1. Context
Children’s health and diseases affect society and future generations’ wellness. Thus, consideration of children’s mental health helps their growth and fertility in adulthood (1). Attention deficient hyperactivity disorder (ADHD), diagnosed in child and adolescent psychiatric outpatient clinics, is the most common psychiatric disorder that appears in the early childhood and includes symptoms such as impulsive hyperactivity or inattention (2). Each one is defined based on several behavioral criteria: Hyperactivity is characterized by nervousness, restlessness, inappropriate running, not being able to play calmly, and wordiness; impulsivity can be observed in people, who shoot their mouth off, cannot wait for their turn, and cause inconvenience to others (3), and inattentiveness is characterized by carelessness, daily forgetfulness, as well as other attention-related problems. Accordingly, symptoms such as acute inattentiveness, hyperactivity-impulsivity, or both can be diagnosed as ADHD in children (1). These symptoms affect cognitive, academic, behavioral, social, and emotional functioning of the patients (4). These children are typically disabled and socially retarded. ADHD mainly affects boys; however, it can be observed in girls as well (5, 6). In the UK, strict diagnostic criteria have been developed to measure severe cases of ADHD and on the basis of those criteria, 0.1% of children have the disorder (7). Broader diagnostic criteria have been established in America based on which, the prevalence of ADHD has been varied from 2% to 20% among pre-school children, however, 3% to 5% are valid figures among schoolchildren. Moreover, the prevalence of ADHD among boys is three to five times more than its prevalence among girls (8). The occurrence of ADHD is high in Iran. In one study done by Tavakkolizade et al. it is reported about 9% (8). In another study, Yosefi estimated the prevalence of ADHD as 6.2% and 5.5% (in clinical re-evaluation) (9). ADHD is a neurobiological disease associated with self-esteem and social problems that typically occur in early childhood before the age of 7 and lasts at least for 6 months (10). Reported ADHD incidence among schoolchildren in America has been varied between 2% to 20%; however, 3% to 7% can be considered as a conservative estimation of ADHD incidence among pre pubertal schoolchildren (11). In another study conducted at Colombia University, Wilson and Levin reported that cases of ADHD accompanied by drug abuse have recently been observed in adults and elderly (12). ADHD has been cited as an important pathogenic factor of drug abuse and its continuation and even mentioned that if addicted people with ADHD were treated in their childhood, the risk of drug abuse could be prevented in their adulthood. Furthermore, treatment of ADHD in addicted individuals, even in their adulthood, may reduce their risk of returning to drug abuse (13). Numerous studies have been conducted on simultaneous problems faced by children with ADHD indicating the need for identification of these problems and conduction of more detailed epidemiology studies to intervene in and prevent simultaneous and secondary problems of children with ADHD. Some studies have been conducted in our country to determine the prevalence of ADHD in Iran. Awareness of students’ level of mental health can play an important role in planning to reduce the effects and consequences of ADHD and improvement of their mental health. In addition, it helps plan the allocation of funds for mental health services in a more effective manner in the society. Further knowledge on this issue would be valuable for the development of policies in the education sector. Given the importance of the issue, it seems that before making any plans, there is a need to obtain information regarding the prevalence of ADHD among schoolchildren.
2. Evidence Acquisition
2.1. Data Sources and Search Strategy
In this analysis, related articles published in scientific journals were found through searching the databases of Magiran, PubMed, Google Scholar, IranMedex, SID, Medlib, and ScienceDirect. Searching for articles was mainly done using systematic search and authentic keywords such as attention deficiency, hyperactivity prevalence, meta-analysis, Iran, etc., in both Persian and English languages.
2.2. Data Extraction
The standard method of data extraction was applied and for quality assessment, the variables including first author’s last name, year of publication, sample size, location, prevalence, and questioners’ type, were extracted from each paper. This article was written according to the PRISMA guidelines.
2.3. Study Selection
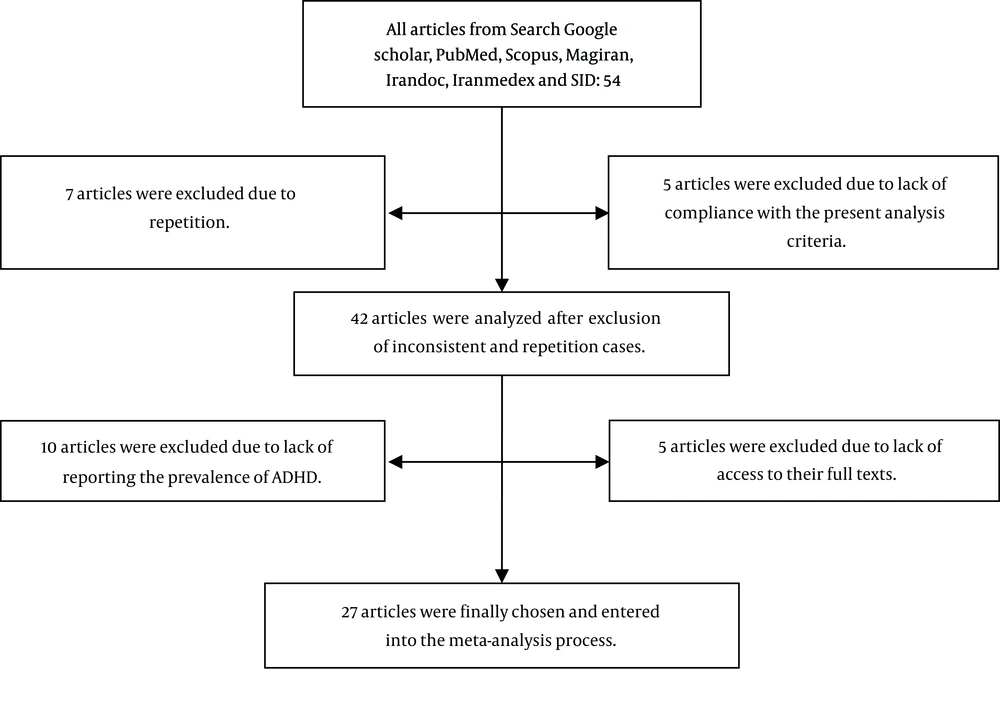
First, a list of the titles and abstracts of all available articles in the databases were prepared and then, related articles were evaluated and finally selected. The selected articles were independently entered into the analysis process. Out of the initial 54 studied articles, five were excluded due to lack of compliance with the present analysis criteria and seven due to being repetitions. Then, out of the remaining 42 articles, five were excluded due to lack of access to their full texts and unavailability of required data in their abstracts and 10 due to lack of reporting the prevalence of ADHD (Figure 1). A total of 27 articles were finally selected and entered into meta-analysis (1, 14-38). All data were first entered into a designed data extraction form and then, into the excel software. In the next stage, the data were transferred from excel to the R and STATA (version 11.2) software. Two independent authors conducted all of the above procedures; any disagreements were resolved by discussion.
2.4. Statistical Analysis
Given that the main focus of this study was to investigate the prevalence of ADHD, its variance was calculated through the binomial distribution (CI = 95%). To combine ADHD prevalence rates presented in different studies a weighted average was used. Accordingly, a weight was given to each study based on its inverse variance. To examine heterogeneity, Q test and I2 index were used. We also observed strong evidence of heterogeneity (I2 = 96.5%). In cases where the studies were heterogeneous, data were analyzed through meta-analysis (random effect model). Data analysis was done using R and STATA (version 11.2) software.
3. Results
To investigate the prevalence of ADHD in Iran, 54 articles were identified. In the next step and after screening, 27 eligible studies published between the years 2001 - 2016 were selected for the final analysis (Figure 1). The total sample size was 15124 primary school students whose ages ranged from six to 14 years old. The numbers of boys and girls were not specified in the analyzed studies; therefore, their numbers and percentages could not be included in the present study data analysis. Properties of the analyzed articles are presented in Table 1. Due to severe heterogeneity of reported prevalence (P < 0.001), meta-analysis was performed by using a random effect method.
| Author (Year Of Publication) | Reference | Location of Study | Sample Size | Prevalence of ADHD and Its Subtypes (%) | Questioners’ Type | ||
|---|---|---|---|---|---|---|---|
| Based on Parents’ Perspective | Teachers’ Perspective | Based on Parents and Teachers’ Consensus | |||||
| Solaiman nigad (2001) | (14) | Ilam | 2000 | T: 6.0 (5.0 - 7.0) | T: 4.8 (3.9 - 5.7) | T: 4.0 (3.1 - 4.9) | CSI-4 |
| Alishahi (2003) | (15) | Shiraz | T: 2182, B: 1083, G: 1099 | AD: 2.6 (2.0 - 3.3), HI: 1.6 (1.1 - 2.2), CT: 5.2 (4.3 - 6.2), T: 9.3 (8.1 - 10.5) | DSM-IV | ||
| Shams Esfandabad (2003) | (16) | Abhar | 600, 300, 300 | T: 43.3 (39.3 - 47.3) | NR | ||
| Ziauddini (2004) | (17) | Sirjan | 656, 322, 334 | T: 21.7 (18.5 - 24.9) | T: 32.7 (29.1 - 36.3) | T: 8.2 (6.1 - 10.3) | Rutter |
| Shabani (2005) | (18) | Zanjan | 428 | T: 49 (44.3 - 53.7) | Conners’ questionnaire | ||
| Akhavan Karbasi (2007) | (19) | Yazd | 400, 200, 200 | T: 16.3 (12.7 - 19.9) | DSM - IV | ||
| Shahim (2007) | (20) | Shiraz | 1311, 644, 667 | AD: 5.2 (4.0 - 6.4), HI: 5.0 (3.8 - 6.2), CT: 8.5 (7.0 - 10), T: 18.7 (16.6 - 20.8) | SWAN (DSM-IV) | ||
| Moradi (2008) | (21) | Neishabour | 722, 402, 320 | T: 12.5 (10.1 - 14.9) | Conners’ questionnaire | ||
| Ghanizadeh (2008) | (22) | Shiraz | 1600, 800, 800 | AD: 3.6 (2.7 - 4.5), HI: 5.0 (3.9 - 6.1), CT: 1.5 (0.9 - 2.1), T: 35.3 (33.0 - 37.6) | CSI-4 | ||
| Ghiasi (2008) | (23) | Ilam | 840, 470, 370 | T: 1.9 (0.9 - 2.8) | Rutter | ||
| Namdari (2009) | (24) | Khorram Abad | 945 | T: 3.2 (2.1 - 4.3) | CSI-4 | ||
| Najafi (2009) | (25) | Shiraz | 1205, 639, 566 | AD: 6.7 (5.3 - 8.1), HI: 6.0 (4.7 - 7.3), CT: 5.0 (3.8 - 6.2), T: 17.7 (15.5 - 19.9) | CSI-4 | ||
| Karimi (2009) | (26) | Esfahan | 450, 207, 243 | T: 2.4 (1.0 - 3.8) | SWAN (DSM-IV) | ||
| Arabi (2010) | (27) | Tehran | T:327 | T: 13 (9.4 - 16.6) | Rutter | ||
| Talaei (2010) | (28) | Mashhad | B:714 | AD: 4.6 (3.1 - 6.2), HI: 5.3 (3.7 - 7.0), CT: 5.3 (3.7 - 7.0), T: 15.3 (12.6 - 17.9) | Conners’ questionnaire | ||
| Alavi (2010) | (29) | Tehran | 799, 391, 408 | T: 8.6 (6.7 - 10.5) | SDQ | ||
| Bakhshi (2011) | (30) | Rasht | 181, 91, 90 | T: 17.7 (12.1 - 23.3) | T: 14.4 (9.3 - 19.5) | T: 7.7 (3.8 - 11.6) | Conners’ questionnaire |
| Meysamie (2011) | (31) | Tehran | 1403, 727, 676 | T: 25 (22.7 - 27.3) | T: 17 (15 - 19) | DSM-IV (CSI-4) | |
| Salehi (2011) | (1) | Arak | 2000, 1040, 960 | AD: 2.3 (1.6 - 3.0), HI: 3.5 (2.7 - 4.3), CT: 2.7 (2.0 - 3.4), T: 8.4 (7.2 - 9.6) | Conners’ questionnaire | ||
| Amiri (2012) | (32) | Tabriz | 1658, 877, 781 | AD:11.8 (10.2 - 13.4), HI: 15.8 (14 - 17.6), CT: 3.3 (2.5 - 4.2), T: 13.5 (11.9 - 15.1) | DSM-IV | ||
| Nejati (2012) | (33) | Tehran | 347 | AD: 6.8 (4.2 - 9.4), HI: 14.2 (10.5 - 17.9), T: 21.0 (16.7 - 25.3) | Rutter | ||
| Moayedi (2013) | (34) | Bandar Abbas | 800, 400, 400 | AD: 5.5 (3.9 - 7.1), HI: 3.1 (1.9 - 4.3), CT: 3.6 (2.3 - 4.9), T: 12.3 (10 - 14.6) | AD: 5.0 (3.5 - 6.5), HI: 3.5 (2.2 - 4.8), CT: 3.1 (1.9 - 4.3), T: 11.6 (9.4 - 13.8) | T: 4.4 (3.0 - 5.8) | CSI-4 |
| Zare Bahramabadi (2014) | (35) | Hamedan | 1938, 988, 950 | AD: 4.5 (3.6 - 5.5), HI: 2.7 (2.0 - 3.5), CT: 1.3 (0.8 - 1.9), T: 8.6 (7.4 - 9.9) | CSI-4 | ||
| Bahrami (2016) | (36) | Sanandej | 384, 198, 186 | AD: 8.3 (5.5 - 11.1), HI: 9.8 (6.8 - 12.8), CT: 6.7 (4.2 - 9.2), T: 24.8 (20.5 - 29.1) | CSI-4 | ||
| Safavi (2016) | (37) | Shahrekord | 631, 308, 323 | AD: 2.5 (1.3 - 3.7), HI: 3.3 (1.9 - 4.7), CT: 3.5 (2.1 - 4.9), T: 9.3 (7.0 - 11.6) | AD: 4.9 (3.2 - 6.6), HI: 3.5 (2.1 - 4.9), CT: 2.4 (1.2 - 3.6), T: 10.8 (8.4 - 13.2) | AD:5.9 (4.1 - 7.7), HI: 5.9 (4.1 - 7.7), CT: 5.5 (3.7 - 7.3), T: 17.3 (14.3 - 20.3) | CSI-4 |
| Bahreinian (2002) | (38) | Tehran | 624 | T: 19.9 (16.8 - 23) | DSM-IV (CSI-4) | ||
Abbreviations: AD, attention deficit subtype; B, boy; CSI-4, child symptom inventory-4; CT, combined subtype; G, girls; HI, hyperactive impulsive subtype; SDQ, strength and difficulties questionnaire; SWAN, strength and weaknesses of ADHD symptoms and normal behavior; T, total.
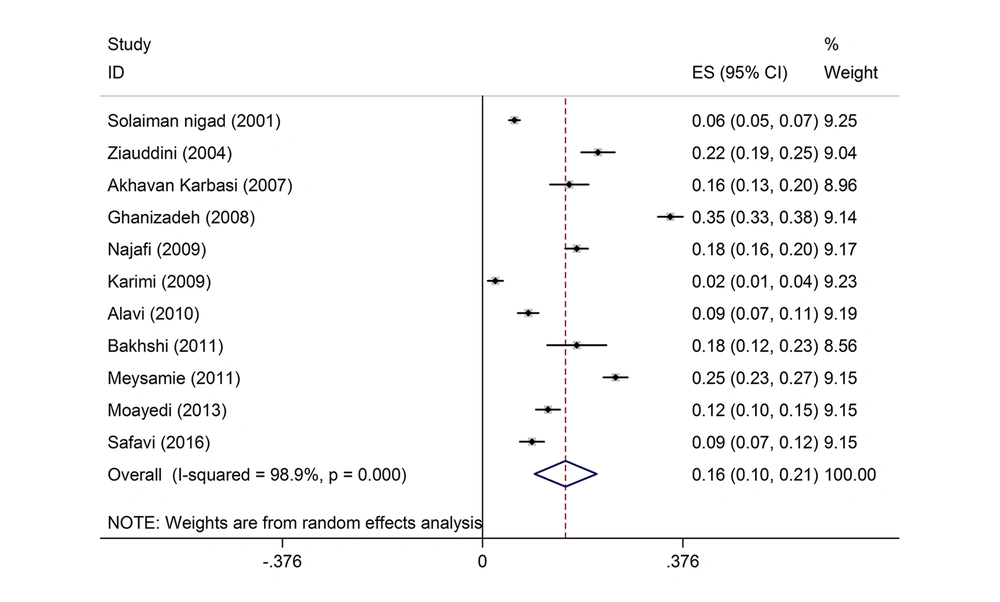
Table 2 presents the pooled estimations the prevalence of ADHD and its subtypes using meta-analysis of data extracted from studies in Iran. A total of 11 studies were included for the prevalence calculation based on parents’ perspective; accordingly, the prevalence of ADHD was 15.6% (CI 95%: 9.8 - 21.5) (Figure 2) and the subgroups’ prevalence were as follows: Attention deficit (AD) = 4.5% (CI 95%: 2.8 - 6.3), hyperactive impulsive (HI) = 4.4% (CI 95%: 3.0 - 5.7), and combined type (CT) = 3.4% (CI 95%: 1.6 - 5.1).
| Prevalence Based on Parents’ Perspectivea | Prevalence Based on Teachers’ Perspectivea | Prevalence Based on Parents and Teachers’ Consensusa | |
|---|---|---|---|
| Subgroup of ADHD | |||
| AD | 4.5 (2.8 - 6.3) | 6.3 (3.8 - 8.8) | 4.2 (2.6 - 5.9) |
| HI | 4.4 (3.0 - 5.7) | 7.5 (4.0 - 10.9) | 4.1 (2.9 - 5.4) |
| CT | 3.4 (1.6 - 5.1) | 4.8 (3.1 - 6.4) | 3.5 (1.8 - 5.2) |
| ADHD prevalence | |||
| Boy | 13.9 (7.6 - .20.0) | 10.5 (5.4 - 15.7) | 7.9 (5.9 - 10) |
| Girl | 9.05 (7.7 - 13.8) | 6.3 (3.4 - 9.2) | 5.5 (3.6 - 7.4) |
| Total | 15.6 (9.8 - 21.5) | 17.2 (12.7 - 21.8) | 12.0 (9.0 - 15.0) |
Abbreviations: AD, attention deficit subtype; ADHD, attention deficit hyperactivity disorder; CT, combined subtype; HI, hyperactive impulsive subtype.
aConfidence Interval 95%.
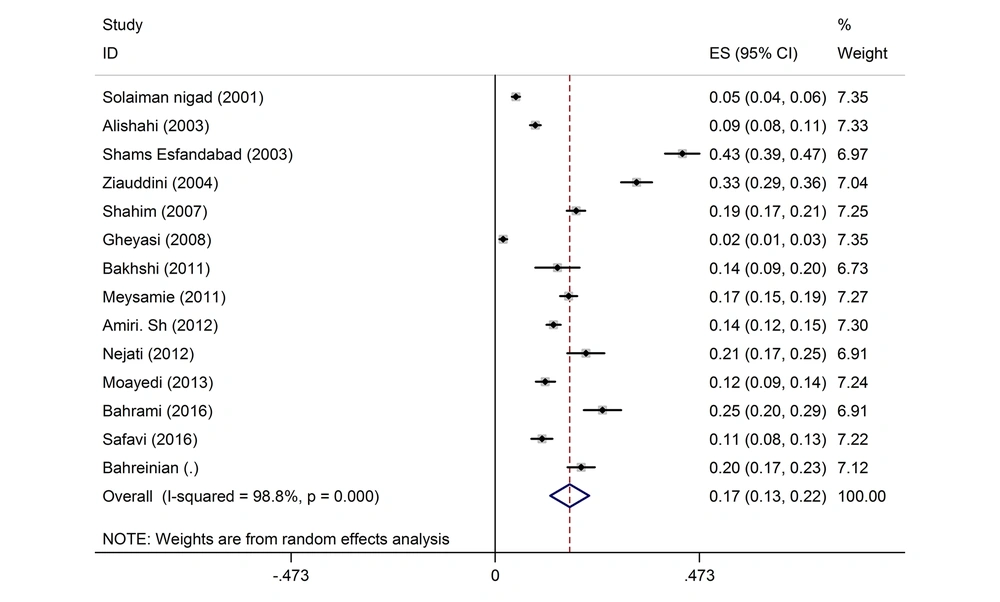
Among the included studies, we found 14 reports that were given according to the teachers’ perspective; the prevalence of ADHD was 17.2% (12.7 - 21.8) based on the teachers’ perspective (Figure 3) and the prevalence in its’ subgroups were as follows: AD = 6.3% (CI 95%: 3.8 - 8.8), HI = 7.5% (CI 95%: 4.0 - 10.9), and CT = 4.8% (CI 95%: 3.1 - 6.4).
To assess the prevalence of ADHD based on parents and teachers’ consensus, 13 studies were entered into the meta-analysis process and the prevalence was obtained 12% (CI 95%: 9.0 - 15). The subgroups’ prevalence rates, based on parents and teachers’ consensus, were as follows: AD = 4.2%, HI = 4.1%, and CT = 3.5%.
Table 2 shows the pooled estimations of ADHD based on gender; as it is seen, the prevalence of ADHD was greater among boys. These figures, based on the parents’ perspective, was 13.9% in boys versus 9.05% in girls, according to teachers’ perspective, was 10.5% in boys versus 6.3% in girls, and based on parents and teachers’ consensus, was 7.9% in boys versus 5.5% in girls.
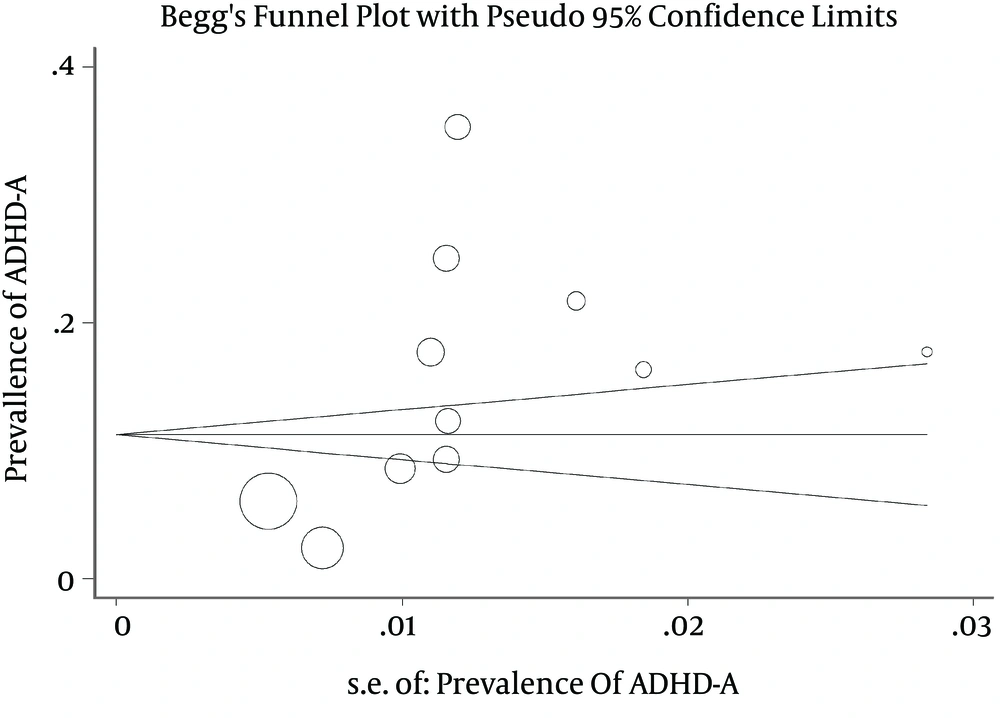
Figure 4 presents the funnel plot of the ADHD prevalence among Iranian children; no sign of publication bias was observed when the Begg’s funnel plot was examined. Regression analysis of this plot indicated no significant asymmetry and thus, no evidence of bias (Figure 4). The Egger and Begg’s tests revealed no evidence of publication bias (P = 0.799 ).
4. Discussion
This meta-analysis was conducted of studies addressing prevalence rates of ADHD to determine the prevalence of ADHD among schoolchildren in Iran. The results of the present meta-analysis are consistent with other studies done in Qatar with an overall prevalence of 9.4% (39) and in Germany (40), on a sample of 1077 schoolchildren, with an overall prevalence of 9.6%. Other studies have been done in Arabia (41) with the prevalence of 16.4% and in Brazil (42) with the prevalence of 13% in which, the reported prevalence of ADHD has been higher than the present study. Still, other studies have been conducted in Germany (43), with the prevalence of 5.3% and in Brazil (42), with the prevalence of 5.8% in which, the reported prevalence of ADHD has been lower than the present study. The prevalence of ADHD among children has been reported by the World Health Organization as 2% - 8% (44). In our study, the prevalence of ADHD, based on parents’ perspective, teachers’ perspective, and parents and teachers’ consensus, was 15.6%, 17.2%, and 12%, respectively; this result indicates a high frequency rate of ADHD among Iranian schoolchildren that requires specialized intervention and treatment.
Concerning gender ADHD was more prevalent in boys than girls indicating that boys have a higher chance of having ADHD than girls. A significant difference between boys and girls was observed in the frequency of ADHD; this finding is in accordance with a report by DSM-IV in which the prevalence of ADHD in boys has been reported as three times more than its prevalence in girls; however, it is consistent with another study done in Colombia (45) in which, it has been reported that 19.8% of boys and 12.3% of girls have obvious symptoms of ADHD. It is also in line with other studies conducted by Pineda et al. (46), Fontana Rda et al. (42), and Gomez et al. (47). In these studies, it was concluded that the prevalence of ADHD is significantly higher in boys compared to girls. Moreover, reference books and studies conducted in Brazil, India, Australia, America, and Colombia indicate the higher prevalence of ADHD among boys. According to studies conducted in Iran, ADHD prevalence is higher among boys and in some cities, the difference is statistically significant (P = 0.001); in addition, ADHD prevalence in boys is two times more than its prevalence in girls.
Higher prevalence of behavioral disorders, such as ADHD, in boys can be due to the fact that boys are generally more biologically vulnerable than girls. For example, male fetal death is more prevalent than female fetal death and boys are more vulnerable than girls to serious diseases, bad nutrition, and poverty. The differences that exist in fostering boys in the community influence this kind of vulnerability as well; for example, their aggressiveness is more tolerated than girls’ aggression. However, some evidence suggests that the higher prevalence of behavioral disorders in boys is due to the fact that their violence is more reported than girls due to the fact that parents usually exaggerate their male children’s behaviors and teachers are less tolerant to their hyperactivity, distractibility, and disorganization. This lack of tolerance toward boys’ behavior can be due to the difficulties that parents and educators encounter in managing them since their birth. Therefore, biological characteristics combined with social expectations can be considered as temporary growth crises in boys’ lives. This conclusion is reinforced when many of these childhood problems disappear without any treatment (25).
Regarding ADHD subgroups, in most of the studies conducted in different countries, many differences were observed in the type of impulsive attention deficiency and hybrid attention deficiency. However, in the present meta-analysis, fewer differences were identified between the ratios of attention deficiency, impulsive attention deficiency, and hybrid attention deficiency, which were not statistically significant despite their high prevalence.
It must be noted that the definition of ADHD disorder, sample size, instrument, validation methods, and diagnosis procedure have been different in different studies leading to diverse prevalence percentages. Furthermore, considering genetic factors, differences in ethnic structures and geographical, social, economic, and cultural factors in different examined communities, many of these different findings can be justified. Higher percentages were related to urban communities and western cultures. It seems that social crises, such as war (like in Iran), has been effective in ADHD prevalence (14). However, the common aspect of all studies is the high prevalence of ADHD among preschool and schoolchildren.
In this light, the long-term picture of children with ADHD is complex so that, without diagnosis and intervention, many of the problems associated with ADHD may turn into other disorders such as mood and anxiety disorders (3). With regard to the consequences of this disorder in children’s future and its unwanted effects on the quality of their social and individual lives, early screening and efforts for prevention and treatment of ADHD seems quite necessary. With reference to the relationships between ADHD and other psychiatric disorders and consequent poor school performance, consultation with children at risk of ADHD seems essential for diagnosis and treatment.
For assessing the risk of bias publication, it was detected by drawing Beggs funnel plot. This diagram shows that, there is a significant publication bias (P = 0.03). This means it is possible that studies with negative results have not been published. The results of this meta-analysis indicated that the prevalence of ADHD among schoolchildren is moderate; therefore, considering the importance of students’ mental health, the needs for identification, prevention, and treatment of high-risk groups by responsible institutions become obvious.