality rate of 12% in ASO/intact IVS and 18% in ASO/VSD (18). Our study did not support this, mortality rate in patients with and without intact IVS did not differ significantly (P value = 0.999). Complex TGA, TGA/VSD, TGA/DORV, coarctation of the aorta are the predictors of the poor outcomes (19, 20); however, some studies did not support the complex TGA to be a risk factor (17, 21, 22). Recently, Mekkawy and colleagues indicated that complex TGA can be operated with low m (20). Similar to the latter study, current study showed no difference in the rate of complications and mortality among patients with simple or complex TGA (P value = 0.999).
Coronary circulation is varied anatomically in these patients. Being a major concern, coronary transfer is important particularly when coronary anomalies exist (5, 16). Anatomical variations are not related to the increased mortality, based on the findings of some studies (18, 23). Three-fold mortality is associated with abnormal coronary looping with a single ostium (24). In our study, advanced medical care and rich experience of the surgeon contributed to managing the complex TGAs with complex coronary branching patterns. The prevalence of the late coronary mortality is less than 2%, which is rare (17, 25, 26). A meta-analysis on 1942 patients indicated doubled risk of mortality for any variant of coronary artery anatomy (24); furthermore, a cohort of 618 patients between 1983 and 2009 declared that coronary artery patterns are not a risk factor for mortality (12). Same result was found by Blume and colleagues (27). In accord with previous studies, this study indicated no association between unusual coronary pattern and mortality rate (P value = 0.999). They demonstrated that inverted coronary pattern and single right coronary patterns are related to delayed sternal closure and prolonged mechanical ventilation (27). The sensitivity and specificity of echocardiography for diagnosis of the coronary pattern abnormality in this study was 42.9% and 88.1%. This means echocardiography is not much reliable for predicting the abnormal coronary patterns in patients with ASO.
Pulmonary stenosis and aortic regurgitation are among the most common anatomical complications following the surgery. AR plays an important role in occurring the late complications, which may eventually lead to aortic valve replacement (28, 29), a potential adverse outcome for pediatric patients. Considering as a rare adverse complication, the prevalence of AR, based on the studies with long follow-up, ranges from 0.3% to 10% (17, 30, 31). The prevalence of immediate post-operative AR in this study was 41.6%, mostly (40%) trivial and mild AR. Trivial or mild AR is likely to disappear during the follow-up postoperatively (32); thus the true prevalence of AR in this study is estimated to be 1.6%, which is in line with the aforementioned studies. PS prevalence is reported to be 5.1% to 56% (33-35). It has usually occurred as a result of anastomotic scar formation, tension on anastomotic site caused by insufficient aortic root mobilization and applied potalon pericardial patch on the anastomotic site (34, 35). The prevalence of PS in the current study was 4%, all of them were mild. This reflects the optimal surgical technique which did not result in anastomotic scar formation or other causes of PS resulted from inappropriate surgical technique.
Arrhythmias in these patients are mostly caused by atrial reconstruction. Cardiac rhythm disturbances are found in 3% - 7% of the patients post-operatively (36, 37). The total rate of arrhythmia in this study was 12.8%, the rhythm abnormality related to the atrial reconstruction (atrial flutter, long QT syndrome, paroxysmal supraventricular tachycardia, suck sinus syndrome and Wenckebach) was 4.8% and ventricular arrhythmia (right bundle branch block and ventricular tachycardia) was present in 8% of the subjects. Several studies have shown that prolonged cardiopulmonary bypass time is associated with postoperative adverse outcomes (20, 27, 38). Mekkawy and colleagues found that CPB time is associated with postoperative bleeding and length of mechanical ventilation, but found no association between CPB time and lactate level (20). Prolonged CPB time, major perioperative events and abnormal coronary pattern are among the important risk factors of early mortality (39). In this study patients with complex DTGA had a higher CPB time, compared to the simple ones (P value < 0.0001) and lesions associated with VSD had a higher CBP time compared to the lesions without VSD (P value = 0.004). The 30-day mortality rate in North America and Europe is less than 3% (5); however, the mortality rate has been higher in the early experience in the developed areas (40). The early mortality in the study of Pretre and colleagues was reported 6% (31), ln that of Prandstetter and colleagues it was 1.75% (41), in Frick and colleagues 2.8% (12). The early mortality rate in the present study was 4%, which is within the range of mortality rate in previous studies.