1. Background
Stafne bone cavity (SBC) is a bone depression of the mandible representing a group of concavities especially in the lingual surface of the mandible, where the depression is lined with an intact outer cortex (1-3). SBC is generally encountered incidentally on plain film radiographs with a cyst-like appearance and thus, they were referred to as pseudocysts historically; they are not true cysts because they do not have epithelial lining (2, 4). Plain film radiographs are often sufficient for diagnosis of SBC, but they may not be definitive when the lesion is atypical. Thus, in cases in which the plain film findings are not completely diagnostic, to establish a certain diagnosis and to distinguish SBC from other lesions, complementary diagnostic procedures may be necessary, and confirmatory evaluation of SBC with sialography, cone beam computed tomography (CBCT), computed tomography (CT) or MRI is warranted (2, 3, 5-10).
2. Objectives
The purpose of this study was to evaluate the imaging features of SBC presenting typical and atypical radiographic features and to show the contribution of different imaging techniques to diagnosis.
3. Patients and Methods
Seventeen patients who had lesions revealing an image compatible with SBC on panoramic radiograph were included in this study. All of the patients were admitted to our clinic with different complaints and none of them were aware of the lesion. All the lesions were detected incidentally on panoramic radiographs that were taken for diagnosis and treatment planning. Informed consent was obtained from the patients included in the study. In addition to panoramic radiography, there were also patients who were examined with lateral oblique mandible projection, CBCT and MRI.
4. Results
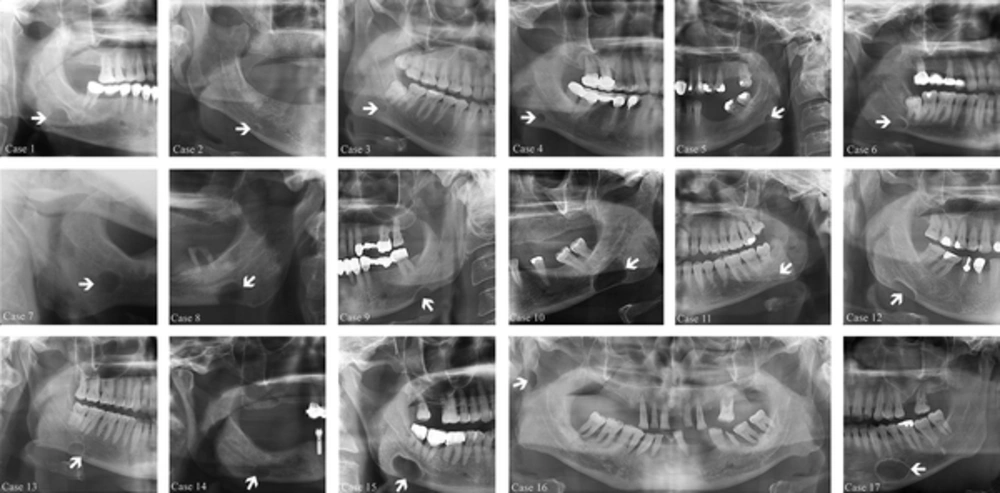
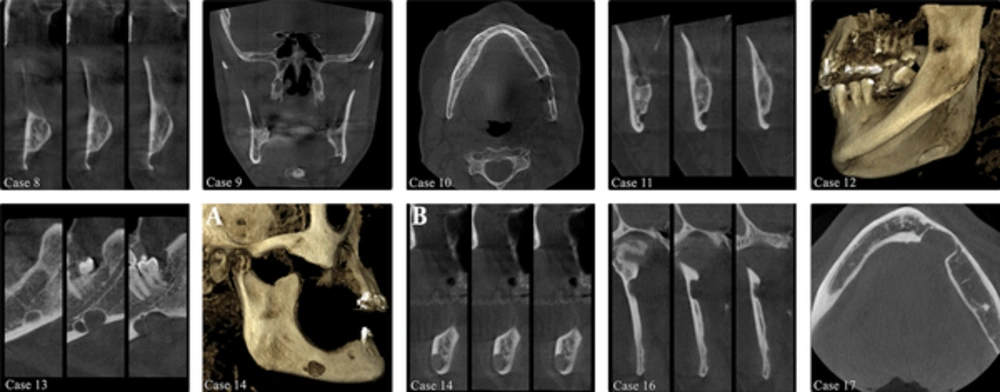
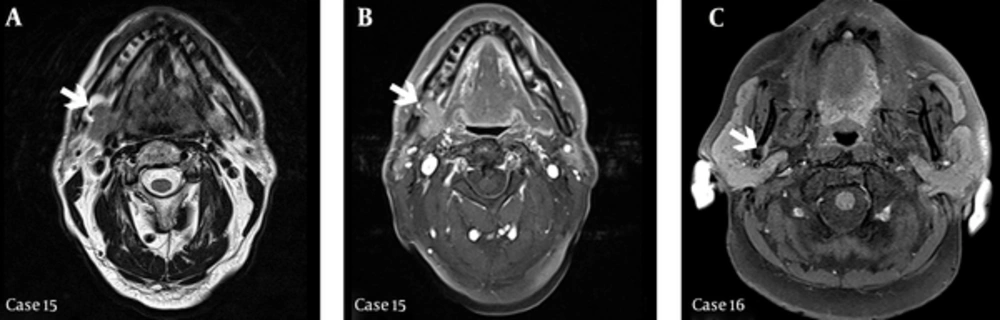
There were 13 male and four female patients with SBC cases presented in this study and their age range was 26 - 89 (56,82 ± 16,58). The demographic features of the patients and radiographic features of the lesions are shown in Table 1. SBC was diagnosed solely according to panoramic radiography findings in five cases. Figure 1 demonstrates cropped panoramic radiographs of 16 patients and cropped lateral oblique mandible projection of one patient. In addition to panoramic radiography, three patients were examined by lateral oblique mandible projection, nine patients with CBCT and two patients with MRI, as some of the lesions did not show the characteristic appearance of SBC. Five lesions had an unclear margin (case 8, 9, 12, 13, and 15), three lesions had great size (case 10, 15, and 17), two lesions had multilocular appearance (case 13, and 14), and two lesions had unusual location (case 16, and 17). In case 13, cropped panoramic radiograph demonstrates a well defined radiolucent lesion inferior to the mandibular canal, in the right posterior mandible (Figure 1). CBCT images revealed a bi-lobed SBC that was located on the lingual side of the mandible (Figure 2). In case 14, CBCT images revealed that the bi-lobed SBC was located on the buccal surface of the posterior mandible (Figure 2). In case 15, MRI sections revealed SBC on the angle of the mandible. In this case, the bone cavity was found to be filled with fat and soft tissue that is continuous and identical in signal with that of the submandibular gland (Figure 3). In case 16, MRI examination was also made the SBC was located in the ramus mandible and MRI sections revealed that the content of the cavity was fat tissue (Figure 3). In case 17, the SBC was located in the canine-premolar region of the left mandible, anterior to the mental foramen (Figures 1 and 2).
| Case Number | Age, y | Gender | Radiographic Examination | Location | Radiographic Features | Content |
|---|---|---|---|---|---|---|
| 1 | 45 | M | PR | R posterior mandible | round, corticated, radiolucent | - |
| 2 | 84 | M | PR | R posterior mandible | round, corticated, radiolucent | - |
| 3 | 26 | M | PR | R posterior mandible | round, corticated, radiolucent | - |
| 4 | 70 | M | PR | R posterior mandible | round, corticated, radiolucent | - |
| 5 | 44 | F | PR | L posterior mandible | ovoid, corticated, radiolucent | - |
| 6 | 44 | M | PR, LOMP | R posterior mandible | ovoid, corticated, radiolucent | - |
| 7 | 69 | M | PR, LOMP | L posterior mandible | ovoid, corticated, radiolucent | - |
| 8 | 89 | F | PR, CBCT | L posterior mandible lingual region | ovoid, corticated, radiolucent | - |
| 9 | 61 | M | PR, CBCT | L posterior mandible lingual region | ovoid, corticated, radiolucent | - |
| 10 | 56 | F | PR, CBCT | L posterior mandible lingual region | ovoid, corticated, radiolucent | - |
| 11 | 36 | F | PR, CBCT | L posterior mandible lingual region | round, radiolucent | - |
| 12 | 51 | M | PR, CBCT | R posterior mandible lingual region | ovoid, corticated, radiolucent | - |
| 13 | 50 | M | PR, CBCT | R posterior mandible lingual region | ovoid, bilobed, corticated, radiolucent | - |
| 14 | 72 | M | PR, CBCT | R posterior mandible buccal region | ovoid, bilobed, corticated, radiolucent | - |
| 15 | 65 | M | PR, LOMP, MRI | R posterior mandible lingual region | ovoid, corticated, radiolucent | salivary gland, fat tissue |
| 16 | 50 | M | PR, CBCT, MRI | R ramus mandible | ovoid, corticated, radiolucent | fat tissue |
| 17 | 54 | M | PR, CBCT | L anterior mandible lingual region | ovoid, corticated, radiolucent | - |
Abbreviations: CBCT, Cone Beam Computed Tomography; M, Male; F, Female; R, Right; L, Left; LOMP, Lateral Oblique Mandible Projection; MRI, Magnetic Resonance Imaging; PR, Panoramic Radiograph; y, years.
Cross-sectional (case 8, 11, 14b, and 16), and coronal (case 9), axial (case 10, and 17) sections of cone beam computed tomography (CBCT) images demonstrate that the lesion is a bone depression of the mandible, and is not a cyst cavity. Cross-sectional (case 13) CBCT images demonstrate that SBC is bilobed. Three dimension reconstructed CBCT images demonstrate Stafne bone cavity (SBC) on the lingual (case 12) and buccal (case 14) surface of the mandible.
Post contrast spin echo (SE) (3540/91, TR-TE) MRI axial section (case 15-a) and post contrast SE (385/8.7, TR-TE) with fat suppression MRI axial section (case 15-b) demonstrates the bony defect containing an extension of tissue from the submandibular gland on right angulus mandible (arrows). Post contrast SE (486/8.7, TR-TE) with fat suppression MRI axial section (case 16) demonstrates SBC on right ramus mandible (arrow).
5. Discussion
A description of 35 cases of lingual posterior variant of SBC was first given by Stafne in 1942 and then the author’s name was linked to this bone depression (2, 4). The terms that have been used to describe this entity are Stafne bone defect, Stafne cyst, static bone cavity, static bone defect, lingual mandibular bony defect, and lingual mandibular salivary gland defect (2, 3, 5, 6, 11, 12).
SBCs are typically seen on panoramic radiographs as unilocular, homogeneous, rounded or ovoid shaped, well-defined corticated, unilateral radiolucencies that range in diameter from 1 to 3 cm (2, 3, 5, 7). They localize between the mandibular first molar and the angle of the mandible below the inferior alveolar canal (8-10). In 2002, Philipsen et al. (1) reported four variants of mandibular bone depressions in a review article: the lingual posterior, the lingual anterior, the lingual ramus, and the buccal ramus depression. They have also mentioned that buccal anterior and buccal posterior bone depressions had been described (13, 14). The most common location of the defect is within the submandibular gland fossa between the mandibular angle and first mandibular molar tooth below the inferior dental canal and often close to the inferior border of the mandible. Similar defects have also been described between the incisor and the premolar teeth, below the root apices (when the teeth are present) and above the mylohyoid muscle (lingual anterior variant) and very rarely on the lingual/buccal surface of the mandibular ramus (ramus variant) (1, 2, 4, 6, 8, 9). In this study, most of the SBCs are located in the posterior lingual region of the mandible, but SBCs that are located in the buccal region, anterior region, ramus mandible are displayed as rare entities. Some variations of SBC such as bilateral lesions (3, 15), lesions above the inferior alveolar canal (5, 16), bilobate as two cases (case 13 and 14) in the present study (5, 17), trilobate (3), and lesions without sclerotic margins (5, 18) have also been described.
The incidence of SBC is 0.1% - 6.06% in different reports (1, 6, 8). The posterior lingual variant and the anterior lingual variant have an incidence of about 0.10-0.48%, and 0.009%, respectively (1, 2, 6). The age range is quite wide, but there is a peak incidence in the fifth-sixth decades with a male predominance (2, 6-8). In this study, the age range was 26 - 89 years (56,82 ± 16,58) and the majority of patients were male, in accordance with the literature.
SBC is generally diagnosed incidentally during the routine radiographic examination of the area. Because these concavities are asymptomatic, nonprogressive and almost impossible to palpate, patients do not usually present clinical symptoms and surgical treatment is not indicated (1-3, 5, 6, 8, 9, 11, 15). All of the SBCs presented in this study were detected during panoramic radiographic examination that was made for other reasons. In this study, in five cases, SBCs were readily differentiated from other pathoses on panoramic radiograph. In these cases, the lesions were located at the posterior mandible, below the inferior alveolar canal and had well defined sclerotic margins. Thus, additional imaging modalities were not required for these cases.
Although SBCs are identified usually on panoramic radiographs, lateral oblique mandible projections can also be helpful for diagnosis. Lateral oblique mandible projections are commonly used to examine the body or ramus of the mandible when panoramic imaging is not available or when an image with greater resolution is needed. However, two problems associated with lateral oblique mandible projection are image distortion and superimposition of the cervical vertebrae to the site of interest (2, 7). On the other hand, in case 7, cervical vertebrae were not superimposed on the site of interest and therefore, the radiograph was sufficient to diagnose the radiolucency as SBC.
When the lesion is atypical, to establish a certain diagnosis and distinguish SBC from other lesions, additional diagnostic procedures may be necessary (3, 5-9). CT, CBCT, and MRI are considered as the complementary imaging methods. CT is used as it is more specific to bone lesions and demonstrates the size and extent of the lesion. MRI is suggested for definitive diagnosis of SBC with the advantage of superior soft-tissue characterization, multiple imaging planes, different echo sequences and discrimination and determination of the content of the cavity without radiation exposure (3, 5, 6, 8, 11, 19). Sialography combined with plain radiographs or with CBCT has been suggested to confirm the diagnosis by demonstrating salivary gland tissue existing in the cavity. However, injection of the radiopaque contrast agent into the ductal system of a salivary gland is invasive and uncomfortable for the patient. It can also be difficult to perform especially for anterior variants of SBC because of multiple ducts in the sublingual gland (3, 5, 8). In this study, it was considered that CBCT and MRI were required with the reasons of unclear margin, great size, multilocular appearance, and location of the lesions. Therefore, the margins of the lesions, the relationship between the lesions and dental-anatomical structures were detected with CBCT and MRI. Contents of the lesions were determined with MRI. In this manner, histopathological examination was not considered and lesions of 11 cases were diagnosed as SBC with the aid of advanced imaging methods. In addition, since SBCs have been shown to be an anatomic structure rather than a pathological condition, radiological diagnosis with appropriate clinical follow-up rather than surgical intervention or biopsy is recommended (1).
It is thought that the content of SBC is consistent with salivary gland as the gland is located adjacent to these cavities and most reports have noted that SBC contain salivary gland tissue. Other tissues such as connective tissue, fat, lymphatic, muscular or vascular tissues have been found in the bone cavity and empty cavities have also been detected surgically or by advanced imaging methods (2, 3, 5, 7-9, 11). The salivary gland and fat tissue contents of the cavities in two of the presented cases are in accordance with the literature (5, 12, 19).
Although the appearance and location of the SBC are characteristic and the lesion is easily identified, various pathoses shown in Table 2 should be considered in the differential diagnosis (Figure 4). SBC can be differentiated from most of these lesions by being asymptomatic and radiographic characteristics including the appearance and location of the cavity (3, 5, 19, 20).
| Diagnosis |
|---|
| Focal Osteoporotic Bone Marrow Defect |
| Vascular malformation |
| Simple bone cyst |
| Dentigerous cyst |
| Keratocystic odontogenic tumour |
| Benign salivary gland tumours |
| Neurogenic tumours |
| Haemangioma |
| Myxoma |
| Multiple myeloma |
| Nonossifying fibroma |
| Fibrous displasia |
| Eosinophilic granuloma |
| Brown tumor of hyperparathyroidism |
| Ameloblastoma |
| Basal cell nevus syndrom |
| Giant cell tumor |
| Metastasis from a primary malignant tumor |
A, Panoramic radiograph demonstrates diffuse radiolucency similar to Stafne bone cavity (SBC) that is located in the right posterior mandible, below the inferior alveolar canal. B, Cross-sectional CBCT images demonstrate that the lesion shown in panoramic radiography (A) is a focal osteoporotic bone marrow defect located in the middle of the mandible which is a radiographic term indicating the presence of focal radiolucencies in areas where hematopoiesis is normally seen within the cancellous bone of the jaws.
Management of this defect is conservative with long-term radiographic follow-up. Atypical cases or other suspected lesions are evaluated with confirmatory three dimensional imaging methods and if necessary, biopsy should be performed for diagnosis (1, 3, 8, 9, 11, 15). All of the patients in this study were notified about the lesion and scheduled for follow-up (1, 3, 8, 9, 11, 15).
In recent years, imaging techniques such as CBCT and MRI have provided detailed information about definitive diagnosis of SBC in addition to panoramic radiographs. CBCT could be suggested as the suitable diagnostic modality for this bony configuration of the mandible because CBCT has the advantage of lower radiation dose compared to CT when suitable exposure parameters are selected. Also MRI is suggested to reveal the content of tissue extending into the bone cavity without surgical intervention.