1. Background
Acute appendicitis is a common gastrointestinal emergency in children and adolescents, which affects approximately 5.7 - 57 per 100,000 people annually (1). The incidence rate of acute appendicitis is dependent on gender, ethnicity, age, and obesity (2, 3). The appendix removal is the gold standard treatment, because there is a possibility of the appendix rupture (4). Diagnosis of appendicitis is commonly based on the patient’s medical history, physical examination of the pelvic region, psoas sign, guarding, obturator sign, digital rectal examination, and rebound tenderness (4). Apart from general clinical examinations and symptom analysis, the primary imaging methods include pelvic ultrasonography (US), computed tomography (CT) scan, X-ray, and magnetic resonance imaging (MRI).
The US examination is a portable, non-irradiating, and cost-effective method that can be carried out rapidly. Therefore, it is considered as an ideal non-invasive method for acute appendicitis, which is especially safe for the elderly, children, and pregnant women (5). This examination is widely used for the diagnosis of acute appendicitis (6). However, many factors, such as the small diameter and length of the appendix, anatomical position, coverage by the intestines, bowel discomfort, and flatulence, may affect the visualization of the appendix (5). Therefore, the diagnostic accuracy of US is highly dependent on the practitioner’s skills (7). The excellent accuracy of non-enhanced CT scan was reported for appendicitis (93%), with higher sensitivity and specificity for the diagnosis of acute appendicitis (8). Besides, a similar performance has been reported for MRI and CT scan in detecting acute appendicitis (9).
2. Objectives
The present study aimed to compare US, CT, and diffusion-weighted MRI (DW-MRI) examinations for the diagnosis of acute appendicitis with the rate of proven appendicitis after surgery. Besides, the patients’ demographic characteristics were investigated in relation to the diagnosis of appendicitis.
3. Patients and Methods
This retrospective study was performed on 70 patients diagnosed with acute appendicitis between February 2018 and January 2020. The inclusion criteria were as follows: diffuse lower abdominal pain; positive clinical and laboratory findings for appendicitis; the right lower quadrant pain; and lack of major contraindications for MRI, such as implanted devices or claustrophobia. On the other hand, pregnant patients were excluded from the study. The US, NECT, and DW-MRI examinations were performed for all patients included in the study.
3.1. Patient Preparation and Surgery
All patients, who were identified as positive for acute appendicitis by DW-MRI, underwent surgery for acute appendicitis. This procedure was performed using a 1.5-Tesla MRI unit, with b-values of 0, 400, and 800 s/mm2.
3.2. Imaging Protocol
The emergency department physicians defined the patient’s imaging management at presentation (i.e., use of NECT). Most of the patients were allowed to undergo detailed imaging after their complaints of pain and primary clinical examinations. DW-MRI was performed using a 1.5-T MRI unit (Signa HDe, GE Healthcare, Waukesha, WI, USA). Imaging was carried out in the supine position with an eight-channel phased-array coil. An axial DW single-shot echo-planar imaging (ssEPI) sequence, with fat suppression but without breath holding, was performed. A three-plane gradient echo sequence was also used as a localizer sequence at the onset of examinations.
Among MRI sequences, T2-weighted (T2W) and short tau inversion recovery (STIR)/turbo inversion recovery magnitude (TIRM) sequences were used to guide DW-MRI. The STIR/TIRM sequences were used to visualize the appendix segments; to detect the accompanying inflammatory fluid; and to identify other possible pelvic anomalies in all examinations, especially those with retrocecal localization. The T2W sequences were used in a multiplanar mode for optimal diameter measurements. The diameter measurements were recorded for each patient by calculating the thickest segment after the radix of the tubule appendix from the outer diameters on the short axis in an appropriate plane.
3.3. T2W Imaging
Before DW-MRI, the patients underwent an axial free-breathing, fat-saturated sequence and a coronal turbo spin-echo (TSE) T2W imaging. The scanning parameters were as follows: repetition time (TR)/echo time (TE): 5030/105 ms; section thickness: 5 mm; intersection gap: 35%; matrix size: 192 × 192; number of excitations (NEX): 4; field of view (FOV): 450 × 450 mm; and acquisition time: ~3 min.
3.4. DW-MRI
The imaging parameters for DW-MRI were as follows: TR/TE: 5500/100 ms; section thickness: 5 mm; intersection gap: 30%; matrix size: 128 × 128; NEX: 4; FOV: 400 × 400 mm; acquisition time: ~4 min; parallel imaging with a reduction factor of two; and water excitations with b-values of 0, 400, and 800 s/mm2. No MRI sequence was obtained for the study group, except DW-MRI.
3.5. CT Scan
A CT scan was acquired for each patient with a dual-slice multidetector row scanner (Brivo CT325; GE Healthcare, Waukesha, WI, USA). The CT protocol was as follows: 120 kVp; tube current, 150 - 200 mAs; maximum collimation, 2.5 mm; slice thickness, 2 - 3 mm; and rotation time, 0.5 sec.
3.6. US Examination
The US examinations were performed for the patients, using a Kretztechnik Voluson 730 Expert/Pro Ultrasound Machine (GE Medical Systems/Kretztechnik GmbH, Zipf, Austria) with a linear probe (5 - 18.5 MHz).
3.7. Statistical Analysis
Statistical analyses were performed in R software version 3.6.1 (R Development Core Team, 2013) and SPSS version 25.0 (released in 2017, IBM SPSS Statistics for Windows, Armonk, NY, USA). Variables are expressed as mean ± standard deviation (SD), median, minimum, maximum, percentage, and frequency. Variables were examined after assessing the normal distribution of data and homogeneity of variance, using Shapiro-Wilk test and Levene’s test. Moreover, Chi-square test (χ2) was performed to determine possible significant relationships between categorical variables. The predictive accuracy of the imaging methods for acute appendicitis was also evaluated using the receiver operating characteristic (ROC) curve analysis. A P-value less than 0.05 was considered statistically significant.
4. Results
The demographic characteristics of the patients are presented in Table 1. The mean age of the patients was 31.75 ± 11.74 years (min/max: 11.0/71.0). Forty-four (62.9%) female and 26 (37.1%) male patients were included in this study. The mean appendix diameter was 6.85 ± 2.96 mm in the patients (min/max: 2.8/15.0). Based on the imaging results, 16 (22.9%) patients were diagnosed with appendicitis by US, 23 (32.9%) patients were diagnosed with appendicitis by NECT, and 40 (57.1%) patients were diagnosed with appendicitis by DW-MRI. Of patients who underwent surgery, 37 were surgically proven to have acute appendicitis (SPAA). Based on the comparison of imaging results by gender, no significant difference was found between males and females (Table 2). The images of some of the patients are presented in Figures 1 and 2.
| Variables | Statistics |
|---|---|
| Age, y | |
| Mean ± SD | 31.75 ± 11.74 |
| Median (min/max) | 27.5 (11.00/71.00) |
| Diameter, mm | |
| Mean ± SD | 6.85 ± 2.96 |
| Median (min/max) | 5.80 (2.80/15.00) |
| Diameter, mm | |
| < 6 mm | 35 (50.0) |
| ≥ 6 mm | 34 (48.6) |
| Total | 69 (98.6) |
| Gender | |
| Female | 44 (62.9) |
| Male | 26 (37.1) |
| Total | 70 (100.0) |
| US | |
| Negative | 53 (75.7) |
| Positive | 16 (22.9) |
| Perforated b | 1 (1.4) |
| Total | 70 (100) |
| NECT | |
| Negative | 46 (65.7) |
| Positive | 23 (32.9) |
| Perforated b | 1 (1.4) |
| Total | 70 (100.00) |
| DW-MRI | |
| Negative | 30 (42.9) |
| Positive | 40 (57.1) |
| Total | 70 (100.00) |
| SPAA | |
| Negative | 33 (47.1) |
| Positive | 37 (52.9) |
| Total | 70 (100.00) |
The Demographic Characteristics of the Patients a
| Variables | Female | Male | χ2 | P-value |
|---|---|---|---|---|
| US | 0.968 | 0.616 | ||
| Negative | 32a (60.4) | 21a (39.6) | ||
| Positive | 11a (68.8) | 5a (31.2) | ||
| Perforated b | 1a (100.0) | 0a (0.0) | ||
| Total | 44 (62.9) | 26 (37.1) | ||
| NECT | 0.724 | 0.696 | ||
| Negative | 28a (60.9) | 18a (39.1) | ||
| Positive | 15a (65.2) | 8a (34.8) | ||
| Perforated b | 1a (100.0) | 0a (0.0) | ||
| Total | 44 (62.9) | 26 (37.1) | ||
| DW-MRI | 0.005 | 0.943 | ||
| Negative | 19a (63.3) | 11a (36.7) | ||
| Positive | 25a (62.5) | 15a (37.5) | ||
| Total | 44 (62.9) | 26 (37.1) | ||
| Surgery | 0.388 | 0.533 | ||
| Negative | 22a (66.7) | 11a (33.3) | ||
| Positive | 22a (59.5) | 15a (40.5) | ||
| Total | 44 (62.9) | 26 (37.1) | ||
| Diameter, mm | 0.009 | 0.925 | ||
| < 6 mm | 22a (62.9) | 13a (37.1) | ||
| ≥ 6 mm | 21a (61.8) | 13a (38.2) | ||
| Total | 43 (62.3) | 26 (37.7) |
Comparison of Study Variables Based on Gender a
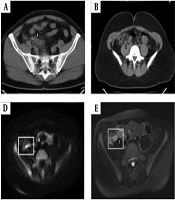
A, A 54-year-old male patient is diagnosed with acute appendicitis surgically. Non-enhanced computed tomography (NECT) shows an enlarged appendix with intraluminal appendicolith (upward arrow) and the surrounding inflamed fatty tissue planes (downward arrow). B, A 23-year-old female patient with acute appendicitis. NECT shows an enlarged and inflamed appendix (arrows). C, An 11-year-old girl with acute appendicitis. Due to tortuosity, the appendix appears to be pseudoreplicated. The US image shows the distending appendix; the arrows represent the appendix. D, Diffusion-weighted magnetic resonance imaging (DW-MRI) shows marked hyperintensity of the appendix with restricted diffusion; the arrow represents the appendix. E, The axial fat-saturated T2W image shows the distending appendix. F, The apparent diffusion coefficient (ADC) image shows marked hypointensity of the appendix with restricted diffusion.
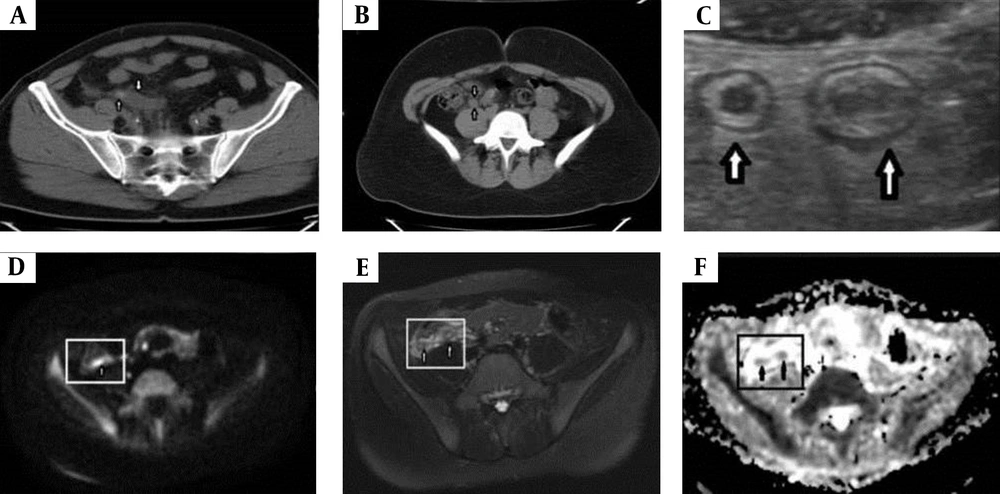
A, A 27-year-old male with acute appendicitis. The US image shows the thick-walled inflamed appendix (arrows). B, Coronal turbo spin echo (TSE) T2W image shows the thick-walled inflamed appendix (arrows). C, Axial TSE T2W image shows the thick-walled appendix and periappendicular fat stranding (arrows). D, Diffusion-weighted magnetic resonance imaging (DW-MRI) shows marked hyperintensity of the appendix with restricted diffusion (arrow). E, The apparent diffusion coefficient (ADC) image shows marked hypointensity of the appendix with restricted diffusion (arrow).
Considering a 6-mm cutoff point for the appendix diameter, 20 (37.7%) patients were found to be negative for appendicitis by US, while 13 (28.3%) patients were negative based on NECT, although the appendix diameter was ≥ 6 mm (Table 3). All appendices with a diameter ≥ 6 mm were diagnosed positively by DW-MRI. The efficiency of imaging methods for SPAA is presented in Table 4. Fourteen (37.8%) patients with SPAA were accurately diagnosed by US; 21 (56.8%) patients with SPAA were accurately diagnosed by NECT; and 37 (100.0%) patients with SPAA were accurately diagnosed by DW-MRI.
| Variables | < 6 mm | ≥ 6 mm | χ2 | P-value |
|---|---|---|---|---|
| US | 12.177 | < 0.001 | ||
| Negative | 33a (62.3) | 20b (37.7) | ||
| Positive | 2a (12.5) | 14b (87.5) | ||
| Total | 35 (50.7) | 34 (49.3) | ||
| NECT | 24.382 | < 0.001 | ||
| Negative | 33a (71.7) | 13b (28.3) | ||
| Positive | 2a (8.7) | 21b (91.3) | ||
| Total | 35 (50.7) | 34 (49.3) | ||
| DW-MRI | 51.560 | < 0.001 | ||
| Negative | 30a (100.0) | 0b (0.0) | ||
| Positive | 5a (12.8) | 34b (87.2) | ||
| Total | 35 (50.7) | 34 (49.3) | ||
| Surgery | 61.443 | < 0.001 | ||
| Negative | 33a (100.0) | 0b (0.0) | ||
| Positive | 2a (5.6) | 34b (94.4) | ||
| Total | 35 (50.7) | 34 (49.3) |
Comparison of Study Variables According to the Appendix Diameter
| Variables | SPAA (No) | SPAA (Yes) | χ2 | P-value |
|---|---|---|---|---|
| US | 11.337 | 0.003 | ||
| Negative | 31a (93.9) | 22b (59.5) | ||
| Positive | 2a (6.1) | 14b (37.8) | ||
| Perforated b | 0a (0.0) | 1a (2.7) | ||
| Total | 33 (100.0) | 37 (100.0) | ||
| NECT | 22.104 | < 0.001 | ||
| Negative | 31a (93.9) | 15b (40.5) | ||
| Positive | 2a (6.1) | 21b (56.8) | ||
| Perforated b | 0a (0.0) | 1a (2.7) | ||
| Total | 33 (100.0) | 37 (100.0) | ||
| DW-MRI | 58.864 | < 0.001 | ||
| Negative | 30a (90.9) | 0b (0.0) | ||
| Positive | 3a (9.1) | 37b (100.0) | ||
| Total | 33 (100.0) | 37 (100.0) |
Comparison of Imaging Methods and Surgical Outcomes a
Table 5 presents the efficiency of imaging methods in diagnosing acute appendicitis. When the significance of AUCs was examined, it was found that all three methods could predict acute appendicitis. However, the lowest significance level was attributed to DW-MRI. The sensitivity of DW-MRI was 100%, and its specificity was 90.90%. There were three patients who were diagnosed with acute appendicitis by DW-MRI, but did not have acute appendicitis surgically. One of these patients had an ovarian torsion, while the other one showed periappendiceal inflammation due to ovarian cyst rupture; DWI positivity was detected secondary to this inflammation. The third patient was also DWI positive with the same mechanism caused by familial Mediterranean fever (FMF) disease". Also, one of the patients showed the appendix perforation (rupture); two patients showed intestinal obstruction, which completely regressed postoperatively; and five patients had postoperative wound infections, who achieved full recovery after antibiotic therapy.
| N | AUC | P-value | Cutoff | Sens. | Spec. | PPV | NPV | |
|---|---|---|---|---|---|---|---|---|
| US | 70 | 0.673 | 0.013 | 0.5 | 40.54 | 93.93 | 0.547 | 0.800 |
| NECT | 70 | 0.768 | < 0.001 | 0.5 | 59.45 | 93.93 | 0.654 | 0.881 |
| DW-MRI | 70 | 0.955 | < 0.001 | 0.5 | 100.00 | 90.90 | 0.896 | 1.00 |
Analysis of the Diagnostic Accuracy of Imaging Methods for Acute Appendicitis
5. Discussion
Acute appendicitis is among the most common causes of admission to emergency departments for lower abdominal pain. Besides, it is the most common disease in young patients, admitted to hospitals with acute abdominal complications (10). Many simple and user-friendly scoring systems have been developed to help predict the risk of acute appendicitis, including physical examinations and inflammatory markers; however, none of these methods have been widely accepted (11-13).
The role of diagnostic imaging in acute appendicitis is subject to controversy (14). Imaging studies have been shown to potentially reduce the rate of negative appendectomy (up to 15%) in patients with clinically suspected acute appendicitis (4). The US examination is a non-invasive method without ionizing radiation, with sensitivity of 71% to 94% and specificity of 81% to 98%. The positive likelihood ratio of US is high, while its negative likelihood ratio is moderate (7, 15). Besides, the US examination, which is a reliable method for confirming the presence of appendicitis, is not considered very reliable in excluding appendicitis (4). The operator’s role in the reliability of US should be also considered. Owing to inconclusive US findings, which cannot visualize the appendix accurately, further imaging studies are needed (4).
The diagnostic accuracy of US is especially reduced in obese patients due to increased subcutaneous and intraabdominal fat content. On the other hand, Anderson et al. (16) reported that the body mass index did not affect the diagnostic accuracy of CT scans. Moreover, it was reported that abdominal CT scan has 76 - 100% sensitivity and 83 - 100% specificity for the diagnosis of acute appendicitis; therefore, it is superior to US. Despite the high sensitivity and specificity of CT scan, its application has been a cause for concern due to radiation, especially in children and pregnant women. Accordingly, MRI is used for pregnant women and children with uncertain US findings (17).
In a recent meta-analysis of MRI findings in 363 patients with appendicitis, it was reported that MRI has a sensitivity of 92 - 99%, a specificity of 94 - 99%, a positive likelihood ratio of 16.3, and a negative likelihood ratio of 0.09 (18); these rates are almost comparable to those of CT imaging. MRI has been reported as a viable alternative to CT scan for secondary imaging in the diagnosis of acute appendicitis in children. Besides, MRI can distinguish perforated appendicitis from non-perforated appendicitis with high specificity (19). However, it is a costly procedure, and interpretation of MR images requires experience. Therefore, the use of MRI for the diagnosis of acute appendicitis seems to be limited to pregnant women and children (4). Nevertheless, it is recommended to use MRI to confirm or exclude acute appendicitis and to distinguish perforated from non-perforated appendicitis, especially in elderly patients with Alvarado scores ≥ 5, who cannot undergo an intravenous contrast-enhanced CT scan for different reasons (e.g., acute or chronic kidney disease) (20).
In the present study, we examined different diagnostic methods, including US, DW-MRI, and NECT for the diagnosis of acute appendicitis. In this regard, Lee et al. (21) reported that the use of US instead of CT scan for adolescents and adults with suspected appendicitis may increase the negative appendectomy rate; however, this does not affect the perforation rate significantly. Moreover, a meta-analysis compared the accuracy of US, CT, and MRI examinations for clinically suspected acute appendicitis in children. MRI was slightly superior to US and CT, but the difference was not statistically significant (22).
In the present study, diagnosis of appendicitis by US, CT, and DW-MRI was significantly associated with SPAA. Overall, 37.8%, 56.8%, and 100% of patients with SPAA could be accurately diagnosed by US, NECT, and DW-MRI examinations, respectively. The sensitivity and specificity of US, NECT, and DW-MRI were estimated at 40.50% and 93.93%; 59.45% and 93.93%; and 100% and 90.90%, respectively. In this study, all three patients with false positive results on DW-MRI showed periappendiceal inflammation for different reasons. Although the sensitivity and specificity of US and NECT were lower than previous studies, the performance of DW-MRI was similar to or even better than previous reports.
It has been reported that the accurate diagnosis of appendicitis depends on demographic factors, such as age and gender (23). In this regard, a previous study showed that diagnosis of acute perforated and non-perforated appendicitis was dependent on age and gender (24). However, in the current study, demographic factors, such as age and gender, were not closely related to the diagnostic approach or emergency surgery. Besides, a recent study suggested that the appendix diameter should be 7 mm for a definitive diagnosis of acute appendicitis (25). Considering the importance of the appendix diameter, it has been recommended to include the axial diameter of the appendix in the diagnostic US examination to improve the Alvarado score (26).
The present study revealed that the diameter of the appendix is an important factor in the accurate diagnosis of appendicitis by DW-MRI and US examinations; this finding is consistent with the results reported in the literature. In this study, there were some cases with an appendix diameter larger than normal (≥ 6 mm). Conversely, there were cases with an appendix diameter < 6 mm due to perforation. In these cases, signs of inflammation, such as extraluminal fluid accumulation and mesenteric fat, were observed. The DWI technique enabled the diagnosis of two non-perforated patients, whose appendix diameter was less than normal (6 mm). Although in appendicitis, the appendix diameter is < 6 mm, according to the literature, acute appendicitis is still suspected. In such critical cases, DW-MRI can be recommended for diagnosis.
The present results demonstrated the efficacy of DWI in diagnosing critical appendicitis cases both rapidly and accurately, even if there is a limited scope for interpretation. The clinical diagnoses and patient outcomes were satisfactory when the US, NECT, and DW-MRI were performed as rapid diagnostic modalities for deciding on an emergency surgery. Moreover, this technique is safe, cost-effective, and affordable for patients. It may be also an appropriate alternative to CT scan. Therefore, DW-MRI and US examinations can be used in combination for an accurate diagnosis and surgical decision-making for individual patients.
In conclusion, based on the present findings, DW-MRI is a reliable, successful, and accurate technique, even when the appendix diameter is smaller than normal. Therefore, it may be useful for a critical and accurate diagnosis of acute appendicitis. However, further studies with a larger sample size may help establish the obtained results.