1. Background
Breast cancer remains one of the major public health problems around the world, with more than two million female cases reported in 2018 (1). Nonetheless, early detection of small tissue changes can improve both morbidity and mortality rates of this disease (2). Notably, studies have reported five-year survival rates of approximately 85% and 27% in women diagnosed with regional and distant breast cancer, respectively, with the survival rate increasing considerably to 99% in women with locally diagnosed breast cancer (3).
Mammography, which involves scanning of the breasts, remains the most universally accepted screening tool for the early detection of breast cancer. Evidence suggest that a poor mammographic image quality is correlated with the occurrence of interval cancer (4). Therefore, the clinical efficacy of mammography is largely dependent on the images acquired by radiographers. In clinical practice, radiographers encounter different challenges and difficulties due to technological advances, patient interactions, individual needs, and requirements for continuous professional development (5). A recent integrative review reported that the challenges of European radiographers were related to patient positioning, breast compression, contrast, noise, sharpness, and labeling; such difficulties have been also identified in previous studies outside Europe (5). Besides, the primary image quality assessment may be challenging for radiographers. In this regard, the results of a previous study showed that 3% to 50% of mammography-based image quality monitoring did not adequately satisfy the quality criteria (6).
2. Objectives
This study aimed to describe the challenges and difficulties of radiographers in daily practice and to investigate the radiographers’ knowledge of image quality assessment tools.
3. Patients and Methods
3.1. Sample and Data Collection
This online questionnaire study, which was approved by the Ethics Committee of King Fahad Medical City (IRB 2033-8E) in Riyadh, Saudi Arabia, was performed on Saudi radiographers with experience of mammography. Non-Saudi participants were also included in this survey for comparison. Data were collected between September 2020 and February 2021. The non-probability sampling method (snowball sampling) was used to recruit the participants. A participation consent form was also attached to the web link of the questionnaire before the survey. The Research Electronic Data Capture (REDCap), which is a Health Insurance Portability and Accountability Act (HIPAA)-compliant and validated survey tool (7), was used to ensure data protection and security.
3.2. Questionnaire Design
To meet the study objectives, a 15-item questionnaire was developed based on previously published studies (5-9). The survey was divided into four main sections. Section 1 was related to the demographic and professional information (8 questions), including nationality, type of work, age, level of education, experience in mammography, number of mammograms per week, and type of workplace (i.e., private, public, or breast screening center). Section 2, which was related to the radiographers’ practice, included two questions. One question was related to 12 ACR criteria used for evaluating the positioning quality of mammograms, while the other question was related to the individual’s familiarity with the image quality evaluation systems or tools, including the Perfect, Good, Moderate, Inadequate (PGMI), Excellent, Acceptable, Repeat (EAR), European Guidelines on Quality Criteria for Diagnostic Radiographic Images (EUROPEAN), and ACR tools.
Section 3 consisted of two multiple-choice questions. One of the questions was related to reasons for repeat mammography in daily practice (8 items), and the other one was related to the challenges of mammographers during daily practice (13 items). Section 4 was related to continuing professional and educational development. It included two questions for individuals who were willing to continue their education. One question was related to the area of development (7 items), and the other one was related to the preferred location for education. The survey questions were generally close-ended, multiple-choice, dichotomous, or based on a three- or six-point Likert scale. Due to missing responses, the total number of the respondents might vary for each question.
The present survey was validated by an academic expert in mammography and then sent to an experienced radiographer to ensure that the survey language and questions were understandable. Moreover, the tool was pretested among 17 participants to assess its clarity and applicability, identify difficulties, estimate the survey completion time, and determine whether the participants interpreted and understood each item as intended by the researchers.
3.3. Statistical Analysis
Considering the study subject, descriptive and analytical approaches could be applied in the theoretical section to acquire accurate knowledge of the elements of the problem by determining different theoretical aspects of the subject. Also, for an accurate and detailed description of the phenomenon, analyses were performed to obtain scientific results in an objective manner. Descriptive statistics (frequency and percentage) were measured to summarize the participants’ characteristics. Since this study focused on Saudi mammographers, comparison between Saudi and non-Saudi mammographers was carried out for each item; the results are presented in tables and bar charts. Moreover, the internal validity, internal consistency, and construct validity of the Likert-scale items were determined by calculating the correlation coefficients. Besides, the correlation of selected variables with the image evaluation tools and ACR image quality assessment scales was investigated. Cronbach’s alpha coefficient was also measured to determine the reliability of the scales, as well as the questionnaire.
4. Results
4.1. Questionnaire Validity
A number of tests were performed to ensure the validity and reliability of the questionnaire. Its validity was examined based on two measures, that is, internal consistency and construct validity.
4.1.1. Internal Consistency
Internal validity was the primary statistical measure used to examine the validity of the questionnaire. It was determined by measuring the correlation coefficient between each item in the construct and the total scale. Table 1 presents the internal consistency of the questionnaire sections with a specific scale for rating responses.
| No. | Item | Correlation coefficient | P value |
|---|---|---|---|
| Q9. Which of the following 12 quality elements do you use to evaluate the positioning quality of an image? | |||
| 1. | Visualization of posterior breast tissue on both CC and MLO views. | 0.407** | < 0.001 |
| 2. | Sagging of the breasts on the MLO view. | 0.663** | < 0.001 |
| 3. | Amount of the pectoral muscle observed on the MLO view. | 0.499** | < 0.001 |
| 4. | Inframammary fold seen on the MLO view. | 0.574** | < 0.001 |
| 5. | Breast positioned too high relative to the image receptor on the MLO view. | 0.545** | < 0.001 |
| 6. | The skin folds significantly obscure tissue visualization. | 0.644** | < 0.001 |
| 7. | The PNL on the CC view measures within 1 cm of the same measurement on the MLO view. | 0.228 | 0.052 |
| 8. | Excessive exaggeration of the breast on the CC view. | 0.588** | < 0.001 |
| 9. | The portion of breast tissue cut off on the image. | 0.703** | < 0.001 |
| 10. | Other body parts projected over the breast. | 0.685** | < 0.001 |
| 11. | Nipple in profile | 0.476** | < 0.001 |
| 12. | Motion artifacts | 0.768** | < 0.001 |
| Q10: Which of the following image quality evaluation systems (tools) are you familiar with? | |||
| 1. | PGMI | 0.787** | < 0.001 |
| 2. | EAR | 0.788** | < 0.001 |
| 3. | EUROPEAN | 0.751** | < 0.001 |
| 4. | ACR | 0.709** | < 0.001 |
The Correlation Coefficients of Each Item for Question 9 and Question 10
For question 9, the P value was less than 0.05 for each item, except item 7, which stated that “the posterior nipple line (PNL) on the craniocaudal (CC) view measures within 1 cm of the same measurement on the mediolateral oblique (MLO) view”. Therefore, the correlation coefficients of the majority of items were significant at P ≤ 0.05. It can be stated that this section was valid for measuring what it was intended to measure for achieving the main goal of this study (except item 7). For question 10, the P value was less than 0.05 for each item; therefore, the correlation coefficients were significant (P ≤ 0.05). It can be concluded that this section was valid for measuring what it was supposed to measure for achieving the main goal of this study.
4.1.2. Construct Validity
The second statistical measure used to examine the validity of the questionnaire was construct validity. This measure evaluates whether a tool reflects the intended construct and is central to establishing the overall validity of a method. For Q.9 and Q.13, the correlation coefficients were significant at r = 0.648 (P ≤ 0.05) and r = 0.384 (P ≤ 0.05), respectively. However, for Q10, the correlation coefficient was not significant (r = 0.129, P = 0.275).
4.2. Questionnaire Reliability
Generally, the reliability of an instrument is the degree of consistency with which it measures an attribute it is supposed to measure. The less variation an instrument produces in repeated measurements of an attribute, the higher its reliability is. Overall, reliability refers to the stability, consistency, or dependability of a measuring tool. The Cronbach's alpha coefficient was equal to 0.592 for the total questionnaire, which indicates its fair reliability. Therefore, the questionnaire was fairly valid and reliable for a pilot study.
4.3. Background Characteristics of the Participants
A total of 100 radiographers participated in this survey. The participants who only completed the demographic section were excluded from the analysis (n = 27). The majority of the participants were full-time radiographers (92%), aged 20 - 23 years, with a bachelor’s degree. Almost half of the participants were Saudi radiographers (52%). Nearly 77% of the respondents were working as a mammographer at the time of the study (Table 2). The mean number of patients was 27.3 per week (n = 69; maximum, 140; minimum, 2; standard deviation, 27.4).
| Characteristics | No. (%) |
|---|---|
| Nationality | |
| Saudi | 38 (52) |
| Non-Saudi | 35 (48) |
| Age group (y) | |
| 20 - 29 | 29 (39.7) |
| 30 - 39 | 29 (39.7) |
| 40 - 49 | 15 (20.6) |
| Healthcare institution | |
| Breast screening center | 14 |
| Public | 49 |
| Private | 9 |
| Education | |
| Bachelor’s degree | 45 (61.6) |
| Diploma | 20 (27.4) |
| Master’s degree | 8 (11) |
| Experience (y) | |
| 1 - 3 | 26 (35.6) |
| 3 - 5 | 11 (15.1) |
| < 1 | 5 (6.8) |
| > 5 | 30 (42.5) |
| Working in the mammography unit and other imaging units | 56 (76.7) |
| Only working in the mammography unit | 17 (23.3) |
Demographic and Professional Characteristics of the Participants
4.4. Radiographers’ Knowledge of Image Quality Assessment Tools
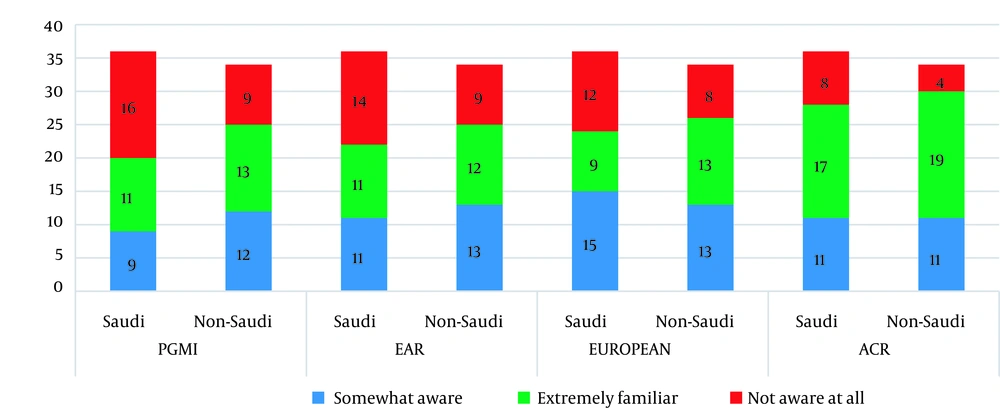
The participants’ knowledge of image quality assessment tools is presented in Figure 1. Among the evaluated tools, the ACR manual was the most familiar tool for both Saudi and non-Saudi participants (52%).
The radiographers’ knowledge level of different image quality evaluation tools, including the perfect, good, moderate, inadequate (PGMI), excellent, acceptable, repeat (EAR), European Guidelines on Quality Criteria for Diagnostic Radiographic Images (EUROPEAN), and the American college of Radiology (ACR) criteria
The Saudi participants were not familiar with the EAR, PGMI, and EUROPEAN tools as compared to non-Saudi participants. The results indicated the good inter-item reliability (Cronbach’s alpha, 0.77). In terms of construct validity, the correlation coefficient for question 10 was r = 0.65 (P < 0.001). The results showed a positive correlation between the knowledge of image evaluation assessment tools (EAR, PGMI, EUROPEAN, and ACR) and age group, experience in mammography, and number of patients per week (Table 3).
| Variables | Scales | |
|---|---|---|
| Image evaluation tools, r (P value) | American College of Radiology image quality assessment, r (P value) | |
| Nationality | 0.16 (0.17) | 0.16 (0.16) |
| Age group | 0.4 (0.001) b | 0.17 (0.14) |
| Education | -0.16 (0.17) | 0.6 (0.60) |
| Occupational status | 0.07 (0.52) | -0.15 (0.19) |
| Experience in mammography | 0.3 (0.01) b | -0.01 (0.73) |
| Number of patients per week | 0.3 (0.02) b | 0.14 (0.22) |
Correlation Analysis Between the Selected Variables and Image Evaluation Tools (Q10) and the American College of Radiology Image Quality Assessment (Q9) Scale a
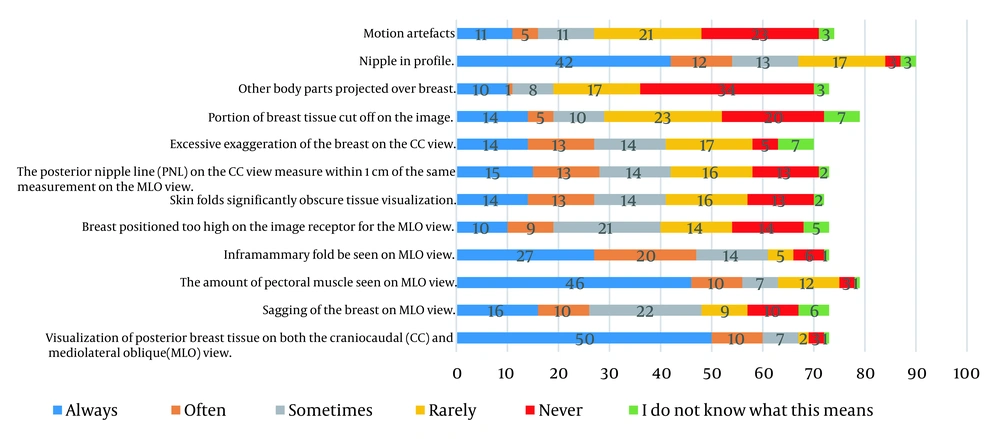
The participants were then asked to rate the items used to assess positioning based on the ACR (Figure 2). Based on the results, the most frequently used item was posterior breast tissue visualization on both CC and MLO views (Saudi, n = 25 vs. non-Saudi, n = 25), followed by the pectoral muscle volume on the MLO view (Saudi, n = 22 vs. non-Saudi, n = 24) and nipple in profile (Saudi, n = 21 vs. non-Saudi, n = 21). On the other hand, other body parts projected over the breast (Saudi, n = 21 vs. non-Saudi, n = 13), motion artifacts (Saudi, n = 14 vs. non-Saudi, n = 9), and portion of breast tissue cut off on the image (Saudi, n = 14 vs. non-Saudi, n = 6) were never used by the participants to assess the quality of mammograms.
The ACR items showed good inter-item reliability (Cronbach’s alpha, 0.81). In terms of construct validity, the correlation coefficient was not significant (r = 0.13, P = 0.28). Regarding the correlations with the selected variables in Table 3, no significant correlation was found with the ACR image quality assessment scale.
4.5. Clinical Practice Challenges Perceived by Radiographers
Regardless of nationality, the majority of the participants considered positioning as the main reason for repeat mammography in daily practice (Table 4). The results showed that image artifact was the second most common reason, regardless of the radiographer’s nationality, followed by breast compression.
| Number of times documented | ||
|---|---|---|
| Saudi participants | Non-Saudi participants | |
| Positioning | 26 | 25 |
| Artifact | 20 | 14 |
| Compression | 8 | 13 |
| Examination identification | 8 | 8 |
| Sharpness | 2 | 5 |
| Contrast | 2 | 6 |
| Exposure | 7 | 6 |
| Noise | 4 | 5 |
Reasons for Repeat Mammography in Daily Practice
In this study, Saudi radiographers reported that breast compression (pain management) was the most challenging item during patient positioning, followed by the patient’s inability to remain in the correct position, reduced range of movement in the shoulder/neck, and being overweight or wheelchair-bound (Table 5). In contrast, among non-Saudi radiographers, the positioning of wheelchair-bound patients was cited as the main challenge, followed by positioning of overweight patients. Other challenges during patient positioning are reported in Table 5.
| Number of times documented | ||
|---|---|---|
| Saudi participants | Non-Saudi participants | |
| Breast compression (pain management) | 21 | 16 |
| Patient’s inability to remain in the correct position | 18 | 11 |
| Reduced range of movement in the shoulder/neck | 18 | 14 |
| Overweight patients | 18 | 17 |
| Wheelchair-bound patients | 18 | 24 |
| Skeletal malformations | 12 | 11 |
| Patient’s refusal to undergo additional imaging | 10 | 12 |
| Management of anxiety and stress in patients | 10 | 12 |
| Cognitive limitations | 7 | 8 |
| Patients with breast implants | 6 | 11 |
| Switching from manual to automatic exposure control | 8 | 6 |
| Periodic quality control machine tests | 7 | 3 |
Challenges Cited by the Participants During Patient Positioning
4.6. Continuing Professional and Educational Development
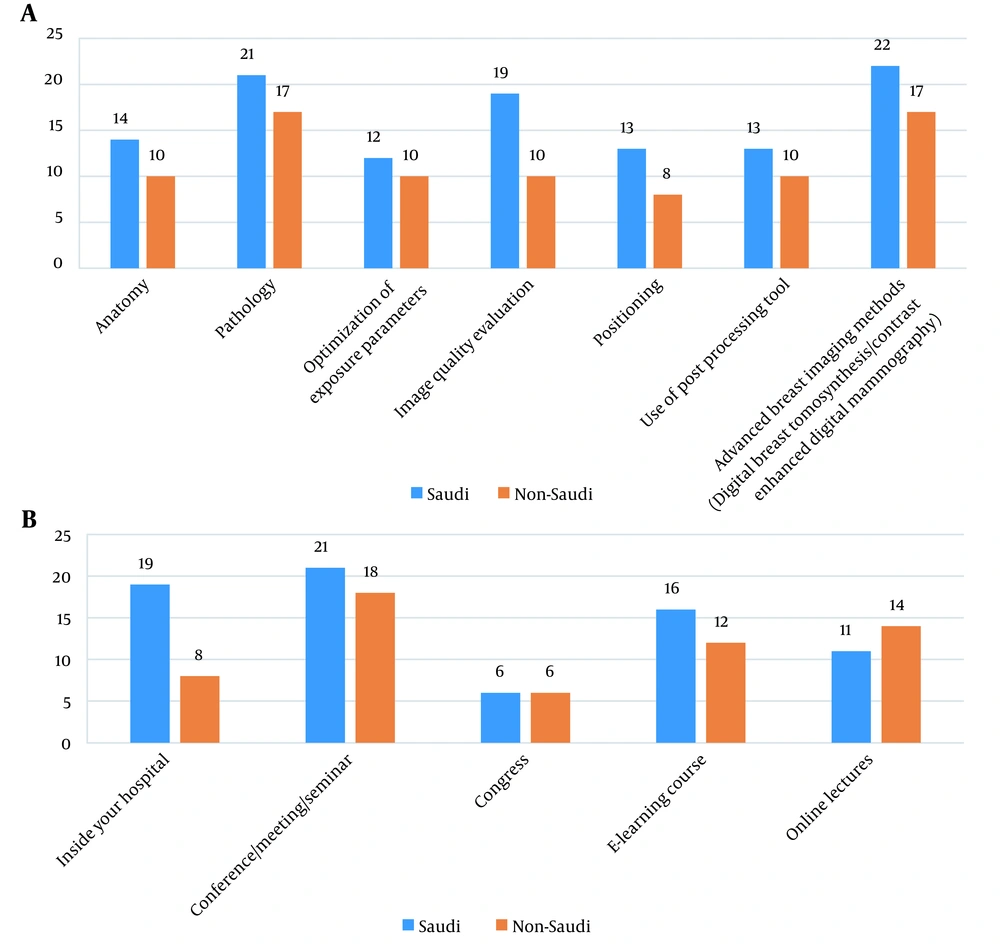
The majority of the participants (n = 52) reported the need for additional education in mammography. The topics that were preferred by Saudi and non-Saudi radiographers were advanced breast imaging methods, breast pathology, and image quality evaluation, respectively (Figure 3A). In terms of location and setting, conferences/meetings/seminars were preferred by the participants (Saudi, n = 21; non-Saudi, n = 18) to advance their professional and educational development in mammography. Also, learning at hospital was the second most preferred location for the Saudi participants versus online lectures for the non-Saudi participants (Figure 3B).
5. Discussion
Radiographers play a central role in acquiring high-quality mammographic images through not only quality control, but also appropriate breast compression and positioning (6). The current study aimed to explore the radiographers’ knowledge of image quality assessment tools and to understand the current challenges and difficulties in daily practice. Radiographers assessing mammographic images need to comply with the guidelines established to ensure standardization in clinical practice (10, 11). For this purpose, radiological organizations use different assessment methods, which include criteria for both positioning and image analysis (11). Notably, the present results showed the acceptable level of radiographers’ knowledge about the ACR tool (52%), but not other evaluation methods (Figure 1). However, given the small sample size of this study, larger and more representative studies are required to accurately measure their level of knowledge.
The quality of a mammogram is greatly influenced by breast positioning, which determines the amount of breast tissue included in the image (10). One of the most widely used methods for assessing the positioning quality of images is the 12-item ACR tool (Figure 2). The present findings showed that posterior breast tissue visualization was the most frequently used item on both CC and MLO views, followed by the pectoral muscle volume on the MLO view and nipple in profile. Although these items are important, a comprehensive positioning assessment, including all ACR elements, is necessary. For instance, one of the most important indicators of mammographic image quality on the MLO view is the measurement of PNL. Based on the ACR tool, images are considered acceptable when PNL is seen at the level of or above the inferior aspect of the pectoral muscle (9). However, the present results showed that only 38% of the radiographers used the PNL for assessing the image quality. For comparison, 71% of Australian radiographers used the PNL in the clinical setting (9).
Moreover, other important positioning indicators, such as projection of other body parts over the breast, motion artifacts (60%), and cutoff breast tissue portions from the image (70%), were rarely or never applied (Figure 2). This could be attributed to the design of the current cohort, in which 52% of the participants were familiar with the ACR tool (Figure 1); however, further studies with a larger sample size are recommended to validate our findings.
Although today, digital technologies can automatically handle the majority of software and hardware factors, positioning is still highly dependent on the radiographer's experience (5). Consistent with previous reports (5, 10, 11), the present results indicated that, irrespective to the radiographer’s nationality, positioning was the main cause of repeat mammography in daily practice (Table 4). The second leading cause of repeat mammography was image artifact, which can be explained by the fact that only 15% of the participants had always used motion artifact to evaluate a mammogram based on the ACR image quality standards (Figure 1). In contrast, a previous study reported that blurred mammograms and noise were the main reasons for repeat procedures (6); however, they were less frequently cited in the current study. Overall, more attention must be paid to repeat imaging owing to its association with increased patient anxiety, cost, and workflow issues, besides unwanted radiation exposure.
The current study found that breast compression was the main patient positioning challenge for Saudi radiographers, while it was ranked the third by non-Saudi radiographers (Table 5). In this study, breast compression was the third most important reason for repeat mammography (Table 4). Breast compression has been shown to not only affect the image quality and radiation dose, but also women’s experience of pain/discomfort (5). A recent study showed that 88% (n = 140) of European radiographers found compression to be a challenging task, especially during painful examinations (6). In previous research, variations in breast compression have been reported, which can be largely related to the absence of or differences in guidelines/recommendations for optimal compression force. Also, these variations may be related to the pain threshold of women, uncertainties or inaccuracies in estimating the pressure applied to the breast, radiographer’s sensitivity to pain expression, and radiographer’s perspective of a good compression (6).
Another important challenge encountered in daily practice by radiographers was related to the positioning of wheelchair-bound patients (Table 5). This challenge was ranked the first by non-Saudi radiographers and the second by Saudi radiographers. Therefore, besides anatomical knowledge and positioning skills, the patients’ individual needs (e.g., special needs of patients with physical disabilities) should be also incorporated into the radiographer’s continuing education.
According to the present results, the majority of the participants expressed their interest in developing their knowledge of advanced breast imaging methods, followed by pathology and image quality evaluation. In the design of future educational and training courses, the needs of mammographers should be considered by professional bodies in the workplace. Additionally, in an integrative review of studies on European mammographers, all studies identified the need for further training over a wide range of contents or issues to provide mammography services at higher quality and improve clinical practice (5).
To the best of our knowledge, there is no specific continuing professional development (CPD) program for radiographers working in mammography units in Saudi Arabia. However, a study in the Netherlands showed that despite mandatory CPD programs every three years, the positioning quality decreased compared to initial courses (6). This study stressed the need for setting individual targets, continuous monitoring, and more frequent training, if necessary, to maintain the mammographic positioning skills up-to-date.
According to previous studies, less attention has been paid to mammography training and education compared to other imaging modalities, which might compromise advances in this field (5). However, the European Reference Organization for Quality Assured Breast Screening and Diagnostic Services (EUREF) guidelines recommend that radiographers working in mammography units attend 40 hours of CPD training per year to improve their basic skills and stay up-to-date (5). Australia has also established the Breast Imaging Clinical Education Program (BICEP), which is a CPD program intended for diagnostic radiographers performing breast imaging. This program provides mammography certification for radiographers with experience of breast imaging for three years (12). Therefore, establishing a mammography certification program is vital in Saudi Arabia to improve the mammographers’ skills.
Some limitations of the present study need to be addressed. First, the small sample size certainly limited the validity of the results, highlighting the need for larger, well-designed studies with sufficient statistical power. However, our study sample size was similar to that of the study by Richli Meystre et al. (6) and even exceeded that of the study by Abuzaid et al. (13).
In conclusion, this pilot study highlighted the importance of developing in-house training courses for radiographers, with the involvement of radiologists, to focus on positioning, image quality evaluation, breast compression, and patient-centered needs for improving clinical practice standards. Given the scarcity of local studies on radiographers’ needs in Saudi Arabia, the present study can offer several avenues for future research.