1. Background
Post-Traumatic Stress Disorder (PTSD) is a psychiatric condition, which is due to experiencing or witnessing life-threatening events such as military combat, natural disasters, terrorist incidents, serious accidents, or physical or sexual assault (1). The condition influences family relations and well-being and can have a long-term impact on ones mental health (2, 3). In the DSM-IV-TR, direct exposure or witness or confrontation with a traumatic event was introduced as a diagnostic criteria for PTSD (1). However, according to clinical observations and experimental studies, traumatic events not only affect the victims, but also their families and others in their environment (4, 5). The term ‘secondary traumatization’ has been used to describe this secondary, indirect effect of traumatic experiences (6). Secondary traumatization affects the mental health of wives and families of war veterans with PTSD (7). Wives of war veterans with PTSD also report somatic complaints, tension, confusion, and low self-esteem (4). Despite this considerable influence of secondary traumatization, indirect secondary exposure to traumatic event(s) was not considered as diagnostic criteria for PTSD in the DSM-IV-TR. To our knowledge, PTSD symptoms did not directly manifest among family members of Iranian veterans who had trauma from the Iran - Iraq war. For the first time, DSM-V introduced indirect exposure to traumatic events as a diagnostic criteria for PTSD: “learning that the traumatic event (s) occurred to a close family member or close friend” (8).
One of the most prevalent disorders reported by persons with PTSD, and specifically veterans with chronic war-induced PTSD, is sleep difficulties (9, 10). According to studies, 44% of veterans with PTSD report difficulty falling asleep, and 91% had difficulty maintaining sleep (11). Sleep disturbance may help differentiate chronic PTSD from healthy subjects (12). Sleep problems have been studied and well documented by subjective assessments (9), however, some studies report significant differences between objective and subjective sleep assessments among the PTSD population (13). On the other hand, unlike subjective investigations, some studies using objective methods such as polysomnography and actigraphy were unable to find any differences in sleep architecture between patients with and without PTSD (14). Therefore, paradoxical insomnia has been proposed to better understand the research question (13).
While most sleep studies have focused on the individual, the impact of sharing a bed and probably sharing thoughts on one’s partner’s sleep quality has been neglected. Data concerning couples’ sleep interactions are rare, however, some studies have shown that not only do individuals’ sleep problems negatively affect their own health, however, it also affects the health and well-being of their partner (15-17). On the other hand, partners’ sleep quality has been found to improve when their spouses, who suffered from sleep apnea, began receiving Continuous Positive Airway Treatment (CPAP) (18). In spite of this evidence, to our knowledge, the effects of sleep problems on partners’ sleep quality have not been studied.
Therefore, PTSD in veterans may induce PTSD symptoms in their wives and influence their sleep quality, both directly, and indirectly. Due to secondary traumatization, PTSD may have critical effects on wives’ mental health and many aspects of their lives, including sleep. Despite these important concerns, to our knowledge neither PTSD symptoms nor sleep quality among wives of veterans with PTSD have been studied. Therefore, this preliminary study aims to investigate PTSD symptoms and sleep patterns of war - induced PTSD veterans and their wives in a small - group setting.
2. Objectives
In the present study, we aimed to investigate PTSD symptoms and sleep quality among chronic PTSD patients and their wives using subjective self - reporting questioners and objective sleep measures by actigraphy.
3. Materials and Methods
This was a cross - sectional study to investigate PTSD symptoms and sleep quality in veterans with chronic war PTSD and their wives. This study was approved by the Research Council and Ethics Board of Kermanshah University of Medical Sciences (KUMS) with ethical code number 48649. All participants provided written informed consent.
3.1. Participants
Fourteen veterans of the Iran-Iraq war (1980 to 1988), with ages ranging between 38 and 65 years (Mean ± SD = 50 ± 7), who had been diagnosed with chronic PTSD, and their wives, with ages ranging between 35 and 61 years (Mean ± SD = 44 ± 7; P = 0.05), were recruited for participation in this study. All consecutive veterans with chronic PTSD who also report insomnia complaints and were referred to Sleep Disorders Research Center (SDRC) of KUMS between March 2013 to November 2014 were also recruited for this study, according to the inclusion and exclusion criteria. Diagnosis of PTSD related to combat exposure emergent from psychiatric interview according to DSM-IV-TR was considered as the main inclusion criteria. Exclusion criteria included schizophrenia, bipolar or other psychotic disorders, and active suicidal ideation. Depression was not considered as an exclusion criteria since combat veterans with PTSD usually have this condition. In addition, participants with sleep apnea or periodic limb movement during their sleep were excluded. All women were in their ovarian cycle and did not have any menstrual disorders. All veterans reported trauma related to combat experience, bombardment, or mine explosion.
3.2. Measures and Procedures
All veterans were interviewed by a psychiatrist using the Structured Clinical Interview for DSM-IV-TR Disorders (SCID). PTSD was defined by criteria described within the DSM-IV-TR (1). Finally, both veterans and their wives completed the military PTSD checklist for DSM-IV (PCL-4) (19). The military version of PCL was used since we aimed to investigate those veterans who had had stressful military experiences and consider if these experiences had any effects on their wives.
After providing informed consent, participants completed the PSQI individually. The instrument’s most important domains included sleep quality, latency, duration, efficiency, and disturbances. The Iranian version of the PSQI was validated among PTSD patients with a diagnostic sensitivity of 100% and a specificity of 93%. Overall, the Cronbach’s alpha coefficient was 0.89 (20). In the subsequent step, all participants underwent an overnight ambulatory actigraphy sleep EEG monitoring for objective evaluations (Somnomedics, Germany). All couples shared the same bed on the recording night. Parameters such as total sleep time, sleep onset latency, and sleep efficiency were documented.
3.3. Statistical Analysis
The data was downloaded to a computer and averages for variables obtained over one night were used for analysis. The PCL-M score was compared between two groups using independent sample t - test. Both objective and subjective sleep indices were subjected to intra - and inter - comparisons. Objective and subjective results were compared separately for each group by paired sampled t - tests. Between groups, comparison was done by independent sample t - test and Mann-Whitney U test for data distributed normal and non-normal respectively. After that, correlations between subjective and objective sleep qualities were evaluated by Pearson’s or Spearman’s correlation coefficients. All the analyses were conducted using SPSS software version 16. Normal distribution of data was evaluated using one-sample Kolmogorov - Smirnov test.
3.4. Ethics
This work was financially supported by KUMS (grant No: 92091). The authors would like to acknowledge everyone who participated in this study.
4. Results
For evaluating the effect of veterans’ PTSD on their wives, the total score of PCL-M in both groups was compared by independent sample t - test. Results indicate no significant differences in total PCL-M scores between these two groups. Item indicated that the arousal symptom was higher significantly among veterans in comparison to their wives. Items related to re-experiencing and avoidance was slightly higher among veterans, however, it did not indicate significant differences (Table 1). According to cut point of 50 for total PCL scores, 7 wives had PTSD and 4 wives of veterans with PTSD did not show the PCL index for PTSD. In addition, we observed a positive correlation between PCL total score in the two groups (r = 0.56; P = 0.03). According to the PSQI (P < 0.01), though not the actigraphy, veterans with PTSD reported significantly worse sleep quality than their wives (Table 1). A significant positive correlation was observed between PTSD severity and PSQI total scores (r = 0.53; P < 0.01).
| Veterans | Wives | P Value | |
|---|---|---|---|
| PCL | |||
| Pcl. b/Re-experiencing | 16.85 ± 4.96 | 14.07 ± 6.12 | 0.21 |
| Pcl. c/Avoidance | 21.62 ± 6.15 | 18.57 ± 7.95 | 0.28 |
| Pcl. d/Arousality | 18.38 ± 4.35 | 13 ± 5.44 | < 0.01 |
| Total | 58.2 ± 13.21 | 46.36 ± 17.16 | 0.051 |
| PSQI | |||
| Total sleep time | 4.85 ± 2.53 | 6.70 ± 2.06 | 0.04 |
| Sleep latency | 88.21 ± 60.05 | 41.79 ± 29.65 | 0.01 |
| Sleep efficiency | 55.43 ± 19.56 | 88.89 ± 18.59 | < 0.01 |
| Total PSQI scores | 16.29 | 9.71 | < 0.01 |
| Actigraphy | |||
| Total sleep time | 7.11 ± 1.01 | 7.69 ± 1.45 | 0.23 |
| Sleep latency | 17.85 ± 19.75 | 10.57 ± 28.68 | 0.43 |
| Sleep efficiency | 81.51 ± 11.11 | 88.01 ± 16.62 | 0.23 |
Veterans indicated significantly poorer PSQI subjective sleep quality than actigraphy sleep quality indices (P < 0.01). However, wives’ PSQI and actigraphy total sleep time and sleep efficiency did not show significant differences. Similarly, as compared to the veterans, the wives’ PSQI sleep latency was significantly higher than the actigraphy sleep latency (P < 0.01) (Table 2).
| PSQI | Actigraphy | P Value | |
|---|---|---|---|
| Veterans | |||
| Total sleep time | 4.50 ± 2.31 | 7.11 ± 1.01 | < 0.01 |
| Sleep latency | 73.93 ± 49.38 | 17.85 ± 19.75 | < 0.01 |
| Sleep efficiency | 51.55 ± 18.28 | 81.51 ± 11.11 | < 0.01 |
| Wives | |||
| Total sleep time | 6.70 ± 2.06 | 7.69 ± 1.45 | 0.23 |
| Sleep latency | 41.79 ± 29.65 | 10.57 ± 27.68 | < 0.01 |
| Sleep efficiency | 88.89 ± 18.59 | 88.01 ± 16.62 | 0.91 |
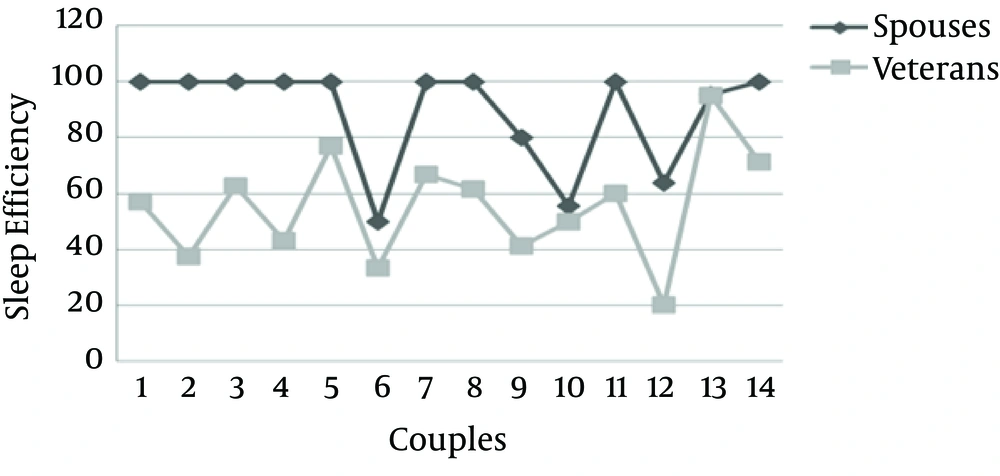
To investigate the effects of veterans’ sleep problems on their partners’ sleep quality, the correlation between their sleep quality indices was calculated using Pearson and Spearman correlation coefficients for normal and non-normal distributed data, respectively. There was no significant correlation between the objective sleep indices of the two groups (P > 0.05). Except for PSQI sleep efficiency, there is no significant correlation between subjective sleep indices. The Pearson correlation coefficient for PSQI sleep efficiencies between the two groups was significantly positive (r = 0.56; P = 0.03; Figure 1).
5. Discussion
In this preliminary study, we aimed to investigate PTSD symptoms and sleep patterns of war PTSD veterans and their wives in a small - group setting. According to PCL, wives reported considerable symptoms of PTSD like their husbands. Our investigation of PTSD revealed that the majority of spouses have some degree of PTSD and the severity of symptoms correlate positively with severity of symptoms in their husbands. This finding strongly indicated the presence of secondary traumatization and confirmed previous findings (4, 6, 21, 22). Induced PTSD is characterized by transfer of trauma from one person who has had direct exposure to traumatic experiences to a closely related one who did not have direct exposure. Veterans with war related PTSD (primary case) are often chronically ill and are typically influential members of close relationships with more suggestible wives (secondary case) who also develop symptoms of PTSD. The secondary case (wives of veterans with chronic PTSD) may be frequently more passive or more lacking in self-esteem and more suggestible. This occurrence of symptoms of PTSD is attributed to strong veterans with chronic war-induced PTSD (23). It is interesting that the veterans reported significant higher arousal symptoms in comparison to their wives, however, the other two PCL items, including re-experience and avoidance, were not higher significantly: the wives reported scores just as high as veterans in these two clusters. These results may be due to the more biological base of arousality that comes from direct exposure to traumatic events, which were not experienced by the wives. On the other hand, re-experience and avoidance are cognitive aspects of PTSD and can be induced and shared between couples (24).
According to the subjective data, veterans reported a significantly lower total sleep time and sleep efficiency as well as a higher sleep latency than their wives. These sharp differences between sleep qualities indices were not observed in the objective data obtained from actigraphy. Veterans had slightly lower, but non-significant, total sleep time and sleep efficiency, and higher, but non-significant, sleep latency in comparison to their spouses. A significant positive correlation between PTSD severity and PSQI total scores indicated that higher PTSD severity leads to lower sleep quality. This finding confirmed previous results about poorer sleep quality among people with PTSD (25).
Comparisons of subjective and objective sleep quality suggested paradoxical insomnia among veterans and wives. For veterans, subjective total sleep time and sleep efficiency were lower, and sleep latency was higher than that observed in the objective actigraphy data. Therefore, present findings corroborate the paradoxical insomnia reported by some previous studies (13, 14). As for the spouses, merely the difference between PSQI and actigraphy sleep latency was significant. They reported more sleep latency than that obtained by the objective actigraphy result. Sleep latency in itself is not completely objective, due to the fact that when we use ambulatory monitoring by actigraphy, both self - report of turn off the light with objective record of sleep were used. This may be the reason of disagreement between the questionnaire and actigraphic measure of sleep latency among wives. On the other hand, this finding may reveal the presence of the same, but weaker, paradoxical situation for spouses, and most probably demonstrates the effects of the veterans’ sleep situations on the sleep quality of their wives, which was hypothesized, however, not directly studied by previous investigators (7, 26, 27). Therefore, we could propose that the wives’ shared paradoxical insomnia is induced by their husbands’ sleep problems. In addition, the secondary traumatisation experienced by wives of veterans with chronic war PTSD may influence this paradoxical situation for sleep latency.
Considerable positive correlations between the two groups’ subjective sleep efficiency may reveal a bidirectional association between the sleep quality of veterans with PTSD and that of their wives. Although more studies with larger sample sizes would be needed to assess this association, it is possible that the association may be induced by the direct effect of veterans’ sleep quality on spouses’ sleep. Additionally, veterans’ judgments about their sleep may induce similar judgments from their spouses. The close relationships between couples who have lived together for a long time may provide environments conducive to the sharing of thoughts and beliefs about all aspects of life, including sleep quality. Furthermore, secondary traumatization may play an important role in the significant correlation witnessed between the two groups in terms of sleep quality. In addition, previous studies have demonstrated the harmful effects of chronic PTSD on couples’ relationships, particularly marital satisfaction and the mental health status of wives and other family members (4, 6, 7). We propose the necessity for a better - controlled study with a larger sample size to investigate both objective and subjective measures among families suffering from PTSD.
5.1. Conclusion
The wives of persons with PTSD indicated some degree of PTSD. Veterans with PTSD reported poorer sleep quality than their wives. PTSD could negatively influence sleep quality. Sleep efficiency was correlated positively among veterans and wives. Paradoxical insomnia was suggested among both veterans and their wives.
5.2. Strengths and Limitations
Since this is the first study to investigate induced PTSD in wives of veterans with chronic PTSD from the Iran - Iraq war, the present findings should be considered in light of both the strengths and limitations of the study. We revealed induced and indirect PTSD symptoms in wives; however, other family members may also show PTSD symptoms. Future studies are recommended to investigate induced PTSD among other family members of veterans with war - induced PTSD (e.g. their children).
Concurrently, investigation of both objective and subjective sleep quality is the strength of this study. In fact, the outcome of combining the two methods provided us with the opportunity to make a more accurate judgment concerning subjects’ sleep difficulties. Some limitations should be taken into account when interpreting our results. One major limitation of the present study is small sample size, which was due to limited access to potential subjects. In addition, lack of control group for veterans and wives is another limitation. The objective sleep duration in this study was based on actigraphy through the course of one night, which may not be representative of habitual sleep duration and may be affected by first-night effects. For controlling first night effects, it is more reliable to include longer recordings of actigraphy. Detailed evaluation of marital satisfaction and its relationship with PTSD severity as well as couples’ sleep quality in future studies could provide mechanism of sleep quality interactions in veterans and their wives. We recommend further research be undertaken with a view to overcome these limitations.