1. Background
The incidence of heart diseases is rising in many societies (1, 2). Among these diseases, coronary heart disease (CHD) has caused the death of 7.3 million patients around the world and led to mortality more than any other disease (1). Quality of life (QOL) includes psychological, social, and physical well-being in people with medical diseases and disabilities (3, 4). Moreover, health-related quality of life is a reflection of the effects of the disease and their treatments with regards to the patient’s views and experiences (5). Coronary Heart Disease has many adverse effects on health-related QOL (4, 6).
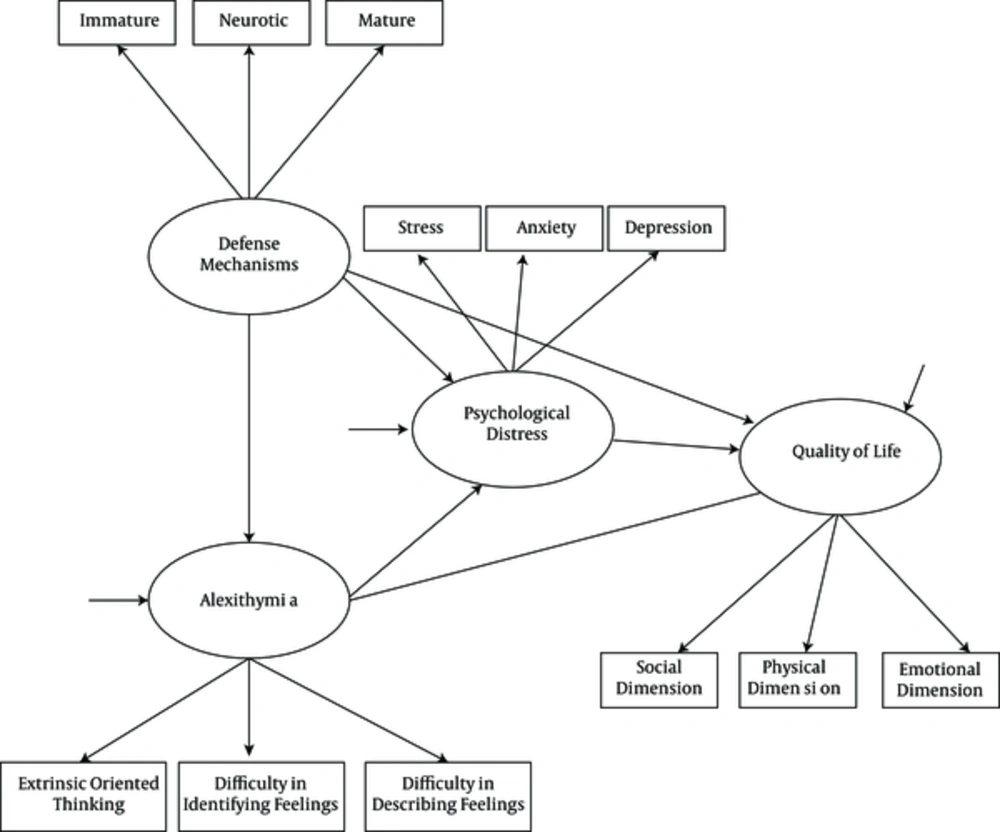
In order to promote the quality of life of patients with CHD, it is necessary to examine factors affecting this disease (2). In the recent years, strong and cohesive studies have provided data on the high importance of psychological factors in the etiology and exacerbation of cardiovascular diseases (7). Psychological distress, including depression, anxiety, and stress, are of the most important factors in morbidity and mortality among patients with CHD (7, 8). Depression as the most common psychological state has a strong effect on increased incidence, inappropriate prognosis, and increased mortality in patients with CHD (9, 10). Similarly, higher levels of anxiety and stress in patients with CHD decrease the QOL and increase mortality (11, 12). Patients with heart disease are at greater risk of anxiety and psychological stress due to a lack of adaptive defense mechanisms and maladaptive coping with stress (13). Defense mechanisms and alexithymia are important personality traits related to QOL and psychological distress in the patients (14, 15). Defense mechanisms are unconscious psychological processes that protect the patients against anxiety and internal or external threats by reducing the effect of unpleasant emotions and maximizing the effect of pleasant ones (16). Defense mechanisms are important factors associated with mental and physical health and quality of life of patients (17, 18). According to Newton (13), patients with heart disease are more exposed to adverse outcomes because of maladaptive defense mechanisms that facilitate unfavorable effects of distress. Despite the importance of defense mechanisms in physical health, as a shortcoming in previous literature, no study was found regarding the mediating role of psychological distress. Along with defense mechanisms, alexithymia can also affect physical performance (19). Alexithymia refers to disability in identifying, processing, or describing feelings, and difficulty in differentiating feelings with physical and emotional arousal (15). Alexithymia is generally associated with health problems such as heart diseases (20, 21). Moreover, alexithymia can disrupt QOL in patients with physical diseases (22). Since alexithymia reflects a deficit in the processing of emotions, it can trigger psychological distress among patients and indirectly reduce their QOL (15). Higher alexithymia is a very important factor in predicting deteriorated QOL (8). In previous studies, no study was found on the role of alexithymia in the QOL in patients with CHD regarding the mediating role of psychological distress. As another shortcoming, defense mechanisms and alexithymia were examined separately in previous studies (17, 19). In addition, indirect roles of defense mechanisms and alexithymia in QOL by other psychological underpinnings are not well known. Therefore, more studies are needed for better understanding of latent and indirect role of defense mechanisms and alexithymia on QOL. In order to eliminate this research gaps, and to provide new knowledge in this field, improve quality of life, and reduce psychological distress in these patients, conducting the study was necessary. According to the problem statement and based on previous models (7, 8, 23, 24), the hypothetical model of the present study was as follows (Figure 1).
2. Objectives
This study aimed at examining the role of defense mechanisms and alexithymia in predicting the quality of life of patients with coronary heart disease considering the mediating role of psychological distress based on the above-mentioned hypothetical model and evaluation of model fitness indices.
3. Materials and Methods
3.1. Study Subjects
This research was a cross-sectional descriptive study. The statistical population of the study was patients with coronary heart disease, who had referred to the specialized heart center of Ayatollah Madani governmental hospital in Khorramabad city of the Lorestan State from February to July 2015. This study was reviewed and approved by the Research ethics committee of the department of psychology and educational sciences of Semnan University (RET: 98.92.626). According to the minimum appropriate sample size in structural equation model based on model parameters (25) and to increase statistical power and manage the possible decrease in the number of participants, a sample size of 300 participants was selected by convenience sampling method from Khorramabad city. Sample selection criteria included informed consent and willingness to participate in the study, the willingness to cooperate in completing the instruments, physical and mental stability (lack of physical or psychological distress, such as breath shortness, that intervenes with answering the items), and age range of 20 to 60 years. Acute psychosocial crisis, unwillingness to complete the self-report measures, medical comorbidity, and dual diagnosis were exclusion criteria in this study. Furthermore, the patients were excluded if they were receiving continuous treatment due to serious physical or mental disease, had cognitive impairments or deficits in cognitive functioning according to the medical records and previous neurological examinations, or had acute or severe symptoms of the disease, which made participation in the study difficult.
3.2. Measures
Instruments used in this study included the demographic checklist, the Mac-New health-related quality of life questionnaire for patients with heart diseases (Mac-New HR-QL), the depression, anxiety and stress scales (DASS-21), the defensive styles questionnaire (DSQ-40), and the toronto alexithymia scale (TAS-20).
The demographic checklist included age, gender, educational level, marital status, occupation, monthly income, history of having physical and psychological diseases, history of hospitalization, history of heart disease in the family, and family support.
The Mac-New health-related quality of life questionnaire for patients with heart disease (Mac-New HR-QOL) is a self-report instrument that has 27 items and assesses quality of life in physical and psycho-social dimensions. Each item is on a 7-point Likert scale (from always to never) and the average response time is 10 minutes (26). The reliability of Mac-New questionnaire in the Iranian population using Cronbach’s alpha was 0.92, 0.92, 0.95, and 0.95 for emotional, physical and social dimensions, and for the total scale, respectively (27). The correlation coefficients were 0.42, 0.38, 0.31, and 0.50 for emotional, physical and social dimensions, and for the total scale, respectively (27). The intergroup correlation coefficients were 0.92, 0.92, 0.93 and 0.95 for emotional, physical and social dimensions, and for the total scale, respectively. The reliability of this questionnaire through construct reliability was in the range of 0.63 to 0.74 for emotional, physical, and social dimensions (27).
The depression, anxiety and stress scales (DASS-21) were prepared by Levibond S. H. and Levibond P. F. in 1995 (28). The scale included 21 items; each item was on a 4-point Likert scale from not at all (0) to high (3). Each of the depression, anxiety, and stress variables were evaluated by seven different phrases in this questionnaire and finally the total score of depression, anxiety, and stress were calculated separately for each patient (29). The coefficient obtained for the three scales of depression, anxiety, and stress were 0.91, 0.84 and 0.90, respectively, and these values were acceptable (28). The short form of this questionnaire was validated for the Iranian population in 2005 by Sahebi et al. (30). Internal correlations of the scale were 0.77, 0.79, and 0.78 for depression, anxiety, and stress using Cronbach’s alpha, respectively.
The defensive styles questionnaire has 40 items on 20 defense mechanisms in 3 levels of mature (items of 2, 3, 5, 7, 21, 24, 29 and 35), neurotic (items of 1, 6, 11, 17, 28, 33, 34, and 40), and immature (other items) on a 9-point Likert scale, from totally agree (9 scores) to totally disagree (1 score). Andrews, Singh, and Bond (31) reported a re-test correlation coefficient of 0.46 to 0.86 for this questionnaire. In a study by Heydarinasab et al. (32), Cronbach’s alpha was reported between 0.69 and 0.81 for defensive styles questionnaire. Among defensive styles in a previous study, the highest alpha was related to undeveloped defensive styles and was calculated as 0.72, and the least alpha was related to neurotic defensive styles and was calculated as 0.50 (33).
The Toronto Alexithymia Scale has 20 items, which evaluates alexithymia in 3 subscales of difficulty in identifying feelings, difficulty in describing feelings, and extrinsic oriented thinking (34). Each item is on a 5-point Likert scale from totally disagree (score 1) to totally agree (score 5). In a sample of 401 undergraduate students, Cronbach’s alpha for the total scale was 0.80, 0.79, 0.75, and 0.66 for its three components. Ghorbani et al. (35) obtained an alpha of 0.74 for difficulty in identifying feelings, 0.61 for difficulty in describing feelings, and 0.50 for extrinsic oriented thinking of this scale in the Iranian sample. In grading the Toronto alexithymia scale, scores higher than 60 were considered as alexithymia and scores below 52 as a non-alexithymia (36).
3.3. Administration
At the beginning, the study was approved by the higher education committee of the psychology department at Semnan University with the following code of 98.92.626, and a referral letter was received. Firstly, written informed consent was obtained from all participants. Then, researchers referred to the specialized heart center of Ayatollah Madani governmental hospital of Khorramabad city of Lorestan and with permission obtained from the staff of the hospital and coordination with heart specialists, patients’ medical records were examined. After making sure of a diagnosis of coronary heart disease by physicians and considering the inclusion and exclusion criteria, data were collected from the patients, some of whom were outpatients and rest hospitalized patients. The counterbalancing method was used, in which the items of the questionnaires and scales are changed, so that the main 4 questionnaires of this study were displaced. To establish moral considerations, the patients were firstly informed of about the aims of the study and the effects of such studies in identifying and improving their conditions. All participants were assured that the researcher could keep their data confidential. In this study, the authors considered all ethical issues, such as informed consent.
3.4. Statistical Analysis
For data analysis, the SPSS-19 Software was used in order to calculate the indices of descriptive statistics such as mean, standard deviation, frequency, and frequency percentage. To analyze the inferential findings, the structural equation model was used by the AMOS software. P values of < 0.05 were considered as significant difference in this study.
4. Results
The mean and standard deviation of the respondents’ age was 46.71 ± 9.78 in the present study. Socio-demographic characteristics and medical history of the statistical population are presented in Table 1.
| Characteristics | No. (%) |
|---|---|
| Gender | |
| Female | 165 (55) |
| Male | 135 (45) |
| Literacy | |
| Diploma below | 190 (63.3) |
| Diploma | 59 (16.7) |
| Over diploma | 15 (5.0) |
| License | 35 (11.7) |
| MSc degree and higher level | 10 (3.3) |
| Marital status | |
| Married | 242 (80.7) |
| Single | 24 (8.0) |
| Widowed | 32 (10.7) |
| Divorced | 2 (0.6) |
| Occupational status | |
| Employed | 36 (12.0) |
| Housewife | 139 (46.3) |
| Free work | 66 (22.0) |
| Unemployed | 17 (5.7) |
| Retired | 42 (14.0) |
| Monthly income, Rials | |
| Income between 7 to 15 Million | 140 (46.7) |
| Income between 15 to 25 Million | 152 (50.6) |
| Income of higher than 25 Million | 8 (2.7) |
| History of serious medical conditions | |
| Not exist | 164 (54.7) |
| Exist | 136 (45.3) |
| History of psychiatric disorder | |
| Not exist | 280 (93.3) |
| Exist | 20 (6.7) |
| History of heart diseases in family | |
| Not exist | 165 (55) |
| Exist | 135 (45) |
| History of hospitalization | |
| Not exist | 141 (47) |
| Exist | 159 (53) |
Table 2 represents descriptive findings including mean, standard deviation and significant and non-significant correlation coefficients.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | 50.67 | 54.88 | 137.12 | 24.50 | 16.33 | 22.35 | 57.13 | 48.88 | 57.37 | 106.16 | 7.55 | 8.38 | 8.96 |
| Standard deviation | 8.81 | 8.71 | 25.73 | 5.22 | 3.66 | 3.02 | 12.99 | 12.78 | 14.12 | 24.04 | 3.80 | 3.91 | 4.10 |
| 1.Mature defense mechanisms | |||||||||||||
| 2. Neurotic defense Mechanisms | 0.37b | ||||||||||||
| 3.Immature defense mechanisms | -0.27b | 0.37b | |||||||||||
| 4.Difficulty in identifying feelings | 0.03 | 0.23b | 0.48b | ||||||||||
| 5.Difficulty in describing feelings | 0.02 | 0.16b | 0.43b | 0.53b | |||||||||
| 6. Extrinsic oriented thinking | 0.02 | 0.11 | 0.25b | 0.24b | 0.42b | ||||||||
| 7.Emotional dimension of QOL | 0.07 | -0.13a | -0.39b | -0.49b | -0.34b | -0.09 | |||||||
| 8.Physical dimension of QOL | 0.04 | -0.17b | -0.36b | -0.44b | -0.37b | -0.12a | 0.78b | ||||||
| 9. Social dimension of QOL | 0.10 | -0.15b | -0.30b | -0.38b | -0.33b | -0.11a | 0.77b | 0.91b | |||||
| 10. Total score of QOL | 0.07 | -0.16b | -0.38b | -0.48b | -0.37b | -0.12a | 0.93b | 0.45b | 0.91b | ||||
| 11. Depression | -0.11a | 0.08 | 0.25b | 0.43b | 0.34b | 0.11a | -0.61b | -0.56b | -0.54b | -0.62b | |||
| 12. Anxiety | 0.09 | 0.15a | 0.26b | 0.39b | 0.30b | 0.04 | -0.64b | -0.63b | -0.57b | -0.67b | 0.70b | ||
| 13. Stress | -0.22b | 0.02 | 0.24b | 0.38b | 0.26b | 0.02 | -0.61b | 0.54b | -0.52b | -0.16b | 0.73b | 0.76b |
aP < 0.05.
bP < 0.01.
Before using the structural equation model, univariate outliers were examined by the rectangular plot (box plot) and outlier data were replaced with the closest last data. In addition, the rectangular plot showed that diagrams of the variable’s distribution were similar. Results of the Kolmogorov-Smirnov test, to examine the hypothesis of normality at the level of P ≤ 0.001, were as follows: Mature, neurotic, and immature defense mechanisms, respectively (P = 0.015, 1.57; P = 0.001, 2.08; P = 0.022, 1.50), difficulty in identifying and describing feelings respectively (P = 0.011, 1.61; P = 0.001, 2.21), extrinsic orientation thinking (P = 0.001, 1.92), emotional, physical and social dimensions of QOL, respectively (P = 0.723, 0.69; P = 0.559, 0.79; P = 0.033, 1.43), and depression, anxiety and stress, respectively (P = 0.013, 1.59; P = 0.043, 1.39; P = 0.006, 1.71). The regression standardized residuals showed that points were distributed randomly that indicated the equality of variances. To examine the independence of the errors, Watson camera statistic showed that the hypotheses of independence was established and the observed values were between 1.5 and 2.5. On the multicollinearity, the results showed that the minimum of tolerance equaled 0.47 and the maximum of Variance Inflation Factor (VIF) equaled 1.75, which showed that there was no multicollinearity between independent variables. Considering the foundation of the hypothesis, path analysis was used.
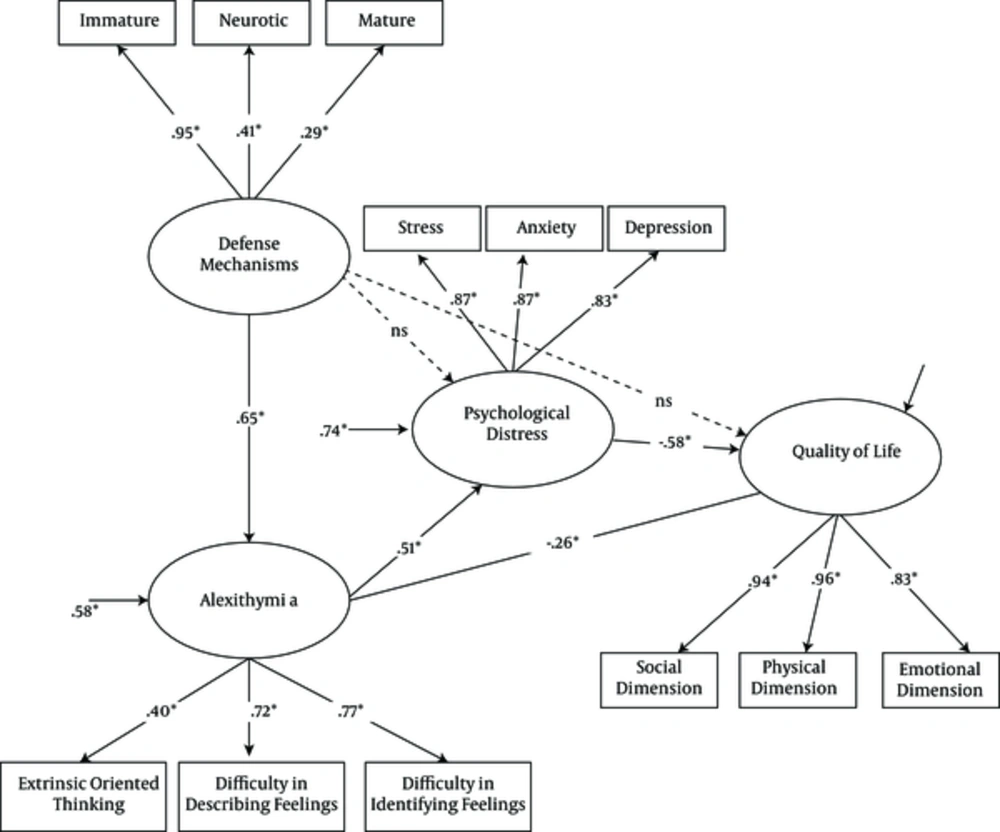
Figure 2 Estimates the tested model of the relationship between defense mechanisms, alexithymia, and psychological distress with quality of life in patients with CHD, based on the path analysis. The mentioned numbers showed the unexplained variance values.
In the structural equation model (Figure 2), measurement models by a factor analysis showed that all components of measures had statistical significant factor loads (P < 0.05). According to the structural model of path analysis, the path coefficient of the defense mechanisms to the alexithymia, the alexithymia to the QOL, the alexithymia to the psychological distress and the psychological distress to the QOL were significant (P < 0.05). On the other hand, the path coefficients of the defense mechanisms to the psychological distress and the defense mechanisms to the QOL were not significant (P >0.05).
Fit indices for the model are presented in Table 3. The results of the Chi-square test (χ2) indicate the poor fit of the model with data. Because the chi-square index is highly influenced by sample size, the experts suggest the use of other fit indices (37). The NFI and CFI values in this study were equal to 0.94 and 0.95, respectively, which were confirmed based on the obtained values of the model. Root mean square error of approximation (RMSEA) showed the mean of the residuals between correlations, observed covariance in the sample, and expected model estimated for the population. Fan et al. (37) considered values less than 0.08 as a good fit, 0.08 to 0.10 as average fit, and higher than 0.10 as poor fit. The value of RMSEA of this study was 0.050, which indicates a good fit for the model of the data.
| Model Fit Indices | Good Fitness Criterion | |
|---|---|---|
| χ2 | 205.87a | |
| df | 48 | |
| p | P < 0.01 | > 0.05 |
| CFI | 0.95 | > 0.90 |
| NFI | 0.94 | > 0.90 |
| RMSEA | 0.050 | < 0.07 |
aP < 0.01.
5. Discussion
The path analysis showed that defense mechanisms are not directly involved in predicting the quality of life in patients with coronary heart disease. This finding is consistent with previous studies in different groups (13, 14, 16). According to similar studies, defense mechanisms indirectly effect QOL in the patients towards certain psychological mediators. It has been discussed that defense mechanisms indirectly effect QOL in patients with CHD, through factors such as social support and other personality traits (14, 16). In fact, mature defense mechanisms are important for making good social relationships and better quality of life (38). Moreover, immature defense mechanisms reduce health-related QOL in patients with CHD, indirectly through increasing psychological distress, including depression, anxiety, and stress (13, 16). According to the path analysis, defense mechanisms are not involved in predicting QOL in patients with CHD, indirectly through psychological distress. In the absence of similar studies, this finding is inconsistent with previous studies on other groups (13, 14, 17). In explaining this finding, it can be stated that patients with heart disease are more exposed to stressful events because of the use of maladaptive coping styles and immature defense mechanisms that facilitate traumatic effects of anxiety (13). In addition, it can be argued that using maladaptive defense mechanisms against life problems is directly related to psychological distress, as an unfavorable underpinning for deteriorated QOL (14). As a result, the continuous use of immature and neurotic defense mechanisms increase emotional problems and have negative effects on QOL (17, 38). The difference in research methods, and social, and cultural formulation of factors are associated with CHD in the studied populations and are of major reasons for the inconsistency of the findings of the present study with previous studies. Furthermore, the findings showed that defense mechanisms are indirectly involved in predicting the QOL in patients with CHD through alexithymia. To explain this new and important finding, alexithymia, as lack of emotional experiences, is considered as a maladaptive coping mechanism that is total denial of emotions and feelings to protect the self against emotional distress and extremely traumatic events (39). Therefore, people with neurotic and immature defense mechanisms generally encounter stressful situations through denial, revocation or neglect, such as patients with alexithymia that deny distress (40). Moreover, alexithymia can be considered as the inability in managing debilitating emotions as the main function of defense mechanisms (41). In addition, defense mechanisms act to manage debilitating emotions and it can be stated that creation, escalation or adjusting alexithymia are other ways of indirectly effecting defense mechanisms and QOL in patients with CHD. In fact, defense mechanisms reduce QOL in patients through decreasing emotional regulation. In addition, the results showed that alexithymia is indirectly involved in predicting QOL in patients with CHD with the mediating role of psychological distress. These findings are consistent with previous studies (7, 15, 20, 41). To explain these findings, it has been argued that alexithymia increases misconceptions of the patients about their disease and results in deteriorated of QOL (41). Furthermore, patients with alexithymia, because of deficits in the cognitive processing of emotions, have exaggerated distress and worsened QOL. Consistent with previous findings (39, 42), in this study alexithymia is indirectly involved in predicting QOL in patients with CHD via psychological distress. In explaining these findings, it should be noted that patients with alexithymia cannot understand their feelings and emotions and thus did not express them. In addition, it has been discussed that alexithymia negatively effects health-related QOL in patients with heart disease through somatization of psychological distress or enhancing the patients’ physical symptoms (43, 44).
Limitations of the study were the lack of control of disease severity, the use of the convenience sampling method, time-consuming instruments, and limited statistical population. Therefore, the results should be used cautiously when generalized for patients with CHD in other circumstances. Therefore, study of the role of defense mechanisms and alexithymia in patients with CHD in other samples and other types of heart diseases is recommended. It is also suggested to use qualitative-quantitative and longitudinal designs in future studies by considering the role of other underlying personality traits in health-related QOL in patients with heart disease.
5.1. Conclusion
In general, the present study showed that defense mechanisms are indirectly involved in QOL of patients with CHD by affecting alexithymia. In addition, alexithymia is involved in predicting QOL in patients with CHD, both directly and indirectly, with the mediating role of psychological distress. These findings highlight the need for planning clinical trials and tailored intervention to manage emotions in order to modify alexithymia in patients with CHD. In addition, according to the results, it seems that patients with CHD have more immature defense mechanisms and lower skills for adapting to stressful events. Thus, it is recommended for these patients to receive coping skills education, such as training effective skills for coping with stress. Receiving appropriate interventions for patients with CHD requires progression of studies in this field, reforming methods and designing interventions, according to these findings by clinicians.