1. Background
The inferior alveolar nerve (IAN) block is the most common mandibular injection technique for achieving local anesthesia in restorative and surgical procedures. The mandible foramen (MF) is a key landmark in implant dentistry and is also of great importance for oral maxillofacial surgeons. Many studies have reported that cone-beam computed tomography (CBCT) is a more suitable modality for detecting different intra-oral nerves (1); however, it may cause some adverse effects due to ionizing X-rays (2, 3). Besides, CBCT image artifacts may not only decrease the image quality, but also reduce the probability of MF detection (4).
Ultrasonography (US), as a non-invasive method using non-ionizing ultrasound beams, seems to be a suitable option for intra-oral nerve and foramen imaging (5). Besides, US can be used to detect the location of neuronal fibers and increase the imaging accuracy during IAN block injection (5); therefore, it is more advantageous than other methods, such as CBCT. In this regard, Rama Mohan et al. (6) discussed the positive effects of using ultrasound beams on oral and maxillofacial surgeries. Also, Laher and Wells (7) recently investigated the location of MF in ultrasound images of black and Caucasian people. However, there is limited information about the detection of MF and its related landmarks using US.
Russa eand Fabian (8) examined the MF position in adult Tanzanian males. Sandhya et al. (9) also evaluated the location of MF and its related landmarks in East Indian mandibles. In another study, Movahhed et al. (10) examined the MF location relative to the occlusal plane using panoramic radiography. Besides, Rezaei et al. (11) investigated the three-dimensional position of the MF in west of Iran, using panoramic CBCT images. It should be noted that in some of these studies, US was not employed. Also, differences in the anatomical features of MF depending on age and sex are important in different patients (12-17).
2. Objectives
This study aimed to determine the MF location and examine its relationship with different landmarks.
3. Patients and Methods
This cross-sectional, analytical study was performed on patients, aged 19 - 28 years (Table 1), who were referred to the Radiology Department of the School of Dentistry, Isfahan University of Medical Sciences (Isfahan, Iran). Fifty patients, without facial trauma or mandible surgeries, were included in this study, and both sides of their mandible (left and right) were examined (Table 1).
| Sex | Males (n = 26, 52%) | Females (n = 24, 48%) |
|---|---|---|
| Age (mean ± SD/range), y | 25.2 ± 1.2/19 - 28 | 24.9 ± 1.1/19 - 28 |
| Facial trauma | 0 | 0 |
| Mandibular surgery | 0 | 0 |
The Demographic Characteristics of the Patients
Image acquisition was performed using an Alpinion US system (ECUBE7, Seoul, South Korea) with a 3 - 12 MHz linear oral transducer. Two maxillofacial radiologists with ten years of experience in US, monitored the patients. The US measurements were performed using a real-time method during examinations. Besides, the MF region was scanned in the horizontal and vertical planes by a transcutaneous approach. The MF was identified as a break on the continuity of the mandible. The horizontal and vertical diameters of the MF were measured by holding the probe both horizontally and vertically. The MF distance from the alveolar crest was also measured in the vertical plane from the upper limits of the alveolar bone. After capturing the best view of the MF, the image was frozen, and measurements were done with a caliper on the control panel.
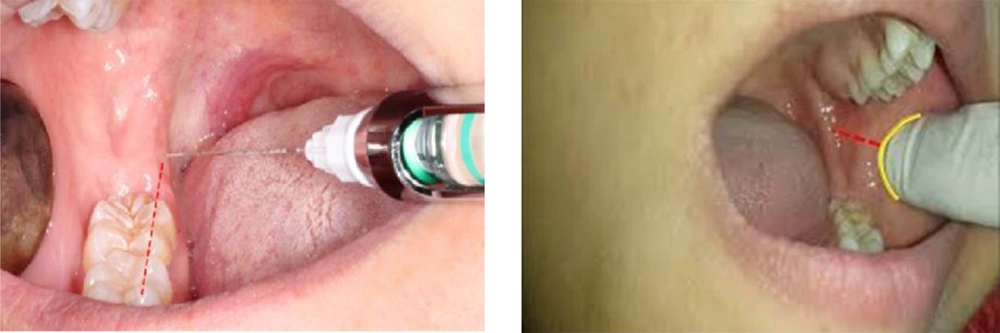
The MF location was determined according to the vertical and horizontal diameters. The MF vascularization was also examined using the Doppler US method. The deepest part of the pterygomandibular raphe (as a soft tissue landmark) was studied using the mentioned transducer. The Doppler method was applied for detecting MF. Moreover, the relationship between the MF and soft and hard tissue landmarks, including the anterior border of the ramus, mandibular occlusal plane, and pterygomandibular raphe, was evaluated using a calibrated ruler and a standard caliper. Figure 1 presents the anterior border of the ramus and also the occlusal plane.
3.1. Statistical Analysis
Mean values and standard deviations (SD) were measured and analyzed using paired samples t-test and independent t-test. These values were calculated in SPSS version 22 (Armonk, NY, USA).
4. Results
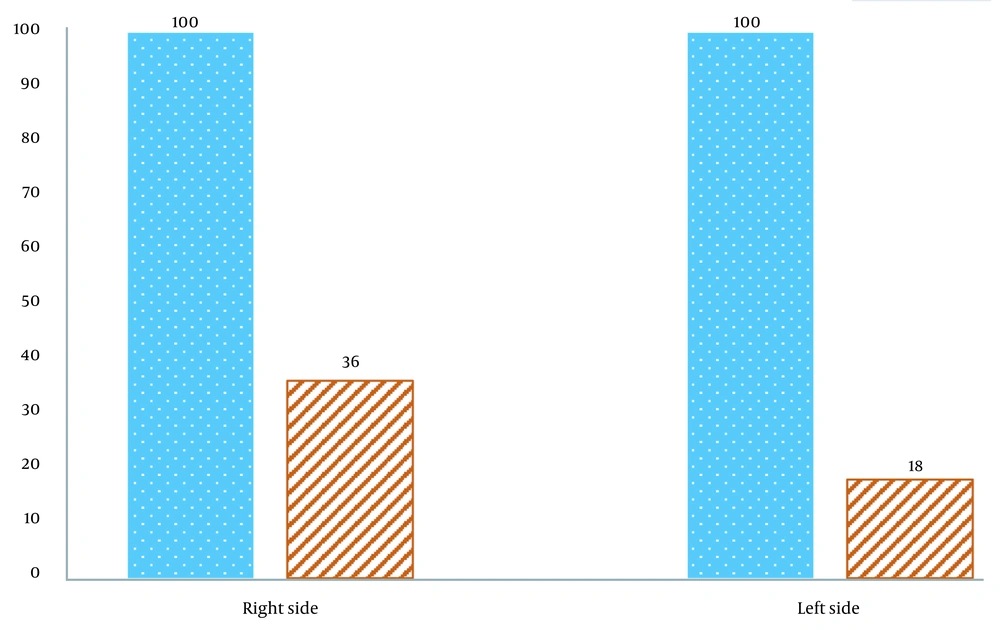
This study investigated the MF distance from its related soft and hard tissue landmarks using US. The age range of the studied patients was 19 - 28 years. Overall, 26 (52%) and 24 (48%) patients were male and female, respectively. In all patients, the MF was detected without any artifacts. Also, there was no similar MF in the ultrasound image of this area. Figure 2 presents the probability of identifying MF on the left and right sides using intra-oral US, with and without the Doppler method. The probability of detecting MF on the left and right sides was 18% and 36%, respectively. In this study, two MFs were detected on the right side. Besides, one MF was detected on the left side in males, while there were two MFs on the right side in females.
Table 2 indicates the mean (± SD) distance of the MF from the anterior border of the ramus on the left and right sides in males and females. Table 2 also presents the mean (± SD) vertical distance of the MF from the occlusal plane on the right and left sides in males and females. Based on the findings, the mean (± SD) distance of the MF from the studied landmarks in males was significantly longer than that of females (P < 0.001) (Table 2).
| Females (n = 24) | Males (n = 26) | P-value | |||
|---|---|---|---|---|---|
| Mean ± SD | Confidence interval (95%) | Mean ± SD | Confidence interval (95%) | ||
| The MF distance from the anterior border of the ramus | |||||
| Right | 13.3 ± 1.3 | Upper bound: 1.96; lower bound: 0.96 | 15.4 ± 1.9 | Upper bound: 1.96; lower bound: 0.97 | < 0.001 |
| Left | 14.6 ± 1.01 | Upper bound: 1.96; lower bound: 0.93 | 17.4 ± 1.8 | Upper bound: 1.96; lower bound: 0.94 | < 0.001 |
| The MF vertical distance from the occlusal plane | |||||
| Right | 6.9 ± 0.8 | Upper bound: 1.96; lower bound: 0.96 | 8 ± 1.1 | Upper bound: 1.96; lower bound: 0.93 | < 0.001 |
| Left | 7.9 ± 0.8 | Upper bound: 1.96; lower bound: 0.95 | 9.3 ± 1.1 | Upper bound: 1.96; lower bound: 0.96 | < 0.001 |
The Mandibular Foramina (MF) Distance from the Anterior Border of the Ramus and the Occlusal Plane of the Mandible
The mean (± SD) distance of the MF from the anterior border of the ramus on the right and left sides was 15.4 ± 1.9 and 17.4 ± 1.8 mm in males, respectively, whereas it was 13.3 ± 1.3 and 14.6 ± 1.01 mm in females, respectively. According to the findings, the mean (± SD) distance of the MF from the vertical occlusal plane on the right and left sides was 8 ± 1.1 and 9.3 ± 1.1 mm in males and 6.9 ± 0.8 and 7.9 ± 0.8 mm in females, respectively. The MF was located in the deepest part of the vertical plane from the pterygomandibular raphe.
5. Discussion
This study was performed to evaluate the MF location relative to the adjacent soft tissue landmarks using intra-oral US. According to our findings, the Doppler method may increase the probability of MF detection as compared to the conventional US method. In US, the mandibular ramus, internal pterygoid, and masseter muscles were detected in gray color with a bright background. The ramous border looked white due to the high absorption coefficient of the bone. Using the Doppler method, the arteries looked bright red, and the pulse of IAN was also detected. The IAN was located anteriorly to the inferior alveolar artery (IAA) and could help detect the area of this artery. In this study, the IAA and IAN location was also detected precisely, because there was no similar artery in the pterygomandibular space (4).
Based on the present findings, the MF is located on the posterior border of the ramus and the deepest part of the pterygomandibular raphe. The mean (± SD) distance of the MF from the anterior border of the ramus on the left side was significantly longer than the right side (P < 0.001). Moreover, the mean (± SD) vertical distance of the MF from the occlusal plane on the left side was significantly higher than the right side (P < 0.001). Also, the mean (± SD) distance of the MF from the anterior border of the ramus and the occlusal plane was significantly longer in males than in females (P < 0.001); however, there was no significant difference in the age of the patients (P > 0.05).
Rezaei et al. (11) reported that there was no significant difference in the MF distance from the anterior and posterior borders of the ramus between the right and left sides (P > 0.05). Besides, the vertical distance was significantly longer in males than in females (P < 0.05). The measured distances did not have a significant correlation with the age of the patients (P > 0.05) (1), which is in line with our findings. In another study, similar to our findings, Ennes and Medeiros (18) found that there was no significant difference in the MF location between the right and left sides.
Additionally, Sandhya et al. (9) evaluated the location of the MF and its relative landmarks in East Indian mandibles and concluded that the MF distance from the anterior border of the ramus was 16.27 and 16 mm on the left and right sides, respectively. However, there was no significant difference between the two sides (9), which is inconsistent with our results; this might be due to the different features of the studied populations. Moreover, Pynn et al. (19) examined mandibular anesthesia landmarks in Canadian aboriginals and the Caucasians and reported that variations in the MF distance from the anterior border of the ramus were largely related to racial differences.
Thangavelu et al. (20) investigated the MF position relative to various anatomical landmarks of dry adult mandibles and concluded that there was no significant difference in the MF distance from the anterior border of the ramus between the left and right sides. Also, failure in achieving anesthesia for the IAN is highly dependent on the operator, and anatomical variations are not considerable (20). Moreover, in our study, there was some small differences in the measured distances between males and females. Besides, there was a significant difference in the MF distance from the anterior border of the ramus and also the occlusal plane between males and females, whereas the difference was not significant according to a study by Laher and Wells (7). It should be noted that this study was performed on a live population, unlike some previous studies which were performed on dry mandibles.
According to the results of the present study, intra-oral US is a suitable non-invasive modality, which can detect the MF distance from related landmarks accurately; therefore, it can be a suitable option for mandibular injection and achieving local anesthesia. Based on our results, US is a safe and reliable modality for detecting the MF and its related landmarks due to the use of non-ionizing beams, besides adequate image quality.