1. Background
A new member of coronavirus family, called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is responsible for the new emerging viral pneumonia, known as coronavirus disease 2019 (COVID-19) (1-3). Today, real-time reverse transcription-polymerase chain reaction (RT-PCR) of respiratory tract specimens is known as the reference standard for diagnosis of SARS-CoV-2 infection (4). Due to different intrinsic limitations, such as sampling, transportation, and diagnostic kit performance, the sensitivity of RT-PCR for detecting COVID-19 ranges from 60 to 71% in the initial presentation (5-8).
Old age and comorbidities, such as cardiovascular and pulmonary diseases and diabetes, have been recently proposed as prognostic factors for COVID-19, causing more complications and exacerbating the disease (9-11). According to previous studies, laboratory findings and biomarkers, such as C-reactive protein (CRP), D-dimer, CD8 T lymphocyte count, N-terminal prohormone of brain natriuretic peptide (NT-proBNP), interleukin-6 (IL-6), and procalcitonin may play a prognostic value in COVID-19 (9, 10, 12, 13).
Chest computed tomography (CT) scan plays an increasingly important role in the early detection of COVID-19. It is used to estimate the clinical course and outcomes of COVID-19 in patients (14). A recent study showed that the well-aerated lung (WAL) percentage, assessed by chest CT scan upon admission, is correlated with improved clinical outcomes in COVID-19 patients. To give an example, patients with WAL< 73% were 5.4 times more likely to be admitted to the intensive care unit (ICU) or expire (15).
2. Objectives
This study aimed to evaluate the prognostic significance of quantitative chest CT scan in COVID-19 patients. We analyzed the patients’ initial chest CT scans and scored the lung involvement using two methods:
- Total lung involvement score (TLI): Each lobe was scored from 0 to 4 based on the percentage of involvement, according to a study by Hani et al. (16).
- Modified TLI: Each lobe involvement was first multiplied by the number of lobe segments, and the sum was suggested as the modified TLI. The correlation between the recorded scores and outcomes of COVID-19 was evaluated in four groups: patients admitted to hospital wards, patients admitted to the ICU, patients intubated during hospitalization, and expired patients.
3. Patients and Methods
3.1. Study Participants
This cross-sectional study was conducted according to the principles of the declaration of Helsinki and our institutional review board (IR.MUMS.REC.1399.029). No informed consent form was obtained from the participants because of the retrospective design of this study. Patients with laboratory-identified COVID-19 based on real-time RT-PCR were included in this study between May 2020 and June 2020. The clinical data included age, sex, and admission ward. Patients with pathological findings other than those related to COVID-19 in chest CT scans (e.g., pattern of lung involvement compatible with tuberculosis and pulmonary fibrosis) were excluded from the study; also, patients with missing data were eliminated.
3.2. Chest CT Scan
We used the available chest CT scans of patients in a referral hospital for COVID-19 during the pandemic. The CT scans were obtained using a 16-row multidetector scanner (NeuViz 16 Classic CT, Neusoft Corporation, Shenyang, China; http://www.neusoftmedical.com/) with the following parameters: (1) 120 kVp, (2) 40 mA, (3) 1.5 mm collimation, (4) 1.35:1 pitch, (5) a sharp kernel (B80f), (6) reconstruction matrix of 512 × 512, (7) slice thickness of 1.0 mm, and (8) high-spatial-resolution algorithm. All images were analyzed by two experienced chest radiologists with more than ten years of experience, who were blinded to the clinical data.
The lung lesion features, including the number of involved lobes and the distribution of lesions in different lobes, were evaluated in each patient. We considered the lingula as a separate lobe from the left upper lobe. A scoring system was used to quantitatively evaluate the pulmonary involvement of all lesions, based on the involved location (17). The scoring criteria were typical chest CT findings for COVID-19 pneumonia (bilateral, multifocal rounded, and peripheral ground glass opacities and consolidations) (18). We analyzed the initial chest CT scans of the patients and scored the lung involvement based on two scoring methods of TLI and modified TLI.
For evaluating the TLI score, each of the six lung lobes was visually scored from 0 to 4: 0, no involvement; 1, 1 - 25% involvement (minimal); 2, 26 - 50% involvement (mild); 3, 51 - 75% involvement (moderate); and 4, ≥ 76% involvement (severe). The TLI score was the sum of each individual lobe score, ranging from 0 (no involvement) to 24 (maximum involvement) (16). Since lobar volume was not considered, we defined the modified TLI score to determine if it can increase the accuracy of prognostic prediction; the lobar involvement score was multiplied by five for the lower lobes, by three for the upper lobes, and by two for the middle lobe and lingula. The modified TLI score was the sum of values, ranging from 0 (no involvement) to 80 (maximum involvement).
To evaluate the demographic characteristics, we classified the patients into four groups: (1) group A, patients admitted to the wards, but not intubated or expired; (2) group B, patients admitted to the ICU, but not intubated or expired; (3) group C, patients intubated, but not expired; and (4) group D, patients who expired. Considering some overlaps between the groups, we also applied another classification. Moreover, the patients were classified into groups to compare the sensitivity and specificity of TLI and the modified TLI scoring methods: Patients with ICU admission or without ICU admission; patients intubated during hospitalization or not intubated; and dead or alive patients.
3.3. Statistical Analysis
Statistical analyses were performed using IBM SPSS for Windows Version 20 (IBM Corp., Armonk, NY, USA). Quantitative data are presented as mean ± standard deviation (minimum/maximum), and continuous data are presented as frequency and percentage. Chi-square (χ2) test was used for categorical variables. The TLI score as a function of time was quantitatively measured using the SPSS curve estimation module. Besides, quantitative data were compared using independent sample t-test or Mann-Whitney U test, according to their normal distribution. Kruskal-Wallis test was used for comparing the TLI and modified TLI scores in different patient groups. Moreover, a receiver operating characteristic (ROC) curve analysis was performed to determine the clinical value of TLI and modified TLI CT scores and to measure the cut-off values for predicting the prognosis of COVID-19. P-value < 0.05 was considered statistically significant in all analyses.
4. Results
4.1. Characteristics and Chest CT Findings of COVID-19 Patients
Of 207 patients, five were excluded due to pathological findings other than COVID-19 in their chest CT scans; also, one patient was excluded because of missing data. In total, 201 COVID-19 patients, aged between 13 and 97 years, were enrolled in this study. We categorized the patients into four independent groups: (1) group A, patients admitted to wards, but not intubated or expired (142 patients); (2) group B, patients admitted to ICU, but not intubated or expired (22 patients); (3) group C, patients intubated but not expired (13 patients); and (4) group D, patients who expired (24 patients) (Table 1).
| Variables | Values | P-value |
|---|---|---|
| Age (y) | 0.001 c | |
| Total (n = 201) | 55.4 ± 17.6 | |
| Group A (n = 142) | 54.8 ± 16.9 | |
| Group B (n = 22) | 55.3 ± 18.8 | |
| Group C (n = 13) | 38.3 ± 18.6 | |
| Group D (n = 24) | 67.8 ± 10.7 | |
| Gender (male/female) | 0.006 d | |
| Total (n = 201) | 125 (62.2)/76 (37.8) | |
| Group A (n = 142) | 79 (55.6)/63 (44.4) | |
| Group B (n = 22) | 15 (68.2)/7 (31.8) | |
| Group C (n = 13) | 13 (100)/0 (0) | |
| Group D (n = 24) | 18 (75)/6(25) | |
| Total lung involvement (TLI) score | < 0.001 e | |
| Group A (n = 142) | 8.99 ± 4.83 | |
| Group B (n = 22) | 9.40 ± 5.50 | |
| Group C (n = 13) | 12.53 ± 7.38 | |
| Group D (n = 24) | 16.08 ± 5.43 | |
| Modified total lung involvement (TLI) score | < 0.001 e | |
| Group A (n = 142) | 32.14 ± 16.60 | |
| Group B (n = 22) | 33.13 ± 18.23 | |
| Group C (n = 13) | 44.23 ± 24.53 | |
| Group D (n = 24) | 55.58 ± 18.32 |
a Group A, patients who were admitted to hospital wards, but not intubated or expired; Group B, patients who were admitted to ICUs, but not intubated or expired; Group C, patients who were intubated, but did not expire; Group D, patients who expired.
bValues are expressed as mean ± SD and No. (%).
c P-value is calculated by one-way ANOVA test.
d P-value is calculated by chi-square test.
e P-value is calculated by Kruskal-Wallis test.
The mean age of the patients was 54.8 ± 16.9 years in group A, 55.3 ± 18.8 years in group B, 38.3 ± 18.6 years in group C, and 67.8 ± 10.7 years in group D. The mean age of the patients was significantly different between the groups (P = 0.001) (Table 1). Among 201 patients, 125 (62.2%) were male, and 76 (37.8%) were female. In group A, 55.6% of the patients were male, and 44.4% were female. Among patients in group B, 68.2% were male, and 31.8% were female. In group C, all patients were male (100%), and in group D, 75 and 25% were male and female, respectively. The patient’s gender was significantly different between the groups (P = 0.006) (Table 1).
Moreover, we studied the lung involvement patterns in chest CT scans. Bilateral lung involvement was observed in 92% of the patients, and 84% of the patients showed a peripheral distribution of lesions. The patterns of lung involvement were mixed ground glass opacities and consolidations (75.6%), pure ground glass opacities (17%), and pure consolidations (7.4%). Other radiological findings included interlobular septal thickening (39.3%), crazy paving pattern (25.8%), halo sign (27.3%), and reverse halo sign (12.4%).
Based on the Kruskal-Wallis test, the mean TLI score was significantly different between the groups (P < 0.001) (Table 1). The mean TLI score was 8.99 in group A, 9.40 in group B, 12.53 in group C, and 16.08 in group D. The mean modified TLI scores of the groups are presented in Table 1. The degree of involvement of each lobe is presented in Table 2. Minimal involvement had the highest frequency among different lobes. The right lower lobe was the most frequently involved lobe and also the most severely involved one (Table 2).
| Lobar involvement | Number of involved lobes (percentage) based on the severity of involvement b | ||||
|---|---|---|---|---|---|
| No involvement | Minimal involvement | Mild involvement | Moderate involvement | Severe involvement | |
| Upper lobes | |||||
| Right upper lobe | 23 (11.4) | 89 (44.2) | 53 (26.3) | 22 (10.9) | 14 (7) |
| Left upper lobe | 30 (14.9) | 94 (46.7) | 43 (21.4) | 22 (10.9) | 12 (5.9) |
| Lower lobes | |||||
| Right lower lobe | 11 (5.4) | 60 (29.8) | 46 (22.8) | 46 (22.8) | 38 (18.9) |
| Left lower lobe | 19 (9.4) | 62 (30.8) | 56 (27.8) | 30 (14.9) | 34 (16.9) |
| Lingula | 43 (21.4) | 77 (38.3) | 39 (19.4) | 28 (13.9) | 14 (7) |
| Middle lobe | 37 (18.4) | 85 (42.3) | 47 (23.3) | 22 (10.9) | 10 (5) |
a Values are expressed as No. (%).
b Each lobe was visually scored from 0 to 4: 0, no involvement; 1, 1 - 25% involvement (minimal); 2, 26 - 50% involvement (mild); 3, 51 - 75% involvement (moderate); and 4, ≥ 76% involvement (severe).
Comparison of the number of involved lobes and the patients' prognoses showed that there was no significant difference among patients admitted to ICUs and patients admitted to the hospital wards (P = 0.06) (Table 3). However, intubated patients had a significantly higher number of involved lobes compared to non-intubated patients (P = 0.002) (Table 3). Patients who expired had the highest number of involved lobes (P = 0.001) (Table 3).
| Patient groups | Total number of involved lobes | Minimum - Maximum | P-value b |
|---|---|---|---|
| ICU admission | 0.067 | ||
| No (n = 146) | 5.08 ± 1.52 | 0 - 6 Lobes | |
| Yes (n = 55) | 5.47 ± 1.23 | 1 - 6 Lobes | |
| Intubation | 0.002 | ||
| No (n = 164) | 5.07 ± 1.51 | 0 - 6 Lobes | |
| Yes (n = 37) | 5.70 ± 1.05 | 1 - 6 Lobes | |
| Death | 0.001 | ||
| No (n = 177) | 5.08 ± 1.52 | 0 - 6 Lobes | |
| Yes (n = 24) | 5.95 ± 0.20 | 5 - 6 Lobes |
Abbreviation: ICU, intensive care unit.
a Values are expressed as mean ± SD unless otherwise indicated.
b P-value is calculated using Mann-Whitney U test.
We also compared the TLI and modified TLI scores in the paired groups, including patients with ICU admission (n = 55) versus patients without ICU admission (n = 146); patients intubated during hospitalization (n = 37) versus patients not intubated (n = 164); and patients who expired (n = 24) versus patients who survived (n = 177). The TLI and modified TLI scores were significantly higher in patients with ICU admission compared to patients without ICU admission (P = 0.002). Intubated patients in comparison with non-intubated patients and expired patients in comparison with alive patients had significantly higher TLI and modified TLI scores (P < 0.001) (Table 4).
| Patient groups | TLI score | Modified TLI score | P-value b, c |
|---|---|---|---|
| ICU admission | 0.002 | ||
| No (n = 146) | 9.24 ± 5.05 | 32.96 ± 17.30 | |
| Yes (n = 55) | 12.4 ± 6.45 | 43.45 ± 21.67 | |
| Intubation | < 0.001 | ||
| No (n = 164) | 9.048 ± 4.88 | 32.28 ± 16.77 | |
| Yes (n = 37) | 14.83 ± 6.32 | 51.59 ± 21.10 | |
| Death | < 0.001 | ||
| No (n = 177) | 9.30 ± 5.16 | 33.15 ± 17.65 | |
| Yes (n = 24) | 16.08 ± 5.43 | 55.58 ± 18.32 |
Abbreviation: ICU, intensive care unit; N, number of related patients.
aValues are expressed as mean ± SD.
b P-value is calculated based on the difference in the TLI score column.
c P-value is calculated using Mann-Whitney U test.
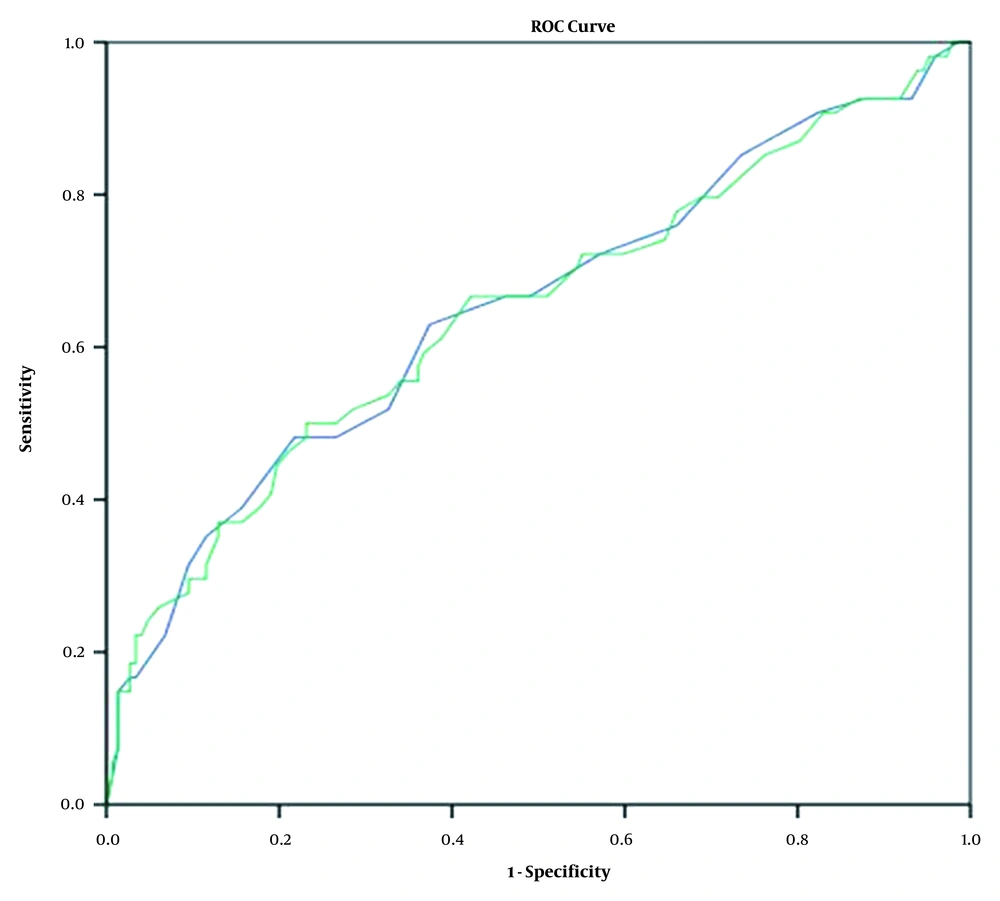
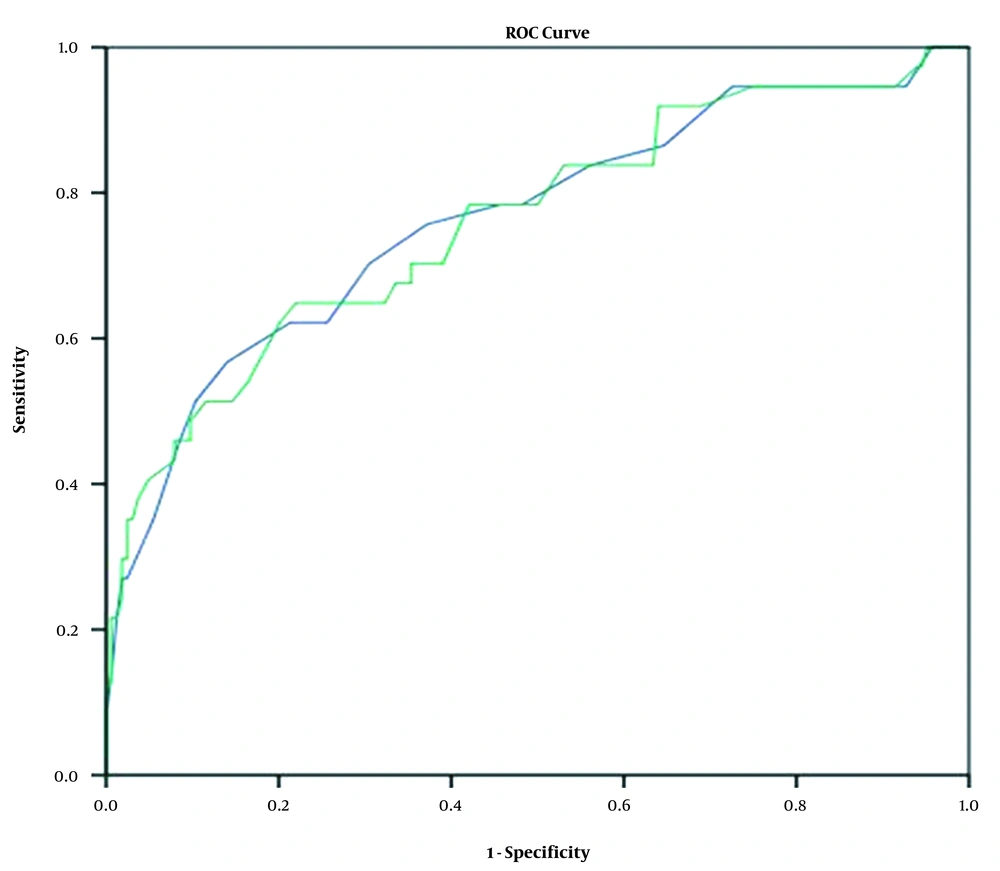
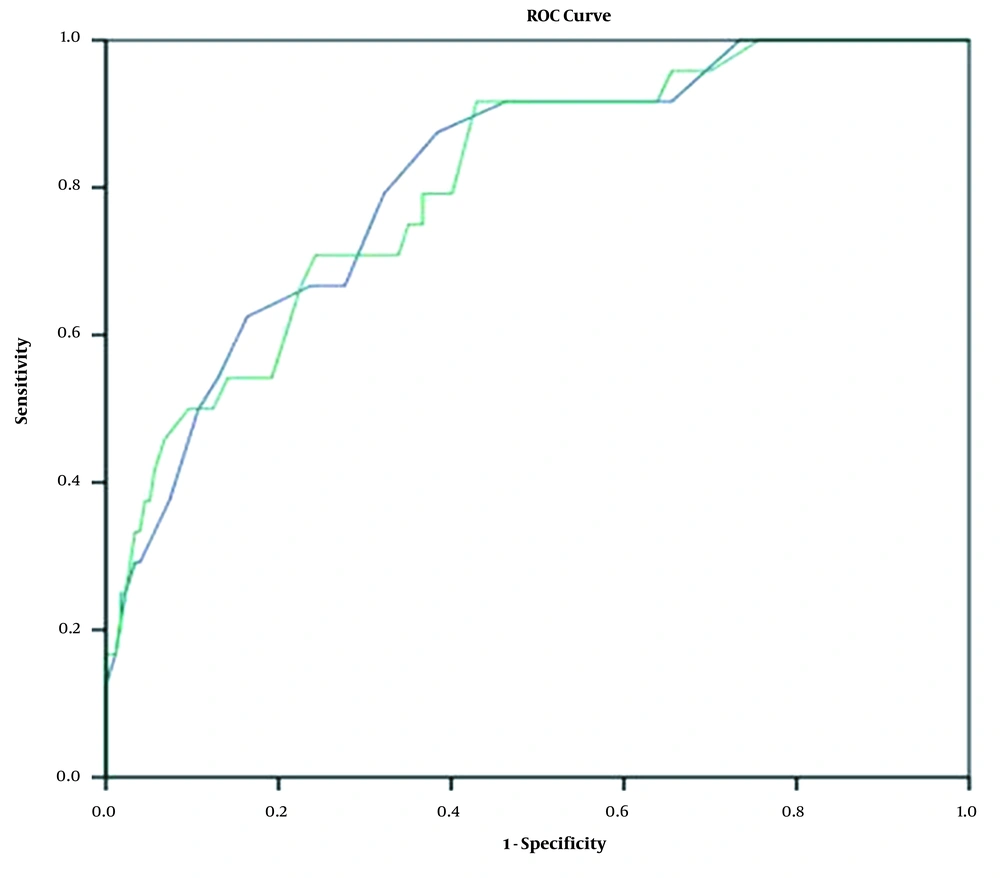
In the paired groups, there was no significant association between gender and mortality (P = 0.168), whereas the difference in the male-to-female ratio was significant between the ICU admission (P = 0.001) and intubation (P = 0.003) groups. Besides, the sensitivity and specificity of TLI and modified TLI scores for the prediction of ICU admission, intubation, and death were estimated using the ROC curve analysis and calculation of the area under the ROC curve (AUC) (Figures 1 - 3). The AUC showed no significant difference between the TLI and modified TLI scores in any of the groups (Figures 1 - 3).
Total lung involvement (TLI) and modified TLI scores in ICU-admitted COVID-19 patients (blue line: TLI score; green line: modified TLI score). The ROC analysis showed that the area under curve (AUC) was 65% (95% CI: 55 - 74%) for the TLI score and 64% (95% CI: 55 - 73%) for the modified TLI score.
Total lung involvement (TLI) and modified TLI scores for mortality in COVID-19 patients (blue line: TLI score; green line: modified TLI score). The ROC analysis showed that the area under curve (AUC) was 81% (95% CI: 72 - 90%) for the TLI score and 80% (95% CI: 71 - 89%) for the modified TLI score.
4.2. Diagnostic Ability of Chest CT Findings
The sensitivity and specificity of TLI scores in patients with ICU admission, intubation, and death prognosis are presented in Table 5. The AUC was 0.65 (95% CI: 0.55 - 0.74; P < 0.001) for patients admitted to the ICUs (Figure 1). The ROC curve analysis showed that the TLI score of 10.5 had 63% sensitivity and 63% specificity for ICU admission (P = 0.001) (Table 5). Also, the AUC for intubation was 0.76 (95% CI: 0.66 - 0.85; P < 0.001) (Figure 2). The TLI score for the prediction of intubation was 11.5, with 70.3% sensitivity and 70% specificity (P = 0.001) (Table 5). The TLI scores for the prediction of death in COVID-19 patients are presented in Figure 3. The AUC attributed to death was 0.81 (95% CI: 0.72 - 0.90; P < 0.001). The TLI score of 11.5 showed 79% sensitivity and 68% specificity, while the TLI score of 14.5 showed 62% sensitivity and 84% specificity. Also, the TLI score of 18.5 showed 96% specificity for the prediction of death in COVID-19 patients (P = 0.001) (Table 5).
| Prognosis | Measures | ||||
|---|---|---|---|---|---|
| AUC | 95% CI | TLI score | Sensitivity (%) | Specificity (%) | |
| ICU admission | 0.650 | 0.55 - 0.74 | 10.5 | 63 | 63 |
| Intubation | 0.763 | 0.66 - 0.85 | 11.5 | 70.3 | 70 |
| Death | 0.813 | 0.72 - 0.90 | 11.5 | 79 | 68 |
| 14.5 | 62 | 84 | |||
| 18.5 | 29 | 96 | |||
Abbreviations: AUC, area under the curve; CI, confidence interval (lower bound-upper bound); ICU, intensive care unit; TLI, total lung involvement.
a The test result variable (s) have at least one tie between the positive actual state group and the negative actual state group. Statistics may be biased.
5. Discussion
COVID-19 pneumonia has various prognoses in different patients. Patients with severe or critical COVID-19 have a poor prognosis and a higher mortality rate compared to normal COVID-19 patients (19, 20). Among different methods used for studying the clinical manifestations of COVID-19, chest CT imaging can be helpful in understanding COVID-19 and improving its clinical diagnosis and management.
Several clinical and laboratory prognostic factors have been suggested as the predisposing factors for COVID-19 pneumonia, including age and underlying medical conditions. Critical cases and patients with severe symptoms are normally older (> 55 years), and patients with an underlying disease (chronic pulmonary, cardiovascular, or cerebrovascular disease and diabetes) commonly have a worse prognosis (11, 14, 21). Sun et al. showed that depletion of lymphocytes and eosinophils and increased liver function tests, lactate dehydrogenase (LDH) level, albumin level, inflammatory markers (CRP), erythrocyte sedimentation rate (ESR), and ferritin are associated with COVID-19 severity (9). It has been also proposed that the elevated serum levels of NT-proBNP, IL-6, and procalcitonin were associated with the severity of COVID-19 (12, 13).
A recent study showed that the elevated ratio of WAL/normal pattern of the lung in CT scan was associated with a better prognosis of COVID-19. For instance, patients with a WAL percentage < 73% were more prone to disease progression, ICU admission, or death (15). The present study evaluated the prognostic significance of quantitative chest CT imaging for COVID-19 patients. The TLI score and a new scale (modified TLI) were evaluated and compared between different groups of patients. We found that there was no significant difference between the TLI and modified TLI scoring methods for COVID-19. Both scales showed approximately similar sensitivity and specificity for predicting the prognosis of ICU admission, intubation, and death (Figures 1 - 3).
There was no significant association between gender and mortality, while the difference in the ratio of men to women was significant in the ICU admission and intubation groups. Unlike previous studies (14, 22), male sex could be considered as a risk factor for ICU admission or intubation in COVID-19 patients, based on the present results. However, this finding may be attributed to the higher frequency of COVID-19 in males than females in Iran (23). Moreover, evaluation of the number of involved lobes and prognosis showed that the highest number of involved lobes was associated with a higher mortality rate. A similar study on prognostic prediction via chest CT scan found that the odds ratio of death prognosis was higher in patients with higher CT scores and more involved lobes (24).
We assessed the TLI and modified TLI scores to quantify lung involvement and evaluate its correlation with the prognosis of COVID-19. There was a significant difference in the TLI and modified TLI scores between different prognostic groups (P < 0.001). There was an overlap in the TLI and modified TLI scores in different groups. However, patients without ICU admission had significantly lower TLI and modified TLI scores compared to the other groups. We also measured the sensitivity and specificity of the scoring methods in the groups. At the TLI score of 11.5, with sensitivity and specificity of 70.3 and 70%, respectively (AUC = 76%; 95% CI: 66 - 85%), the patients were intubated.
Besides, the AUC for death was 81% (95% CI: 72 - 90%), and the TLI score of 11.5 showed 79% sensitivity and 68% specificity. The sensitivity and specificity were measured to be 62 and 84% for the TLI score of 14.5 and 29 and 96% for the TLI score of 18.5, respectively. Patients with intubation and patients who expired had higher TLI scores compared to patients who were only admitted to a ward or ICU without intubation. Our results are similar to the findings of a study by Li et al. (25), which found that the AUC of the total lung involvement score for diagnosing severe/critical COVID-19 was 0.918 (95% CI: 0.843 - 0.994).
Since COVID-19 has different clinical outcomes, and there are limited medical facilities for in-hospital management, application of a method for early prediction of prognosis can be helpful during the pandemic. Despite evaluating a large number of COVID-19 patients in the present study, this study had several limitations. First, we did not apply both qualitative and quantitative chest CT indicators to identify the CT characteristics of all cases. Second, we only analyzed the initial chest CT scans of patients; therefore, more follow-up imaging is suggested in future research. Third, we did not assess the correlation of clinical features and outcomes with chest CT scan features. Therefore, evaluation of both qualitative and quantitative chest CT findings, follow-up chest CT scan, and assessment of clinical symptoms and medical history are recommended in future cohort studies.
In conclusion, the severity of COVID-19 is associated with chest CT indicators, including TLI and the number of involved lobes. Patients with higher TLI scores in chest CT scan had a greater likelihood of severe disease, leading to intubation or death. The TLI scoring system seems to have a prognostic value in determining the need for ICU admission and vital healthcare planning in critical situations, such as the current COVID-19 pneumonia pandemic.