1. Introduction
Prostate-specific membrane antigen (PSMA), which is highly expressed in prostate carcinoma cells, is a type II transmembrane protein. Gallium-68-labeled PSMA (68Ga-PSMA) is a relatively novel radiotracer, which targets PSMA and can detect cancer relapse and metastasis. PSMA is also expressed in the neovasculature of various solid malignant tumors, including clear cell renal cell carcinoma (ccRCC). For the first time, Demirci et al. reported a case of ccRCC with 68Ga-PSMA uptake (1). The 68Ga-PSMA positron emission tomography/computed tomography (PET/CT) scan is potentially useful in patients with RCC recurrence to detect metastasis. Moreover, 68Ga-PSMA PET/CT may detect lung cancer lesions; however, further investigation is needed.
2. Case Presentation
We present the case of a 65-year-old man with a history of right lower lobe adenocarcinoma in 2015 and a subsequent diagnosis of ccRCC of the left kidney in 2018. Both conditions were treated with a right lower lobectomy and a left partial nephrectomy, respectively. Also, they were evaluated using 18F-fluorodeoxyglucose (18F-FDG) PET/CT scan before surgery. As an age screening protocol, the prostate-specific antigen (PSA) level was examined annually. An increase in PSA (15.98 ng/mL) was detected in the follow-up for the first time in September 2020. The initial transrectal and pelvic ultrasounds demonstrated a hypoechoic lesion in the right peripheral zone of prostate, which was confirmed via pelvic magnetic resonance imaging (MRI), as it indicated a lesion at the same site with low T2 signals, restricted diffusion, and reduced apparent diffusion coefficient (ADC).
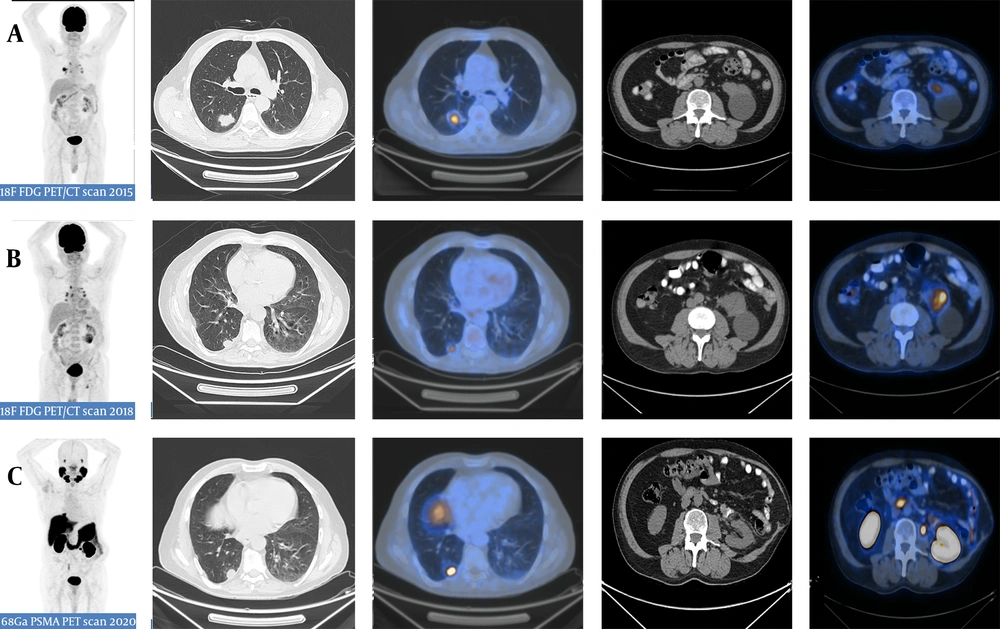
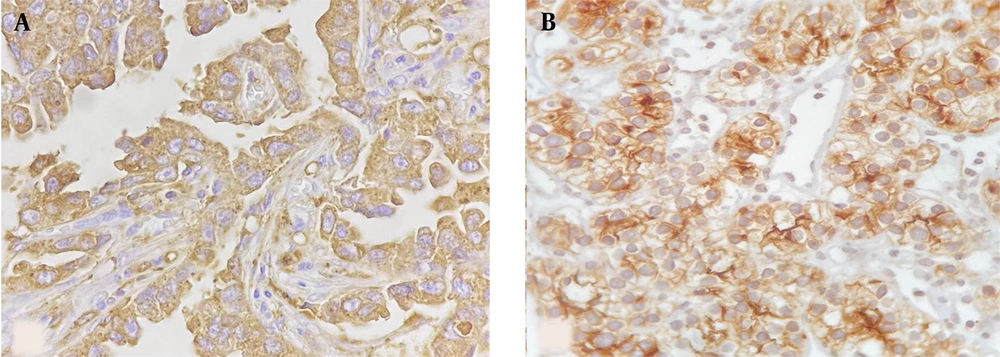
The subsequent transrectal prostate biopsy demonstrated prostate adenocarcinoma with a Gleason score of eight. Although not recommended by the National Comprehensive Cancer Network (NCCN) guidelines, the patient was referred for 68Ga-PSMA PET/CT scan for the initial staging and metastatic evaluation. The 68Ga-PSMA PET/CT scan demonstrated 68Ga-avid lesions in both lung and kidney surgical beds, along with prostate as the primary tumor site (Figure 1). There was no other 68Ga-PSMA avid lesion in the study. The subsequent biopsy of the right lung and the left kidney surgical bed lesions was consistent with non-small cell lung carcinoma and ccRCC, respectively (Figure 2).
A 65-year-old man with a history of two surgeries for lung adenocarcinoma and renal cell carcinoma, presenting with a peripheral prostate lesion that was confirmed as prostate adenocarcinoma in the histopathology. The patient underwent Gallium-68-labeled prostate-specific membrane antigen (68Ga-PSMA) PET/CT scan for prostatic cancer staging. Three consecutive PET/CT scans were performed. The first 18F-fluorodeoxyglucose (18F-FDG) PET/CT scan (A) in 2015 demonstrated a hypermetabolic lesion in the right lower lobe, while no significant hypermetabolic lesion was detected in the left kidney despite an apparent simple cyst. The second 18F-FDG PET/CT scan (B) in 2018 demonstrated the recurrence of the hypermetabolic lesion in the right lower lobe, besides the emergence of a new hypermetabolic lesion adjacent to the left renal cystic lesion. The third PET/CT scan (C) with prostate-specific membrane antigen (PSMA) in 2020 demonstrated the recurrence of both right lung adenocarcinoma and left RCC lesions in the respective surgical beds.
3. Discussion
The expression of PSMA has been demonstrated in the neovasculature of various malignancies other than prostate cancer, including breast adenocarcinoma, colorectal adenocarcinoma, transitional cell carcinoma, glioblastoma multiforme, pancreatic ductal and gastric adenocarcinomas, and a variety of renal tumors, including ccRCC, papillary RCC, oncocytomas, and angiomyolipomas (2). However, breast, lung, colorectal, and renal cell carcinomas are the most common primary tumors with PSMA expression (3, 4).
Siva et al. published a case series, including eight patients with RCC, undergoing both 18F-FDG and 68Ga-PSMA PET imaging. The PSMA uptake was typically more intense than FDG in RCC. Both PET radiotracers demonstrated treatment response before the emergence of morphological changes on either CT or MRI. They concluded that PSMA PET scan is suitable for diagnostic and response assessments in metastatic RCC patients after local treatments (5).
Mads et al. reported an interesting case of primary lung adenocarcinoma in a 70-year-old man with prostate cancer on 68Ga-PSMA PET scan for the first time in 2018 (6). On the other hand, Pyka et al. reported that 68Ga-PSMA PET scan cannot differentiate between pulmonary metastasis and primary lung tumors in patients with prostate cancer. They found no clear reason for the high PSMA uptake in non-prostate cancer lesions. However, they hypothesized that PSMA protein expression in the neovasculature can be related to other factors, such as tracer binding to proteins other than PSMA (7). Nadebaum et al. also described the “flip-flop” phenomenon using 68Ga-PSMA and 18F-FDG PET/CT scans in a patient with sarcomatoid RCC. Areas with a slow recurrence and a low grade of sarcomatoid differentiation demonstrated intense 68Ga-PSMA expression with a low 18F-FDG uptake (8).
Overall, 68Ga-PSMA PET/CT scan is potentially useful for patients with RCC recurrence to detect metastasis; it may be also used for the assessment of treatment response to novel therapeutic agents (9, 10). The expression of PSMA may be considered as an indicator of lutetium-177 (177Lu)-PSMA therapy efficacy and an alternative treatment for patients with RCC recurrence. However, further studies with a larger sample size (9, 11) and prospective trials are needed to evaluate PSMA-targeted agents for imaging and treatment of non-prostate neoplasms. Also, the role of 68Ga-PSMA PET scan in the evaluation of lung cancer lesions is less understood, and further research is necessary.
In conclusion, we found the expression of PSMA in a patient with concurrent renal and pulmonary cancers. Based on the findings, 68Ga-PSMA PET scan is a potentially useful tool for the evaluation and treatment of tumors other than prostate cancer with PSMA expression. Nonetheless, further investigation is needed on a larger sample size to confirm its potential role.
.jpg)