1. Background
A central venous catheter (CVC) is a cannulation device that is located within the proximal third of the superior vena cava, inferior vena cava, or the right atrium. Catheters could be inserted through a peripheral vein or a proximal central vein, most commonly the internal jugular, subclavian, or femoral vein (1). Indications for using CVC include long-term injections of drugs (such as antibiotics, irritant drugs [e.g. cloxacillin] and chemotherapy), access for extracorporeal blood circuits (such as plasma replacement), central venous pressure measurement, central venous oxygen saturation measurement, pulmonary artery pressure measurement and parenteral nutrition (2).
Although CVC saves lives in many patients, its complications are noteworthy. Complications of thoracic and neck CVC such as infection (up to 26%), hematoma (up to 26%), and pneumothorax (up to 30%) have been reported previously (3). Incorrect placement of the thoracic catheter tip could also cause complications in 7% of the cases. After pneumothorax, malposition of the catheter tip is the second leading cause of mechanical injuries of CVC (4). Insertion of the CVC tip in the wrong vessel increases the risk of catheter wedging, erosion or perforation of vessel walls, local venous thrombosis, catheter dysfunction, and cranial retrograde injection, because the injected material is inserted to the head instead of the central circulation (5).
After catheterization, a chest X-ray (CXR) is necessary to evaluate the possible complications and the proper placement of the catheter. Based on guidelines, control by CXR should be done with the patient in supine position. Most of the radiographs performed for these individuals are taken in anterior-posterior (AP) view, which makes it difficult to interpret. Many of these patients may show variation in the shape of the heart shadow in the imaging due to heart failure and cardiomegaly, which also makes it difficult to pinpoint the exact location of the catheter tip. Pre-operative fluoroscopy may be used to check correct catheter positioning for long-term use and post-operative CXR is then required only if complications are suspected (6). The annual estimated cost for X-ray graphies is $155,000 (7). A definite diagnostic method for finding the location of the tip of the catheter is CXR. In many cases, in which radiography is contraindicated including pregnancy or the inability to transfer the patient to a radiology unit, it is necessary to use other diagnostic methods to determine the location of the tip of the catheter. One of these methods is ultrasonography (US), which in addition to being able to be used at the patient’s bedside, has lower costs and no radiation. Many studies have suggested the use of ultrasound as a suitable alternative to CXR (8-12). US has been used to reduce the complications of CVC before inserting a catheter for assessment of venous status (indirect US) and during catheter placement (real-time US) (11). The results suggest that US is a good alternative to X-ray imaging in terms of cost and time in adult and children (10, 11, 13).
2. Objectives
The present study was conducted in order to determine the diagnostic value of ultrasonography in determining the location of the CVC tip.
3. Patients and Methods
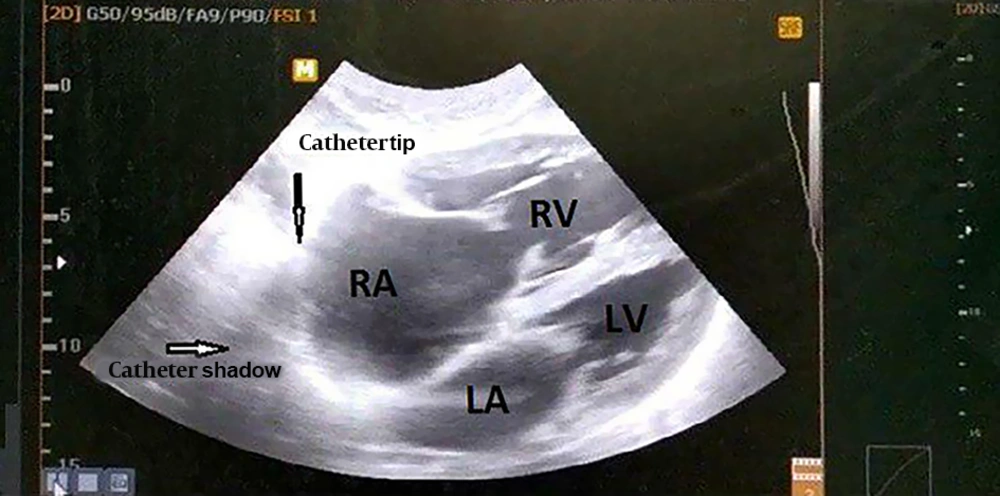
This was a cross-sectional analytical study conducted from 2017 to 2018 in Shahid Sadoughi Hospital affiliated to Shahid Sadoughi University of Medical Sciences, Yazd, Iran. This study was performed on candidates for CVC insertion for plasmapheresis or dialysis. This study was approved by the Ethics Committee of Yazd Shahid Sadoughi University of Medical Sciences. The exclusion criteria was age below 14 years, and insertion of the central catheter to the femoral vein. Written and informed consent was obtained from all participants. The catheter insertion was performed by the treating physician. A sonographer performed all ultrasonography procedures. US was performed by eZono 3000 portable ultrasound machine and by micro-convex probe 35 cl 20 (2 - 5 MHZ). The method used was extended FAST (eFAST) through subxiphoid 4-chamber view. First, the location of the catheter tip was evaluated via ultrasound in all patients who had undergone CVC placement after which patients were sent for a control chest radiography.
At the end, the diagnostic accuracy of US in determining the proper placement of CVC tip was determined considering CXR as the gold standard. Because of the lack of a better and more cost-effective alternative, x-ray is still used as the standard method for determining the location of CVC tip, although it has limitations. The demographic information (including age, sex, and body mass index [BMI]) and the location of the tip of the catheter (in US and CXR) were input in checklists and then data was analyzed by SPSS version 21 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp).
4. Results
Totally, 117 patients were included in the study. Sixty-two patients (53%) were male and 55 patients (47%) were female. The mean age of the patients was 59.63 ± 18.53 years. Based on CXR findings, the catheter tip was located in SVC in 104 cases (88.9%), while it was seen in the right atrium (RA) in 10 cases (8.5%), in the right ventricle (RV) in two cases (1.7%), and in the interventricular groove (IG) in one case (0.9%). By using US the proper view of the heart and the tip of the catheter were seen in 111 patients (94.4%) including 100 cases of catheter tip located in SVC (90.1%), nine cases located in RA (8.1%) and two cases located in RV (1.8%) (Table 1 and Figure 1). Catheter tip location was not seen in five patients (4.27%), because obtaining a heart view through the subxiphoid approach was not possible due to the patient’s anatomy. In one case, although the heart was seen in ultrasonography, the tip of the catheter was not seen and consequently, the tip of the catheter was seen in CXR. There was no significant difference between the mean of BMI in 111 patients (in whom the tip of the catheter was seen by using US [group one] A) with the six other cases (in whom the tip of the catheter was not seen by using US [group two]).
| Vein | Detected in CXR | |||
|---|---|---|---|---|
| SVC | RA | RV | IG | |
| Detected in US | 100 | - | - | - |
| Detected in US | - | 9 | - | - |
| Detected in US | - | - | 2 | - |
| Detected in US | - | - | - | 0 |
| Not detected in US | 4 | 1 | 0 | 1 |
| Total | 104 | 10 | 2 | 1 |
Abbreviations: CXR, chest X-ray; IG, interventricular groove; RA, right atrium; RV, right ventricle; SVC, superior vena cava; US, ultrasonography.
Based on the above mentioned points, the overall detection rate (sensitivity) of sonography for catheter tip was 94.9% (111/117); while, when the proper heart view through the subxiphoid approach was possible, the detection rate of the catheter tip by US was 99.1% (111/112). US is part of catheter insertion in our center, but the additional cost of CXR for recognizing the true catheter placement was $1 for each patient adding up to a total amount of $117. The complications of CVC insertion were not observed in any of the patients.
5. Discussion
Given the advancement of patient management in patients under emergency room supervision and the performance of procedures such as central venous catheterization in the emergency room, certain tools are needed to accurately locate the catheter position in the shortest possible time. In order to prevent further complications such as infection, mechanical trauma, long-term valvular damage, and clot formation, in case of displacement of the catheter, immediate correction of the error should be provided. In addition, by eliminating additional interventions, we could reduce the pain.
In this study, the sensitivity of US in showing the tip of the catheter was 94.4%, but in a similar study conducted by Matsushima et al., the sensitivity of ultrasound was totally 50% (14). The cause of sensitivity variability in similar studies may be due to risk factors such as a pre-existing central catheter. However, obesity, similar to the results we obtained, was not considered a risk factor in their study. Blans et al. (15) in 2016 in Netherlands conducted a similar study on 53 patients. US sensitivity was measured as 98%. Alonso-Quintela et al. (16) also conducted a study on bedside children. They compared CXR results with ultrasonography in malposition of catheter and they found that in 92% of cases, the results were consistent.
In our study, the time that was needed to detect the tip of the catheter by US was not compared with the time that was needed for detection by CXR. This had different reasons including technical problems; but in similar studies, this time was significantly shorter by using US compared with CXR. In a study conducted by Matsushima et al. (14), the time required for ultrasonography was 10.8 minutes versus 75.3 minutes needed for CXR. Alonso-Quintela et al. (16) also stated that to locate the CVC tip, US required less time than chest radiography (2.22 min vs 22.96 min). Duran-Gehring et al. (17) also mentioned that US took less time than CXR (5 min vs 28 min) and US was 24 minutes faster.
Chui et al. (18) conducted a cohort study from 2008 to 2015 on 6,875 patients in the Department of Anesthesia and Perioperative Medicine. They determined the incidence of pneumothorax and catheter misplacement after ultrasound-guided CVC insertion. They concluded that the complications of catheter insertion by US were low, therefore, CXR was not necessary afterwards due to the unnecessary extra cost for patients. In a study performed by Woodland et al. (7), similar results were obtained.
In our center, children’s emergency room was different from the adults, so, patients under 14 years of age were not included, but according to the study carried out by Alonso-Quintela et al. (16), US was the appropriate method to detect the tip of the catheter, also in children under 14 years old.
We did not use air contrast in US for better detection of the tip of the catheter due to its harmful effect, but in a study conducted in the emergency medicine department of Florida University, in 2015, air contrast was used alongside US to determine the location of the catheter tip and also to detect pneumothorax, and the results were the correct diagnosis of both the catheter tip location and pneumothorax (17). This study showed significant time saving and rapid attention to the treatment of critical patients.
US is part of catheter insertion in our center, but the additional cost of CXR for recognizing true catheter placement was $1 for each patient ($117 totally). The cost of CXR is cheap in our country, but in some countries, it is more expensive. In the study conducted by Matsushima et al. (14), the cost of CXR was $76 to $150 for each patient and therefore, $10000, totally. It was also expensive in the study performed by Chui et al. (18) ($105,000 to $183,000 per year). Therefore, by using US, the additional cost is saved.
Our study had a larger sample size than similar studies. However, due to technical problems, we were unable to measure the time required to perform ultrasound and compare it with X-rays. We suggested that a chest radiography should only be used to determine the location of the catheter tip when it is not possible to see the heart by US. Further studies with higher sample size are needed to confirm the feasibility of US replacement for CXR.
In conclusion, US is a cheaper method compared to CXR, and it is not harmful. The advantage of this study in comparison to similar studies is that air contrast agent was not used to determine the location of the tip of the catheter. We suggest that a chest radiography should only be used to determine the location of the catheter tip when it was not possible to see the heart by US. US has more sensitivity in the diagnosis of pneumothorax than chest radiography; therefore, if a diagnostic US is performed for detecting pneumothorax after CVC insertion, it is possible to set aside the control CXR request, especially in patients who are at risk due to hemodynamic instability.