1. Context
Coronavirus disease 2019 (COVID-19), caused by a novel coronavirus, was first reported from Wuhan city, China, in December 2019 and rapidly spread across the world (1, 2). The virus was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (3). Pneumonia is the most serious manifestation of COVID-19 that mainly affects the respiratory system (1). As the infection evolves, various computed tomography (CT) scan manifestations may appear. Being familiar with these diverse CT findings is important as currently the infection has reached a pandemic; especially in centers that laboratory tests may not be easily accessible.
2. Evidence Acquisition
A wide spectrum of CT findings has been reported in COVID-19 pneumonia. Abnormal findings on chest CT could be unilateral or bilateral with single or multilobar involvement. Additionally, the lesions can have various distribution patterns (central, peripheral or diffuse) (2). In this pictorial review, we present various manifestations of COVID-19 pneumonia on chest CT scans of 14 patients with positive polymerase-chain reaction (PCR) assay for COVID-19. Wherever possible, we describe the CT findings using the standard nomenclature presented by the Fleischner Society as glossary of terms for thoracic imaging (4). The common radiologic findings on chest CT scan of patients with PCR-positive assay for COVID-19 are as follow:
2.1. Ground Glass Opacity and Consolidation
Most of the studies reported isolated ground glass opacity as the most frequent finding in COVID-19 pneumonia. According to a systematic review (1), bilateral multilobar ground glass opacities with a peripheral or posterior distribution, mainly in the lower lobes are known features of COVID-19 pneumonia on the initial CT scan. Combination of ground glass and consolidative opacities is a less frequent presentation that is mainly reported in older patients (1). Ground glass opacity is presented in cases 1 to 10, 12, and 13. Consolidation is presented in cases 6 to 12 and 14.
2.2. Air Bronchogram
Air bronchogram, as defined by Fleischner Society, is a pattern of air-filled bronchi within a surrounding opaque lung. Consolidation that is a type of increased lung attenuation due to alveolar-filling processes could occur with or without air bronchogram (4). It has been described in up to 80% of patients with COVID-19 pneumonia (5). Air bronchogram is depicted in case number 7.
2.3. Vascular Dilation or Thickening
Vascular dilation occurs in small vessels within or around a lung parenchymal lesion like a ground glass opacity or consolidation. A recently published study reported vascular thickening in 80% of cases (6), although in other studies it has been reported as a less frequent finding. Vascular dilation is presented in case number 10.
2.4. Reticular Pattern
The reticular pattern as a dominant pattern (including coarse linear or curvilinear opacity or fine sub-pleural reticulation) is a late and rare finding (7). Moreover, the presence of reticular opacities in combination with other findings has been described as a common presentation of COVID-19 pneumonia especially in the late stage (3). Enlarged fibrous stripes refer to the interstitial septal thickening (1). Small number fibrous stripes are seen in early stages of COVID-19 pneumonia. Nevertheless, in advance stages, more and enlarged fibrous stripes are presented (8, 9). Reticular opacities are presented in cases 4, 6, 11, and 12.
2.5. Crazy Paving
Crazy paving pattern refers to ground glass opacities associated with thickened intralobular and interlobular septum (4). It is a common pattern in early stages of COVID-19 (8). In addition, development of crazy paving pattern could be seen in intermediate stages of the infection (1). Crazy paving pattern is depicted in case number 10.
2.6. Bronchial Wall Thickening and Bronchiectasis
Bronchial wall thickening and bronchiectasis are seen less commonly in COVID-19 pneumonia and are more frequent in later stages (2). Bronchiectasis is presented in case number 2 and bronchial wall thickening is seen in case number 14.
2.7. Halo Sign
The halo sign is the ground-glass opacity surrounding a mass or nodule (4). Han et al. (6) reported the halo sign in about 65% of cases, but other studies reported this sign as a rare finding in COVID-19 pneumonia (1). Halo sign is presented in case 7.
2.8. Reversed Halo Sign
The reversed halo sign is defined as a central focal area of ground glass opacity surrounded by a complete or incomplete ring of consolidation (4). It has been more reported in later stages of COVID-19 pneumonia (10). The reversed halo sign is presented in case number 8.
2.9. Rare Findings
Mediastinal and hilar lymph node enlargement, discrete/centrilobular pulmonary nodules, pleural thickening, and pleural and pericardial effusion are uncommon findings in CT scan of patients with COVID-19 pneumonia (11, 12). Pleural thickening is presented in case number 13. Pleural effusion is noted in case number 11.
3. Results
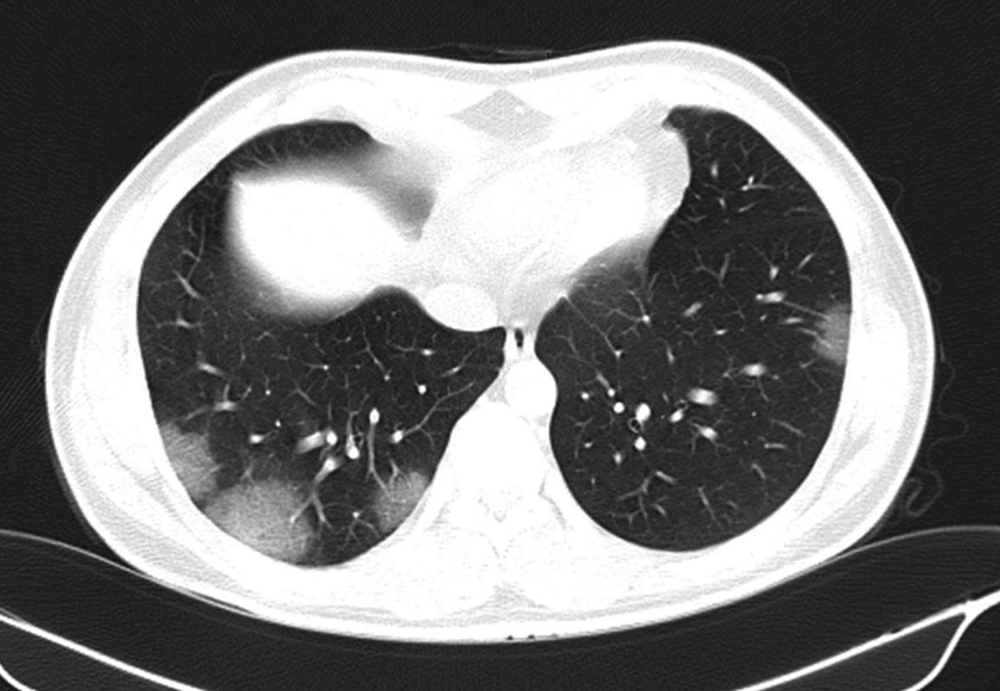
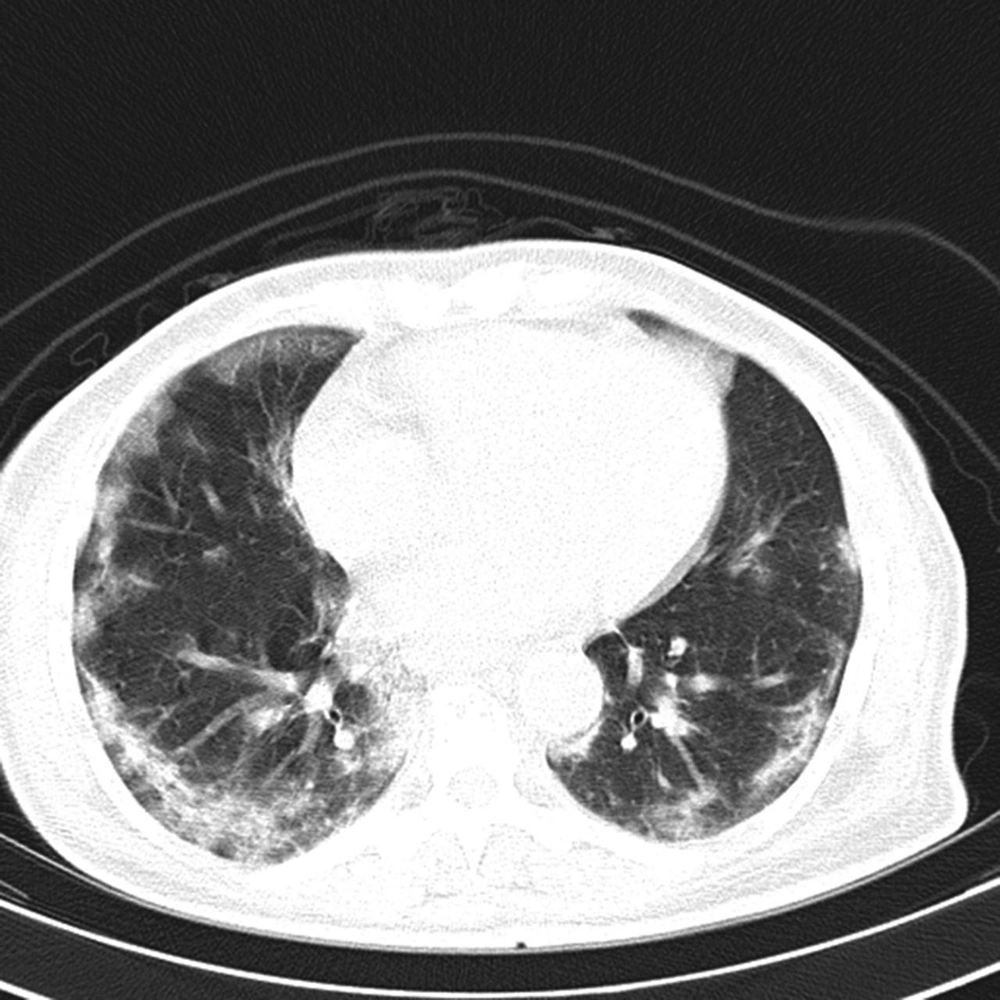
3.1. Patient 1
COVID-19 pneumonia was diagnosed in a 34-year-old man who presented about 48 hours after the onset of fever, non-productive cough, dyspnea and myalgia. Blood oxygen saturation on admission was 94%. Unenhanced CT scan of the chest at the time of admission demonstrated multiple peripheral patchy ground glass opacities with bilateral distribution (Figure 1).
3.2. Patient 2
The patient was a 65-year-old woman with COVID-19 pneumonia who presented with fever and cough. Blood oxygen saturation on admission was 93%. CT scan obtained on day 4 of admission showed bilateral peripheral and sub-pleural consolidative opacities mainly in the lower lobes. Scattered bronchiectasis was noted (Figure 2).
3.3. Patient 3
The patient was a 72-year-old female with COVID-19 pneumonia who presented with fever and shortness of breath. Blood oxygen saturation on admission was 78%. Unenhanced CT scan of the chest indicated extensive ground glass opacities in both lungs (Figure 3).
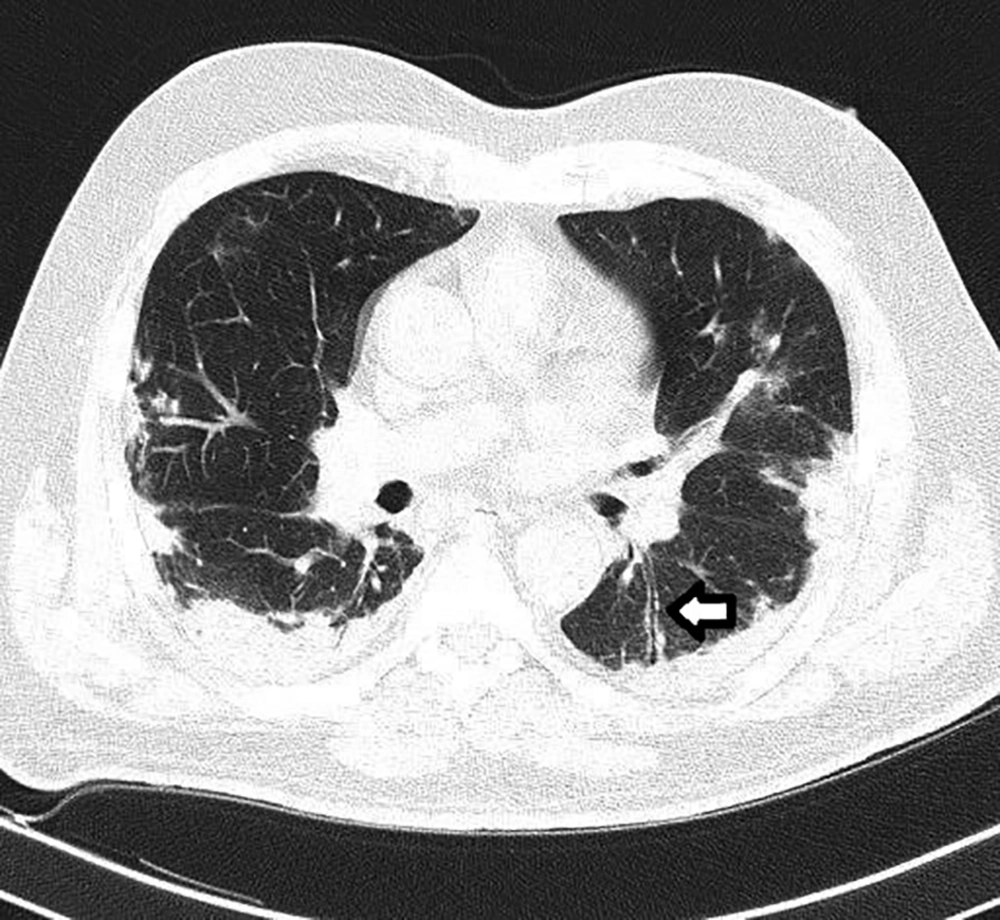
3.4. Patient 4
This is a COVID-19 pneumonia in a 36-year-old female who presented with dyspnea and flu-like symptoms. Her initial oxygen saturation was 95% under ambient air. Spiral CT scan of the thorax revealed patchy sub-pleural ground glass and reticular opacities in both lower lobes (Figure 4). Moreover, situs inversus totalis was noted. The patient did not have any history of recurrent pulmonary or sinonasal infection suggestive of primary ciliary dyskinesia.
3.5. Patient 5
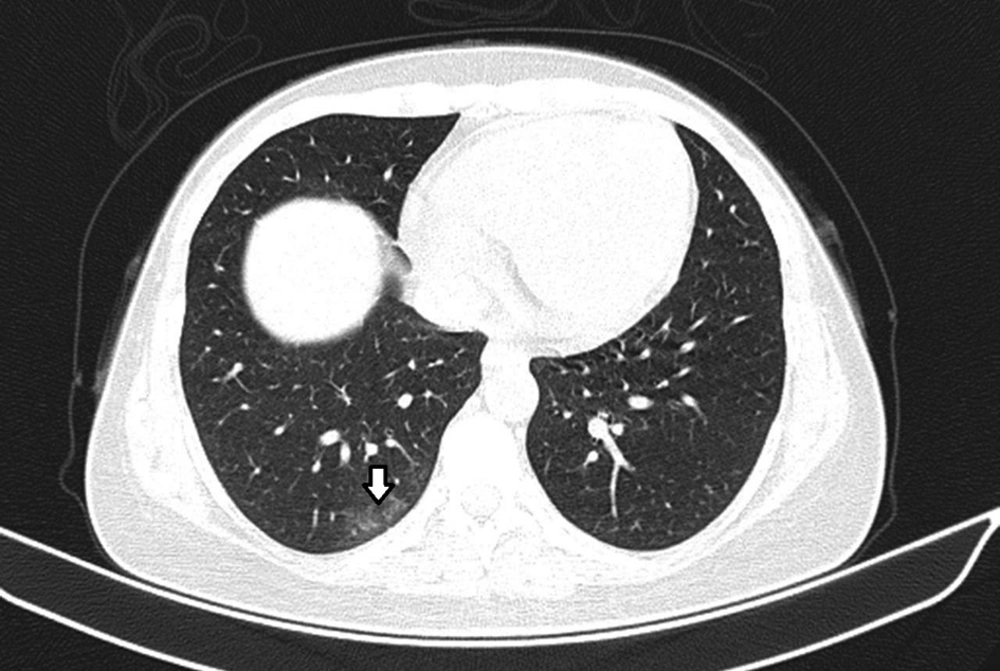
The patient was a 36-year-old female who presented with cough and low-grade fever. Spiral CT scan of the chest at the time of admission demonstrated solitary peripheral ground glass opacity in the posterior segment of the right lower lobe (Figure 5).
3.6. Patient 6
The patient was a 68-year-old female with diabetes mellitus (DM) and ischemic heart disease (IHD) who presented with cough, fever, and chills. Blood oxygen saturation on admission was 94%. Spiral CT scan of the chest at the time of admission showed bilateral mixed ground glass opacities and consolidation associated with air bronchogram in the upper zones. Reticulation and peripheral linear strip were noted in the basilar segments of both lungs (Figure 6).
3.7. Patient 7
The patient was a 36-year-old female who presented with non-productive cough and fever. Blood oxygen saturation was 94% on admission. Spiral CT scan of the chest showed a patch of airspace consolidation with air-bronchogram and peripheral ground glass opacity (halo sign) in the right upper lobe (Figure 7).
3.8. Patient 8
The patient was a 35-year-old man that complained of fever, cough, shortness of breath and sore throat. His initial blood oxygen saturation was 87% in room air. Spiral low dose CT scan of the chest revealed patches of ground glass opacities and consolidation mainly in sub-pleural regions of both lungs, some of them representing a reversed halo sign (Figure 8).
3.9. Patient 9
The patient was a 66-year-old female with DM, hypertension and chronic kidney disease. She presented with dyspnea and blood oxygen saturation was 92%. Her baseline CT scan of the chest showed peripheral rim of mixed ground glass and consolidative opacities in both lungs that spared the juxta-pleural line (Figure 9).
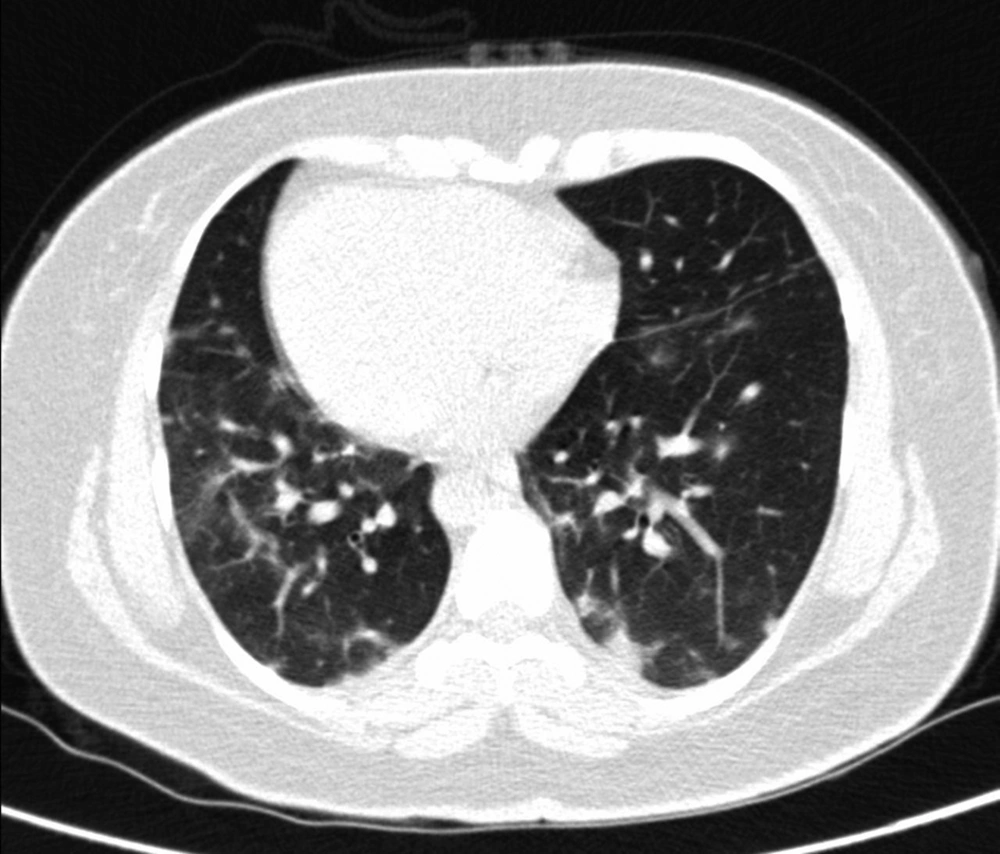
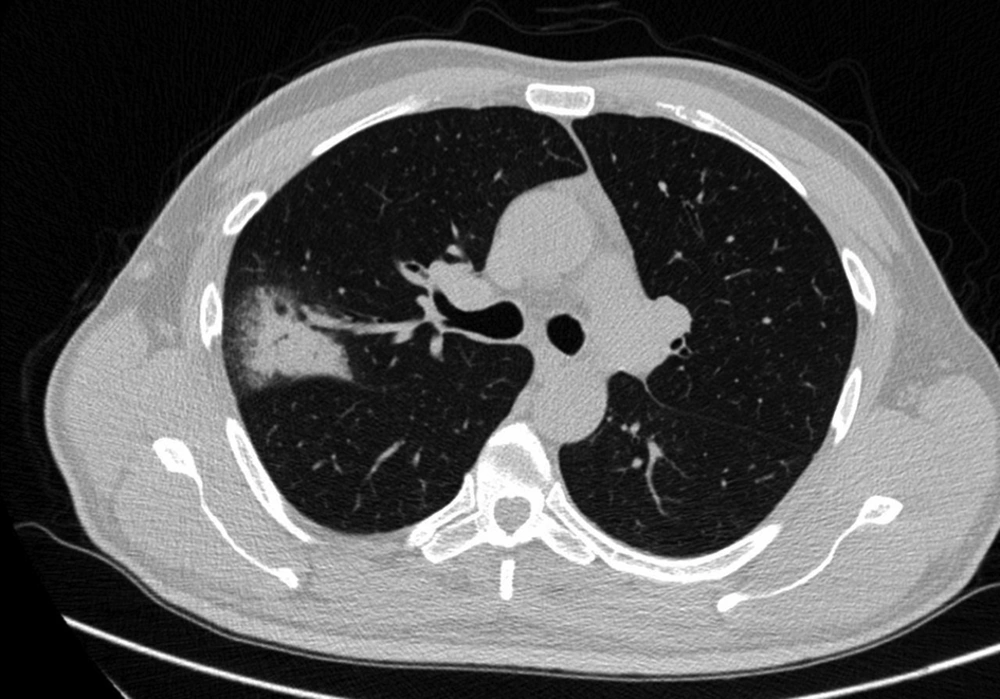
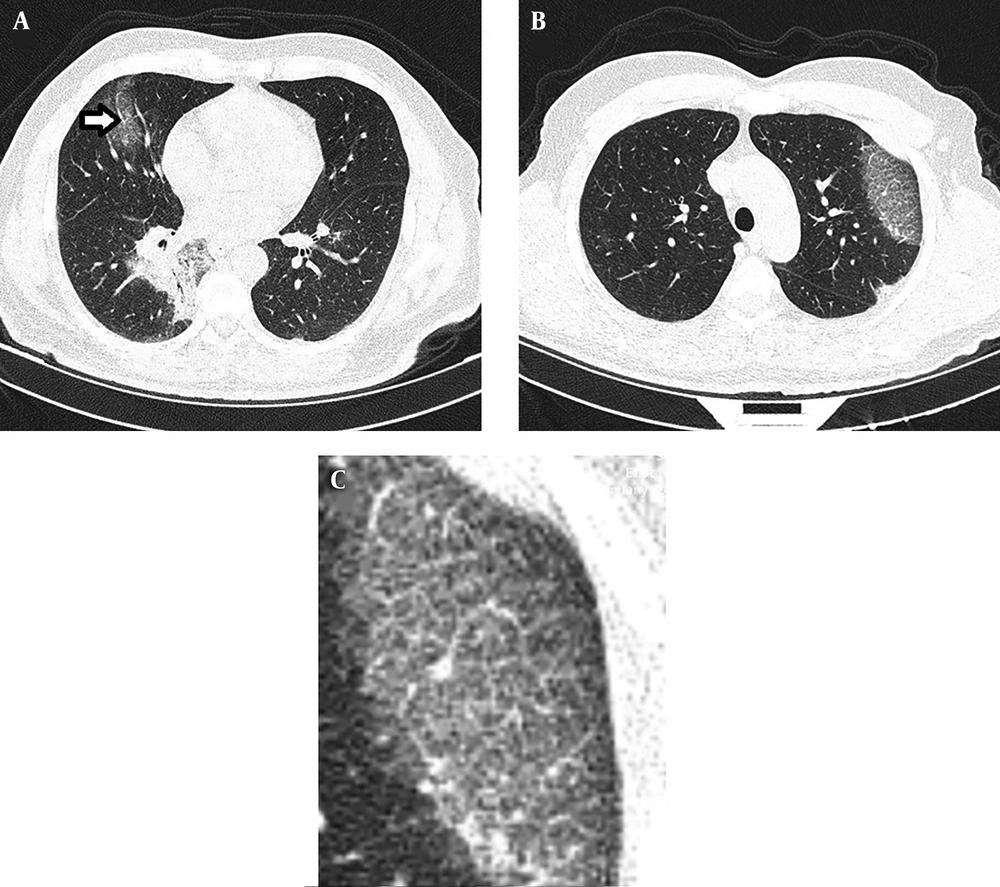
3.10. Patient 10
COVID-19 pneumonia was diagnosed in a 54-year-old man with a 3-day history of cough and fever. Oxygen saturation was 93% under ambient air. CT of the thorax revealed patches of peripherally distributed ground glass opacities as well as consolidation throughout both lungs (Figure 10A). Ground glass opacity in the left upper lobe was associated with thickened intralobular and interlobular septum (crazy paving) (Figure 10B and C). Vascular dilatation was noted within the ground glass opacity of the right upper lobe.
A, Patches of peripherally distributed ground glass opacities as well as consolidation throughout both lungs. Vascular dilatation is noted within ground glass opacity of the right upper lobe (arrow). B and C, Ground glass opacity in the left upper lobe is associated with thickened intralobular and interlobular septum (crazy paving).
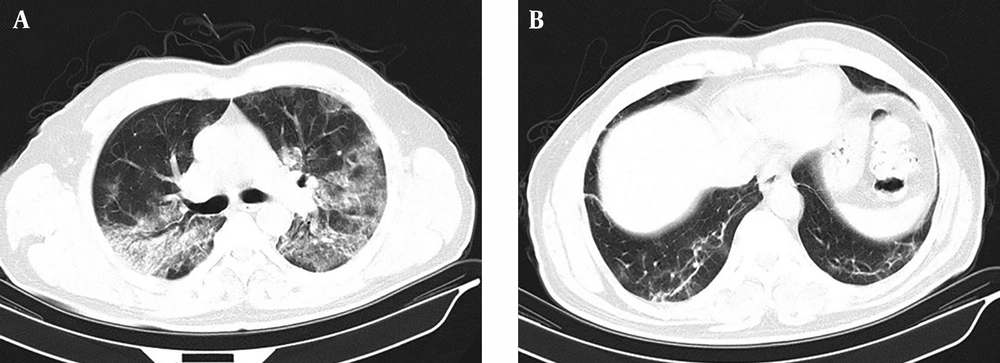
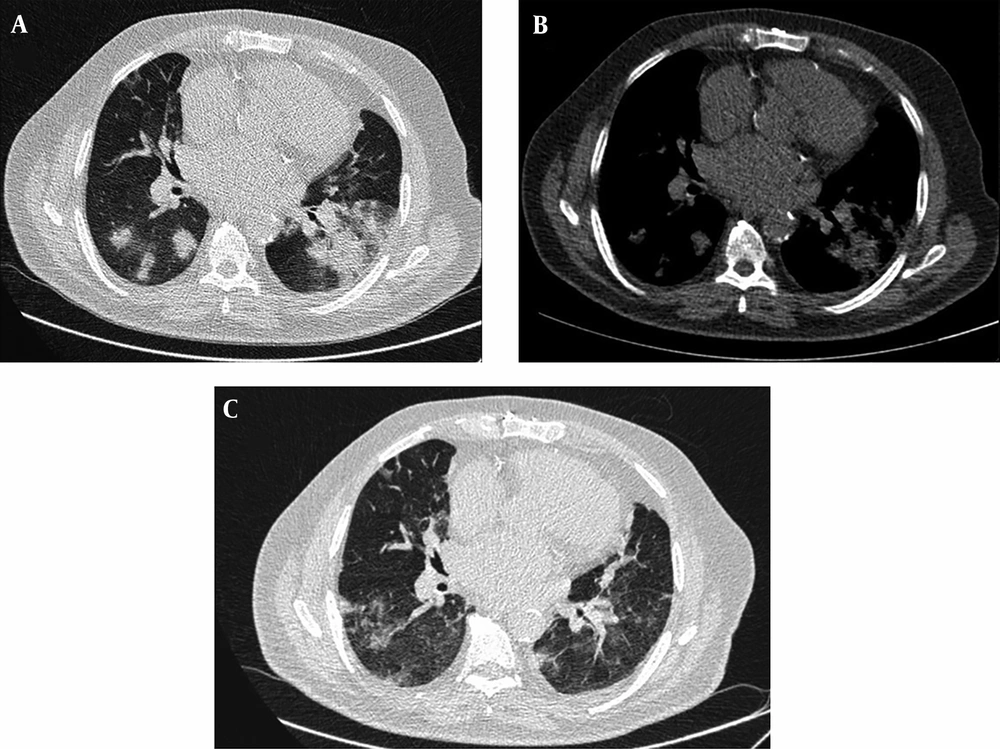
3.11. Patient 11
An 80-year-old male presented with dyspnea and fever. Blood oxygen saturation was 94% in room air. His past medical history was significant for IHD and chronic obstructive pulmonary disease (COPD). Initial spiral low dose CT scan of the thorax revealed patchy air-space consolidation with minimal left sided pleural effusion (Figure 11A). In follow up CT scan that was performed 8 days later, most of the air-space consolidations disappeared. Areas of patchy reticular and ground glass opacities in sub-pleural regions of both lungs were noted (Figure 11B and C).
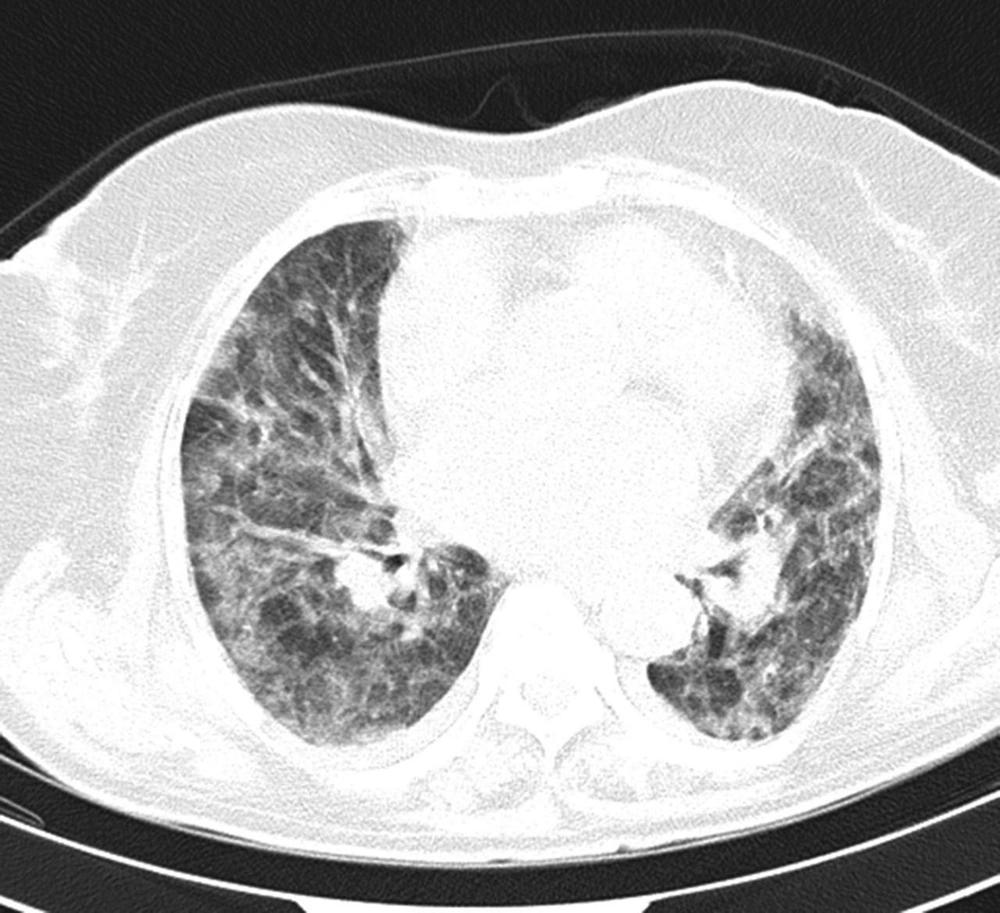
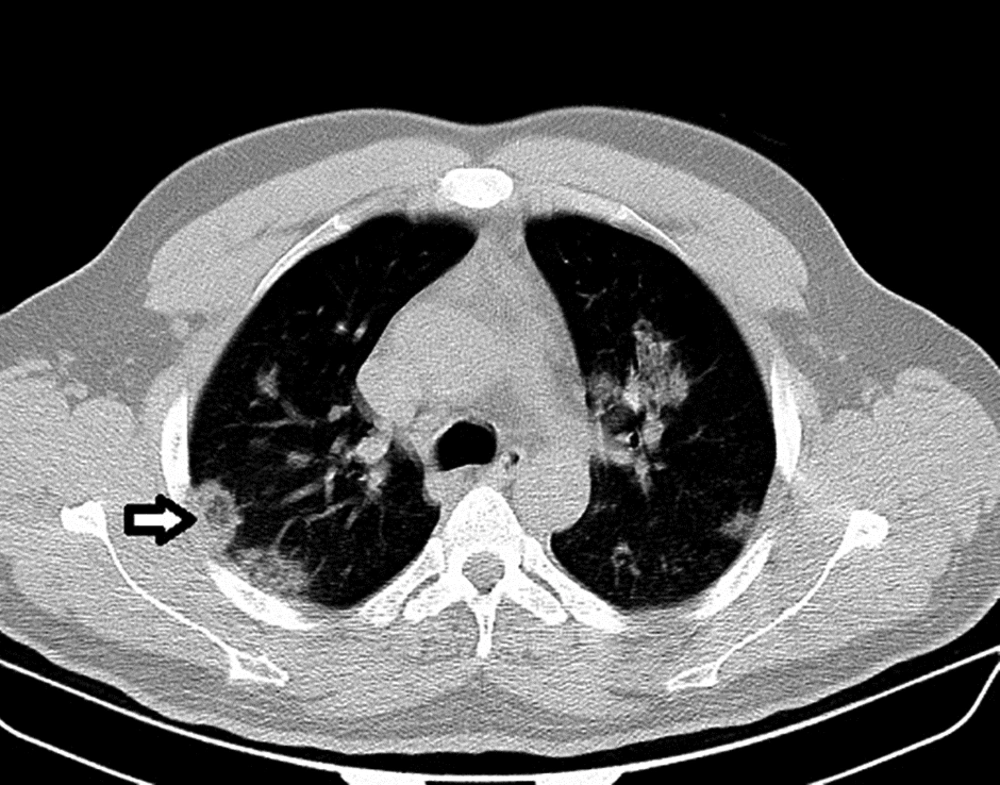
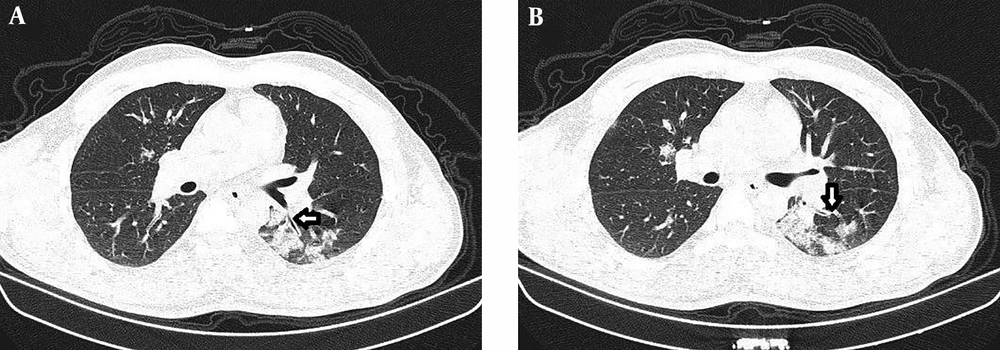
3.12. Patient 12
The patient was a 66-year-old male who presented with fever, dyspnea and oxygen saturation of 88%. Initial spiral low dose CT scan of the thorax revealed diffuse patchy ground glass opacities and consolidation involving most of the both lungs’ parenchyma that was compatible with diffuse alveolar damage (Figure 12A). After 8 days, the second CT scan was obtained. Ground glass opacities and consolidations were reduced but increased reticular opacities were noted (Figure 12B).
A, Diffuse patchy ground glass opacities and consolidation involving most of the both lungs’ parenchyma that is compatible with diffuse alveolar damage. B, After 8 days, a second CT scan was obtained. Ground glass opacities and consolidations were reduced but increased reticular opacities are noted.
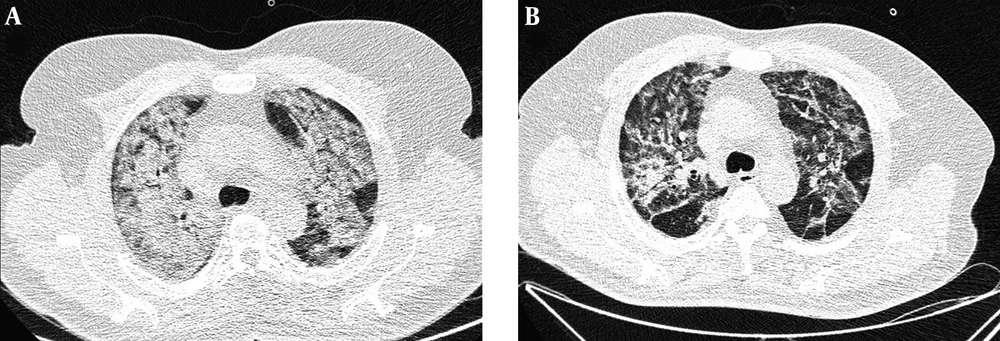
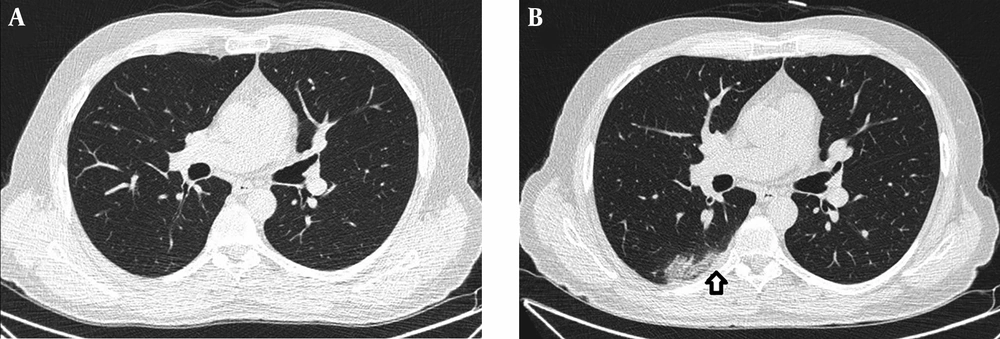
3.13. Patient 13
A 45-year-old man presented about 36 hours after initiation of fever and cough. Initial spiral CT scan of the thorax without contrast did not show any abnormality (Figure 13A). He tested positive for COVID-19 and underwent outpatient therapy. Despite the cessation of fever and reduction of cough and myalgia, the patient returned with pleuritic chest pain located in the right parasternal region 15 days after disease onset. A second CT scan of the thorax was obtained that showed patchy ground glass opacities in both lungs, of which some were located adjacent to the pleura (Figure 13B). Minimal thickening of the pleura was noted.
3.14. Patient 14
The patient was a 66-year-old man with a history of seizures. He presented with dyspnea. His oxygen saturation was 92%. His baseline chest CT scan showed mixed ground glass and consolidative opacities in the left lower lobe (Figure 14A and B). Bronchial wall thickening was noted within and around the lesion.
4. Conclusion
As COVID-19 outbreak spreads and many patients who present to the medical centers have respiratory symptoms, chest CT scan is helpful in the management of patients. Radiologists can use the presented cases and images in this pictorial review to improve their skills in the diagnosis of COVID-19 pneumonia.

.png)