1. Background
Osteoporotic compression fractures are common complications of osteoporosis, which have become increasingly prevalent in the elderly (1). According to the Thoracolumbar Injury classification and severity score (TLICS) proposed by Vaccaro et al. (2), a compression fracture can be classified as the most stable type of fracture, depending on the fracture morphology. In clinical practice, a posterior ligamentous complex (PLC) injury can be found in an osteoporotic compression fracture. If the compression fracture is accompanied by a PLC injury, the TLICS score will be four, and the orthopedist will recommend a surgical intervention.
In this regard, previous studies (3, 4) have shown that a disc injury is closely related to vertebral instability and can lead to progressive kyphosis and a poor prognosis; therefore, assessment of the PLC and disc is essential. Magnetic resonance imaging (MRI) is mainly used to evaluate the PLC and disc status in fractures that are not associated with neurological deficits or canal invasion. However, in emergency situations, when the patient has multiple traumas, MRI is not the first-line examination due to its limited availability and contraindications. If computed tomography (CT) scan parameters are applied to predict PLC and disc injuries, it is possible to save medical resources and improve the patients’ compliance.
The loss of vertebral body height (LOVBH) plays a critical role in the assessment of the severity of compression fractures. Many previous studies (5-7) have reported that LOVBH is not associated with PLC or disc injuries. However, it should be noted that these studies either excluded osteoporotic fractures (7, 8) or confused them with non-osteoporotic fractures (5, 9) when investigating the relationship between LOVBH and PLC injuries. The bone mass of different vertebrae varies, especially between osteoporotic and non-osteoporotic vertebrae. This variation may be neglected if only LOVBH is considered, because two vertebral bodies with the same LOVBH are generally subjected to different impact forces due to differences in solidity. Previous studies (10, 11) have confirmed that the vertebral body CT value is useful for assessing the bone mineral density and diagnosing osteoporosis with high consistency.
2. Objectives
In this study, it was hypothesized that the CT compression ratio (CTCR), namely, the CT value ratio of the injured vertebra to the adjacent vertebra, could represent the impact forces of the injured vertebra in thoracolumbar compression fractures and exclude differences in the solidity of different vertebrae. This study aimed to determine the role of CTCR in the diagnosis of disc and PLC injuries and to compare it with LOVBH in osteoporotic thoracolumbar compression fractures.
3. Patients and Methods
This single-center, retrospective study was approved by the medical ethics committee and the institutional review board of our hospital (code: [2017] 121501). It was performed on consecutive patients, aged 40 - 90 years, presenting to our hospital for a new single osteoporotic vertebral compression fracture, without a neurological deficit, during 2018 - 2020. Osteoporosis was diagnosed when the lowest T score was ≤ 2.5 standard deviations (SDs) on dual X-ray absorptiometry. Complete examinations, especially CT and MRI, were necessary, and the fractured vertebral body was located in the thoracolumbar spine (T11-L2).
The exclusion criteria were as follows: (1) pathological fractures, such as vertebral metastasis and spinal infection; (2) fractured vertebrae with dislocation or rotation; (3) a history of spinal surgery or postoperative vertebral fractures; (4) a negative CT value of the vertebral body for severe vertebral fat degeneration; and (5) an inaccurate CT value due to the separation of vertebral body fragments, such as burst fractures. The CT and MRI characteristics of the compression fracture, as well as demographic information, including age, gender, injured segment, and cause of fracture, were recorded.
3.1. CT Scan of Suspected Signs
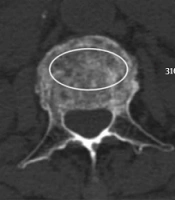
The CTCR was measured in the axial view of CT images and calculated by dividing the injured vertebra CT value by the average CT value of the cephalad and caudal uninvolved vertebrae. The measurement of the vertebral body CT value was based on the methods proposed by Pickhardt et al. (12) by drawing a single click-and-drag ROI in the anterior trabecular bone space while avoiding the cortical bone, hyperosteogeny, and the intravertebral venous plexus at the level of pedicles in axial images (Figure 1). To measure the final CT value, the average values of the first measurement (L.D.) and the second measurement (Z.D.) were calculated.
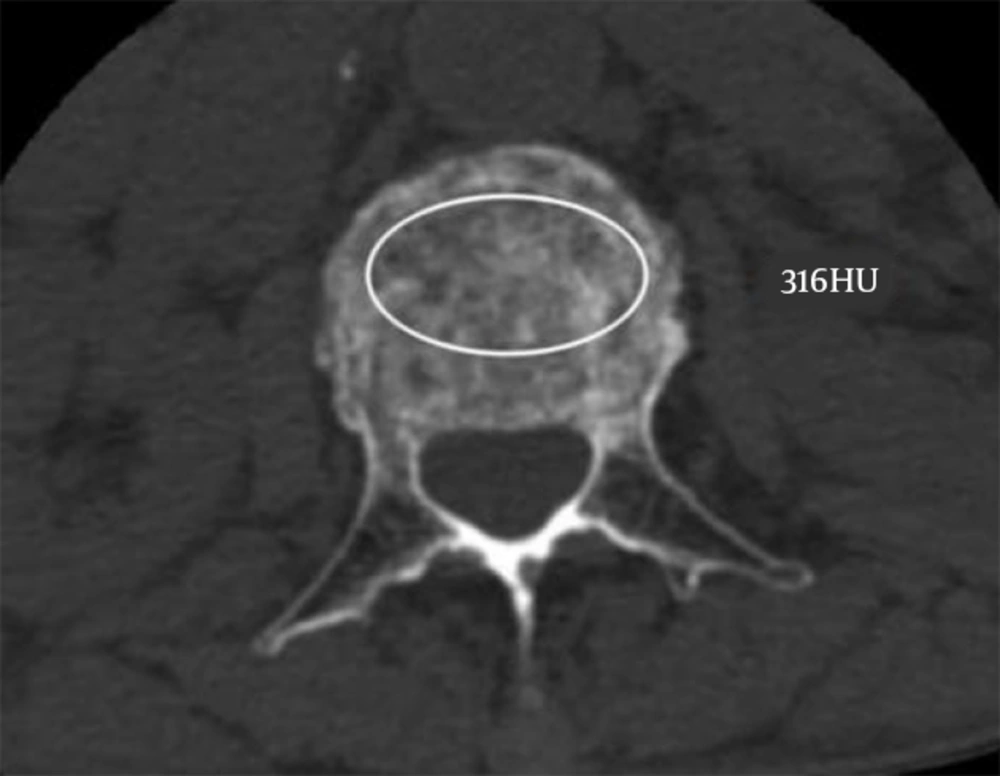
Parameters, including LOVBH, local kyphosis (LK), interspinous widening (ISW), vertebral translation (VBT), and posterior structure fracture (PSF), were measured in the mid-sagittal view of CT images. The LOVBH was defined as Ha/Hp or Hm/Hp ratio, where Ha represents the anterior height of the injured vertebra, and Hp represents the posterior height of the injured vertebra. If the whole vertebral body is compressed, Hp refers to the posterior height of the cephalad vertebra, and Hm represents the middle height of the injured vertebra, as described in previous studies (5, 13) (Figure 2).
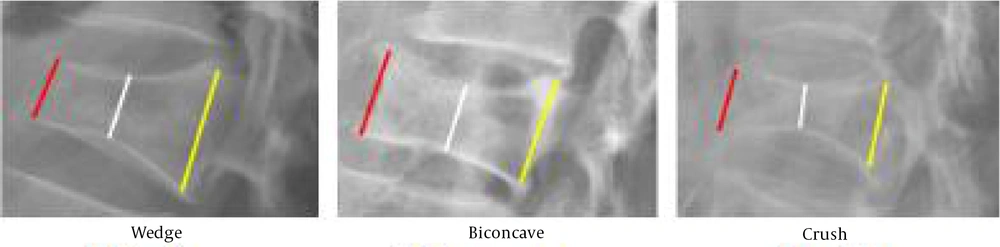
Moreover, LK is the angle between the lines drawn along the superior and inferior endplates of the fractured vertebral body. Besides, ISW is defined as the relative widening of the midpoint interspace of the spinous process above the injured vertebra compared to the subjacent interspinous distance. VBT is defined as relative displacement of the injured vertebra in the sagittal or coronal plane (Figure 3). Finally, PSF is considered if a pedicle, lamina, or spinous process fracture is observed.
A, Interspinous widening (ISW) (white line); B, Local kyphosis (LK); C, Vertebral translation (VBT) (arrow); D, The same case presented in Figure 3C. The VBT is not obvious in the coronal view (arrow).
3.2. MRI Evaluation of Disc and PLC Injuries
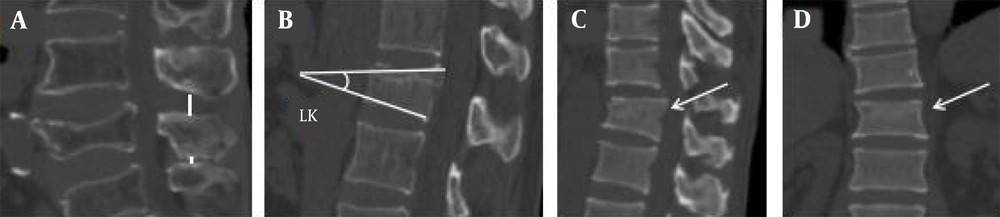
The injured vertebral segment was examined via MRI in all patients within three days after admission. According to the methods proposed by Haba et al. (14) as a reference, a PLC injury was considered when the black stripe, representing the supraspinous ligament (SSL) on sagittal images, disappeared or appeared discontinuous (Figure 4), and/or when the interspinous space showed high signal intensity on sagittal T2-weighted (T2W)/T2W-short tau inversion recovery (STIR) images, representing an interspinous ligament (ISL) rupture.
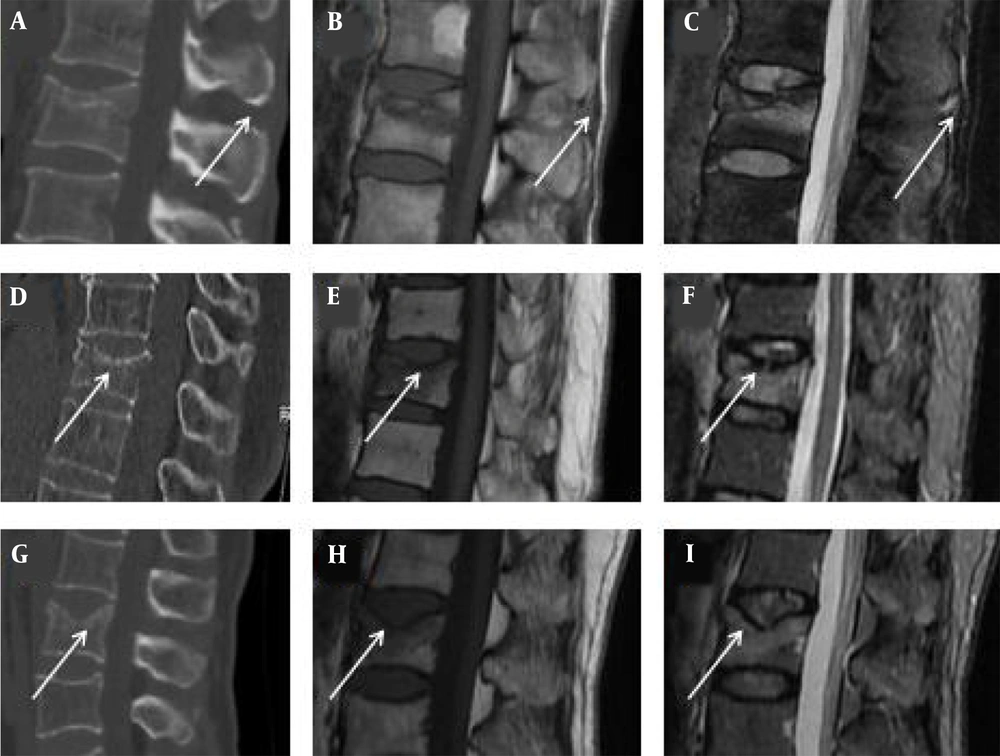
CT scans (A, D & G), T1WI MRI (B, E & H), and T2-short tau inversion recovery (STIR) MRI (C, F & I) images. A-C, A posterior ligamentous complex (PLC) injury is shown with a high signal intensity (HSI) of the interspinous space on T2W-STIR image and isointensity on T1WI (white arrows). D-F, Disc injury (grade 2) is shown as discontinuous HSI inside the disc on T2W-STIR image and isointensity on T1WI (white arrows). G-I, Disc injury (grade 3) is shown as disc rupture and infraction into the vertebral body on the T2W-STIR image and T1WI (white arrows). These manifestations cannot be seen on the CT scans (A, D & G).
In this study, disc injuries were classified into three grades, as described by Sander et al. (4). Grade 0 suggests no morphological or signal difference between the injured disc and a comparable uninjured disc. Grade 1 is defined as relatively well distributed hyperintense signals on T2W/T2W-STIR images, representing disc edema. Grade 2 is defined as a disc rupture with discontinuous perifocal hyperintense signals on T2W/T2W-STIR images and iso/hyperintense signals on T1W images, suggesting intradiscal bleeding. Compared to grade 2, the criteria for grade 3 injuries are based on the additional features of disc infraction into the vertebral body, annular tear, or herniation into the endplate. Overall, grade 0 and grade 1 injuries suggest disc integrity, while grade 2 and 3 suggest disc injuries (Figure 4). A disc located in the upper or lower parts of the fractured vertebra was injured.
All measurements were performed independently on a Picture Archiving and Communication System (PACS, Senyint, China) by two experienced radiologists (L.D. and Z.D.), who were blinded to the patients’ medical records and the initial imaging diagnoses. If there were any differences in the interpretation of images, consensus was achieved through discussion. CT scans were performed on a 64-slice spiral scanner with a slice thickness of 1.4 mm, a tube voltage of 120 kV, and a tube current of 200 mA. MRI was performed on a 3.0 T machine.
3.3. Reproducibility
Twenty patients were randomly selected to examine intra- and inter-reader reproducibility by calculating the CTCR of the fractured vertebrae. To assess the inter-reader reproducibility, two reviewers (D.L. and D.Zh) calculated the CTCR of the fractured vertebrae independently. Also, to examine intra-reader reproducibility, one reviewer (D.L.) calculated the CTCR of the fractured vertebrae twice in a time interval of one month to minimize memory bias.
3.4. Statistical Analysis
The CTCR and LOVBH were analyzed to determine the relationship of PLC and disc injuries. Other CT findings, including LK, ISW, VBT, and PSF, were also analyzed to determine significant variables for further analysis. Independent samples t test, Mann-Whitney U test, or chi-square test was applied as appropriate. The odds ratio (OR) and 95% confidence intervals (CI) of CTCR and LOVBH were also calculated for discriminating PLC and disc injuries, based on a logistic regression analysis before and after controlling for the confounders. Next, a receiver operating characteristic (ROC) curve was used to calculate the area under the curve (AUC), representing the predictive value of CTCR and LOVBH in PLC or disc injuries, and to find the best threshold. All statistical analyses were performed in SPSS Version 24.0 for Windows (IBM Inc., Chicago, IL, USA), and P-value less than 0.05 was considered statistically significant.
4. Results
4.1. Characteristics of the Study Population
A total of 112 patients met the inclusion criteria. Twenty-one patients with incomplete medical records or poor image quality were excluded, and finally, 91 patients, with the mean age of 62.12 ± 9.16 years (range, 48 - 87 years), were recruited as the study population. Overall, there were 39 (42.8%) male and 52 (57.2%) female participants. The demographic and injury characteristics of the participants are presented in Table 1. There were 9 (9.8%) patients in the PLC injury group, and 82 (90.1%) patients in the intact PLC group. The disc injury and intact groups included 47 (51.6%) and 44 (48.3%) patients, respectively. No PSF was found in the study population. The causes of injury included traffic accidents, crush injuries, high falls, and others. The number of fractures at each level was as follows: 11 fractures at T11, 35 fractures at T12, 29 fractures at L1, and 16 fractures at L2.
| Demographics | Values |
|---|---|
| Gender | |
| Female | 52 |
| Male | 39 |
| Mean age | 62.12 |
| Fractured level | |
| T11 | 11 |
| T12 | 35 |
| L1 | 29 |
| L2 | 16 |
| Status of PLC/disc | |
| PLC | Injured: 9, intact: 82 |
| Disc | Injured: 47, intact: 44 |
| Causes | |
| Traffic accidents | 7 |
| Crush injuries | 29 |
| High falls | 24 |
| Others | 31 |
Abbreviation: PLC, posterior ligamentous complex .
4.2. CTCR and LOVBH in Diagnosis of PLC/disc Injuries
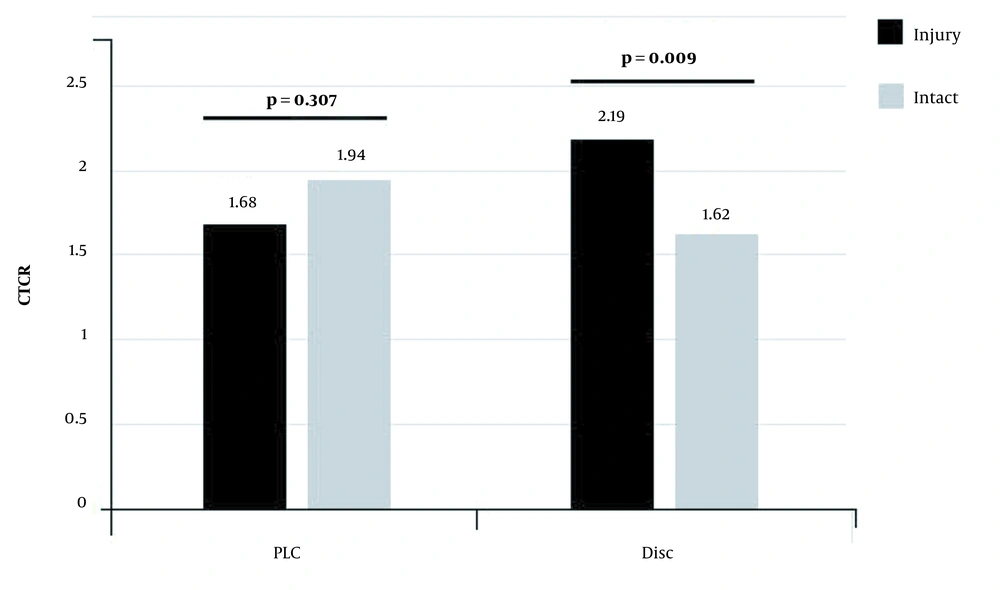
In the first-round analysis, 91 patients were divided into the PLC injury and intact groups. Based on the findings, the CTCR, Ha/Hp, and Hm/Hp were not significantly associated with PLC injuries (CTCR: 1.68 ± 1.02 vs. 1.94 ± 0.71, P = 0.307; Ha/Hp: 0.67 ± 0.09 vs. 0.67 ± 0.10, P = 0.667; and Hm/Hp: 0.62 ± 0.08 vs. 0.58 ± 0.09, P = 0.536). Regarding other CT findings, only VBT was significantly related to PLC injuries (22.2% vs. 2.4%, P = 0.006).
Moreover, in the second-round analysis, 91 patients were divided into disc injury and intact groups. The mean CTCR was significantly higher in the disc injury group compared to the disc intact group (2.19 ± 0.80 vs. 1.62 ± 0.54, P = 0.009) (Figure 5), while comparison of Ha/Hp and Hm/Hp showed no significant differences between the groups (Ha/Hp: 0.63 ± 0.10 vs. 0.71 ± 0.08, P = 0.250; Hm/Hp: 0.52 ± 0.06 vs. 0.66 ± 0.06, P = 0.577). On the other hand, VBT was significantly associated with disc injuries (8.5% vs. 0%, P = 0.048), as summarized in Table 2.
| PLC injury | Disc injury | |||||
|---|---|---|---|---|---|---|
| PLC injury group (n = 9) | PLC intact group (n = 82) | P-value | Disc injury group (n = 47) | Disc intact group (n=44) | P-value | |
| CTCR | 1.68 ± 1.02 | 1.94 ± 0.71 | 0.307 | 2.19 ± 0.80 | 1.62 ± 0.54 | 0.009 |
| Ha/Hp ratio | 0.67 ± 0.09 | 0.67 ± 0.10 | 0.667 | 0.62 ± 0.10 | 0.71 ± 0.08 | 0.250 |
| Hm/Hp ratio | 0.62 ± 0.08 | 0.58 ± 0.09 | 0.536 | 0.52 ± 0.06 | 0.66 ± 0.06 | 0.577 |
| LK (°) | 14.78 ± 1.79 | 15.35 ± 2.16 | 0.422 | 15.32 ± 2.21 | 15.27 ± 2.06 | 0.981 |
| ISW | 2 (22.2) | 14 (17.1) | 0.700 | 10 (21.3) | 6 (13.6) | 0.339 |
| VBT | 2 (22.2) | 2 (2.4) | 0.006 | 4 (8.5) | 0 (0) | 0.048 |
| PSF | 0 | 0 | - | 0 | 0 | - |
Abbreviations: CTCR, CT compression ratio; LOVBH, loss of the vertebral body height; LK, local kyphosis; ISW, interspinous widening; VBT, vertebral translation; PSF, posterior structure fracture; PLC, posterior ligamentous complex.
aThe data are presented as mean ± standard deviation or No.(%)
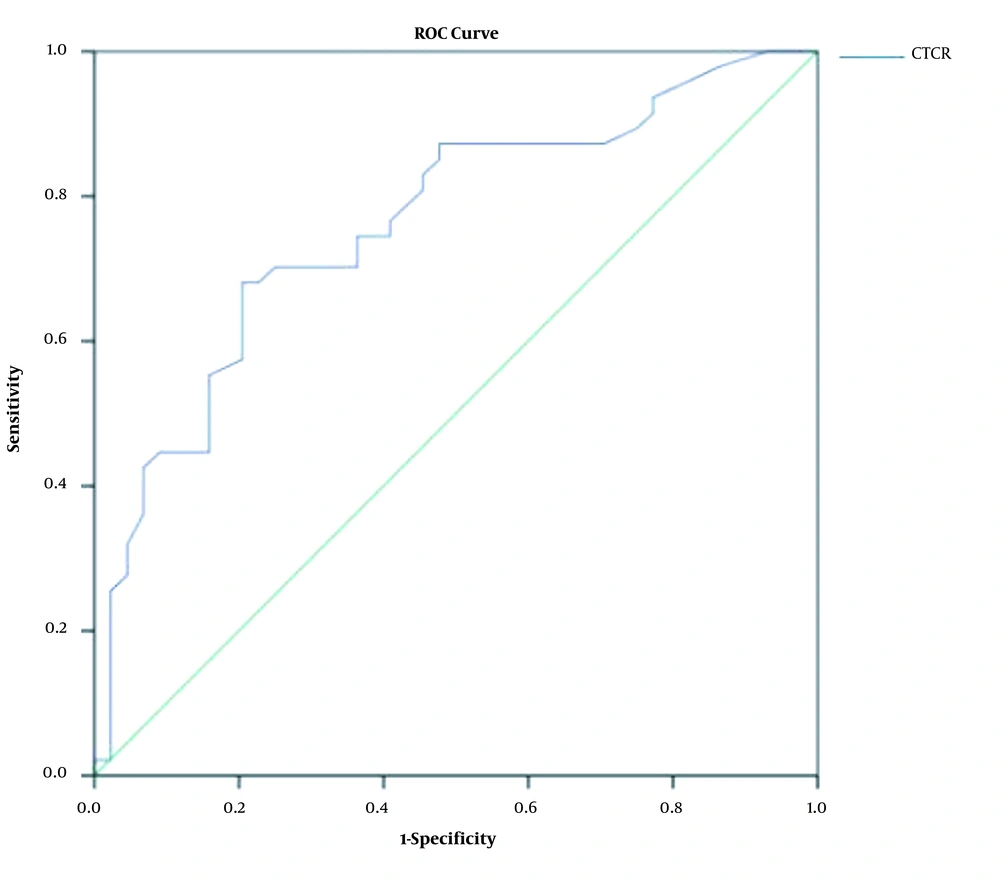
The univariate logistic regression analysis revealed that CTCR was significantly associated with disc injuries (OR, 4.884; 95% CI: 1.872 - 12.742; P = 0.001). The correlation was still significant after controlling for VBT in the multivariate logistic regression analysis (OR, 5.242; 95% CI: 1.945 - 14.133; P = 0.001). The ROC curve analysis (Figure 6) showed that the AUC of CTCR was 0.762 (95% CI: 0.663 - 0.860, P < 0.001). The most appropriate threshold was 1.755, with sensitivity of 68.1% and specificity of 79.5%.
4.3. Reproducibility
The intra-reader and inter-reader agreement of CTCR measurements for the fractured vertebrae were acceptable on CT images (ICC = 0.795, P < 0.001 and ICC = 0.770, P < 0.001, respectively).
5. Discussion
The PLC injuries can influence the clinical decision to perform surgical procedures. Previous studies (15, 16) have shown that biomechanical stress on the PLC can stabilize the spine. Therefore, PLC injuries should be considered in the treatment of thoracolumbar fractures, as they can affect the postoperative spinal stability. Similar to the PLC, the disc also plays a crucial role in posttraumatic stability and healing capability. With the growing awareness of the importance of the PLC and disc, evaluation of these injuries seems critical.
Osteoporotic compression fractures are relatively stable fractures based on the TLICS. According to previous studies (7, 17), the incidence of PLC injuries is relatively low in neurologically intact thoracolumbar fractures. In the present study, only 9.9% (9/91) of the PLC injuries were found in osteoporotic compression fractures. Disc injuries were more common, with an incidence of approximately 56% (18) in patients with a single thoracolumbar vertebral fracture; the corresponding rate was 51.6% (47/91) in the present study. Consistent with previous studies, our findings confirmed that compression fractures are less likely to be accompanied by a posterior structure damage. Nevertheless, damage to the intervertebral disc is common, because the disc is located between two vertebral bodies and is easily involved.
Many studies have calculated the vertebral height loss by directly measuring the vertebral height. Hong et al. (13) recommended the Ha/Hp ratio measurement as the first-line technique with the highest reliability. However, when the fractured vertebra shows depressed upper margins, the Ha/Hp ratio is inaccurate, and the Hm/Hp ratio (19) seems more accurate. The vertebrae of different individuals, especially the osteoporotic vertebrae of the elderly, often show different degrees of fat infiltration, resulting in differences in solidity. Therefore, when a compression fracture occurs, the impact forces on the vertebral bodies differ, even if the height loss is similar. Previous studies (10, 11) have shown that the vertebral body CT value is a valid index for assessing the bone mineral density and diagnosing osteoporosis. In the present study, only CTCR was related to disc injury, which indicates the importance of heterogeneity of bone solidity in different patients.
In this study, the PLC injuries were not associated with the degree of vertebral compression, regardless of the evaluation method. Jiang et al. (5) and Rajasekaran et al. (6) reported that the loss of anterior or posterior height was not a predictor of PLC injuries, which is consistent with the present results. Our findings strengthen the evidence that osteoporotic compression fractures are relatively stable with less PLC injury. A recent study (9) revealed that only a vertebral body translation > 3.5 mm was related to a PLC injuries. In this study, VBT was also associated with the PLC injuries, suggesting that these injuries are more closely related to vertebral translation rather than vertebral compression.
There are several limitations to this study. First, the PLC injuries were only observed in MRI images and were not confirmed by surgical procedures. Second, no PSF was found in our study population; therefore, a larger study population is warranted to reveal the role of PSF. Third, the standard diagnosis of PLC injuries varies based on MRI; therefore, unified diagnostic criteria need to be established in future studies.
In conclusion, the CTCR of the injured vertebral body is significantly associated with disc injuries rather than PLC injuries in patients with osteoporotic thoracolumbar compression fractures, suggesting that compression fractures are relatively stable with less PLC injury. Overall, the CTCR is a useful indicator of compression degree and a valid predictor of disc injuries.