1. Background
The increased application of 68-gallium prostate-specific membrane antigen (68Ga-PSMA) positron emission tomography/computed tomography (PET/CT) scan has significantly improved the quality of clinical management and treatment for patients with prostate cancer. With an increase in the prostate-specific antigen (PSA) level following radical prostatectomy and radiotherapy, tumor lesions are anticipated outside the treated area (1, 2). It has been shown that 68Ga-PSMA PET/CT scan can detect tumor lesions outside the prostatectomy bed with high accuracy (3). By using this modality, extra-prostatic lesions associated with increased PSA levels, such as metastatic pelvic lymph nodes, are detectable (4).
Additionally, in patients with a progressive increase in PSA after treatment, recurrent prostate cancer is indicated by a positive 68Ga-PSMA PET/CT finding, followed by biopsy confirmation (5). Therefore, 68Ga-PSMA PET/CT can potentially change the treatment plan if the results are positive (6, 7). In a previous study, based on the findings of 68Ga-PSMA PET/CT scan, the treatment protocols were modified for 42% of prostate cancer patients (8). The use of 68Ga-PSMA PET/CT technique also allows for the delineation of tumor itself with high accuracy (9); therefore, a more targeted regional therapy will be possible after an accurate measurement of the tumor burden (10). Overall, diagnosis and assessment of treatment response in prostate cancer is a major challenge, as both the serum PSA level and conventional imaging have potential limitations. The 68Ga-PSMA PET/CT scan seems to be a valuable radiotracer in the evaluation of prostate cancer recurrence and metastasis with high sensitivity (11).
2. Objectives
Although the correlation between the PSA level, tumor stage, and the Gleason score has been investigated to some extent, the present study aimed to evaluate the value of 68Ga-PSMA PET/CT scan findings in prostate cancer patients with regard to the Gleason score, PSA level, and metastatic burden and to determine their relationship with other tumor characteristics.
3. Patients and Methods
3.1. Patients
In this cross-sectional study, 80 male patients with a definitive diagnosis of prostate cancer, who were candidates for 68Ga-PSMA PET/CT scan for both initial staging and restaging, were included. Restaging indicated biochemical recurrence, characterized by a detectable PSA level after being documented undetectable following a definitive primary treatment. Any prostate cancer patient who was not initially treated with a definitive therapy was excluded from the study.
3.2. Variables
In this study, the examined variables included the PSA level (based on the laboratory results), the Gleason score (based on the pathology report), and the maximum standardized uptake value (SUVmax) (amount of radiotracer uptake in the tumor lesion).
3.3. Imaging Protocol/Analysis
All patients were injected with 68Ga-PSMA intravenously one hour before imaging. The injection dose was calculated as 2 MBq/kg, according to the Society of Nuclear Medicine and Molecular Imaging (SNMMI) guidelines. All PET/CT images were acquired using a Discovery 690 Visual Configuration Tool (VCT) system (GE Healthcare Systems, Milwaukee, Wisconsin, USA), equipped with a 64-slice CT scanner (LightSpeed VCT CT system, GE Healthcare, Milwaukee, Wisconsin, USA). Imaging was initiated with CT scan from the vertex to the mid-thigh, followed by PET scan from the mid-thigh to the vertex (three minutes for each bed position).
Image analysis was performed using the Advantage Workstation Version 4.5 (ADW4.5) software. The SUVmax for Tumor lesions was calculated on the workstation by drawing a region of interest (ROI) around each lesion. A cut-off value ≥ 4 was considered significant for SUVmax to differentiate benign from malignant 68Ga-PSMA-avid lesions (10). Any 68Ga-PSMA uptake outside the prostate bed, especially in the lymph nodes, bones, and visceral organs, was considered metastatic.
3.4. Ethical Considerations
This study was approved by our institutional review board, with an ethical code of IR.SBMU.MSP.REC.1398.196. Written consent was obtained from all the patients to use their clinical data.
3.5. Statistical Analysis
For statistical analysis, data are presented as mean ± standard deviation (SD) for quantitative variables and as frequency and percentage for categorical variables. Continuous variables were compared using t-test or Mann-Whitney test if the data did not have a normal distribution or when the assumption of equal variance was violated across the study groups. Categorical variables were compared using chi-square test. To determine the correlation between quantitative variables, Pearson’s correlation coefficient test or Spearman’s correlation test was performed. For statistical analysis, SPSS version 23.0 for Windows (IBM, Armonk, New York, USA) was used.
4. Results
A total of 80 patients with prostate cancer were examined in this study. The mean age of the patients was 69.74 ± 8.12 years. Regarding the cause of referral, 78 (97.5%) patients showed increased PSA levels, 1 (1.2%) patient showed increased PSA levels with mediastinal lymphadenopathy, and 1 (1.2%) patient showed increased PSA levels with recurrent, biopsy-proven prostate cancer. The mean PSA level was 13.11 ± 27.46 ng/mL in the latest test.
Regarding the metastatic involvement of lymph nodes in different areas, cervical lymph node metastasis was found in 7 (8.8%) cases (two cases of single lymph node involvement and five cases of multiple lymph node involvement), abdominal lymph node metastasis was found in 19 cases (23.8%) (three cases of single-node involvement and 16 cases of multiple-node involvement), hilar/mediastinal lymph node metastasis was detected in 16 (20%) cases (three cases of single-node involvement and 13 cases of multiple-node involvement), and pelvic lymph node metastasis was found in 28 (35%) cases (two cases of single-node involvement and 26 cases of multiple-node involvement).
The 68Ga-PSMA uptake in the prostate itself was reported in 23 (28.8%) cases, which was focal in 13 (16.2%) cases and diffuse in 10 (12.5%) cases. Twenty-six patients showed bone metastasis (32.5%), including 6 (23.1%) cases of single bone metastasis and 20 (76.9%) cases of multiple bone metastases. Delayed 68Ga-PSMA PET/CT scan was performed for 15 (18.8%) patients, which did not indicate any avid lesions found in the initial PET/CT scan. The review of 68Ga-PSMA PET/CT images demonstrated that the mean SUVmax was 7.66 ± 5.68 in the involved cervical lymph nodes, 11.25 ± 14.47 in the abdominal lymph nodes, 13.44 ± 14.23 in the hilar/mediastinal lymph nodes, 13.24 ± 10.85 in the pelvic lymph nodes, and 21.03 ± 22.77 in bone metastasis.
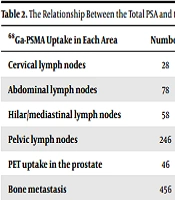
Based on the review of pathology reports, adenocarcinoma was diagnosed in 51 (63.8%) cases. The mean Gleason score was 7.33 ± 1.08. In this study, no significant correlation was observed between the Gleason score and the total PSA (correlation coefficient = 0.228). Comparison of the level of PSA between two subgroups with and without metastasis (Table 1) demonstrated a higher PSA level in patients with abdominal lymph node involvement, besides a slightly higher PSA level in patients with pelvic lymph node involvement. However, there was no significant association between the level of PSA and the extent of disease burden (Table 2).
| 68Ga-PSMA uptake in each area | Number | PSA level (metastasis group) | PSA level (non-metastasis group) | P-value |
|---|---|---|---|---|
| Cervical lymph nodes | 28 | 18.42 ± 5.40 | 12.59 ± 3.32 | 0.595 |
| Abdominal lymph nodes | 78 | 28.15 ± 9.97 | 8.42 ± 2.33 | 0.005 a |
| Hilar/mediastinal lymph nodes | 58 | 13.79 ± 3.38 | 12.93 ± 3.75 | 0.911 |
| Pelvic lymph nodes | 246 | 20.87 ± 6.98 | 8.92 ± 2.75 | 0.063 |
| PET uptake in the prostate | 46 | 15.86 ± 4.76 | 11.78 ± 3.94 | 0.537 |
| Bone metastasis | 456 | 20.83 ± 8.56 | 9.98 ± 2.53 | 0.110 |
The Relationship Between the Total PSA and Metastasis in Different Involved Areas
| 68Ga-PSMA uptake in each area | Number | PSA level in single-node involvement | PSA level in multiple-node involvement | P-value |
|---|---|---|---|---|
| Cervical lymph nodes | 28 | 16.60 ± 1.83 | 19.15 ± 7.78 | 0.852 |
| Abdominal lymph nodes | 78 | 15.59 ± 10.36 | 30.50 ± 11.69 | 0.600 |
| Hilar/mediastinal lymph nodes | 58 | 15.59 ± 0.79 | 16.61 ± 3.70 | 0.082 |
| Pelvic lymph nodes | 246 | 21.26 ± 20.97 | 20.85 ± 7.48 | 0.988 |
| PET uptake in the prostate | 46 | 4.10 ± 2.47 | 19.39 ± 5.96 | 0.080 |
| Bone metastasis | 456 | 7.69 ± 2.84 | 37.91 ± 18.47 | 0.080 |
The Relationship Between the Total PSA and the Extent of Metastatic Involvement in Different Areas
Regarding the association of the Gleason score with the pattern of metastatic involvement, higher Gleason scores were reported in patients with multiple rather than single metastatic involvement (Table 3).
| 68Ga-PSMA uptake in each area | Gleason score in single-node involvement | Gleason score in multiple-node involvement | P-value |
|---|---|---|---|
| Cervical lymph nodes | 7.00 ± 2.00 | 8.00 ± 0.25 | 0.379 |
| Abdominal lymph nodes | 8.00 ± 1.00 | 7.78 ± 1.59 | 0.789 |
| Hilar/mediastinal lymph nodes | 7.00 ± 1.00 | 7.56 ± 0.35 | 0.705 |
| Pelvic lymph nodes | 8.00 ± 1.00 | 7.48 ± 1.37 | 0.534 |
| PET uptake in the prostate | 7.50 ± 1.31 | 7.96 ± 0.97 | 0.294 |
| Bone metastasis | 7.00 ± 1.10 | 8.44 ± 1.01 | 0.004 a |
The Relationship Between the Gleason Score and the Extent of Lymph Node Involvement in Different Areas
Moreover, the PSA level (Table 4) and the Gleason score (Table 5) showed no significant correlations with the SUVmax values.
| 68Ga-PSMA uptake in each area | Coefficient (r) | P-value |
|---|---|---|
| Cervical lymph nodes | -0.381 | 0.456 |
| Abdominal lymph nodes | 0.101 | 0.732 |
| Hilar/mediastinal lymph nodes | 0.297 | 0.349 |
| Pelvic lymph nodes | 0.305 | 0.156 |
| PET uptake in the prostate | -0.183 | 0.883 |
| Bone metastasis | 0.357 | 0.112 |
The Relationship Between the Total PSA and the SUVmaxa
| 68Ga-PSMA uptake in each area | Coefficient (r) | P-value |
|---|---|---|
| Cervical lymph nodes | -0.200 | 0.704 |
| Abdominal lymph nodes | 0.330 | 0.294 |
| Hilar/mediastinal lymph nodes | -0.119 | 0.712 |
| Pelvic lymph nodes | 0.331 | 0.080 |
| PET uptake in the prostate | 0.790 | 0.420 |
| Bone metastasis | 0.315 | 0.177 |
The Relationship Between the Gleason Score and the SUVmaxa
5. Discussion
Various imaging modalities have been applied to evaluate the disease burden in prostate cancer patients. The 68Ga-PSMA PET/CT scan has recently received particular attention due to its high sensitivity, specificity, and accuracy. In this study, the value of 68Ga-PSMA PET/CT scan (and SUVmax) in assessing metastatic prostate cancer lesions and other tumor characteristics was investigated. Some significant findings were obtained in the present study. First, the relationship between the total PSA and metastatic disease burden was examined; higher PSA levels were significantly associated with a higher incidence of abdominal and pelvic lymph node metastasis. Secondly, although the assessment of total PSA could predict metastatic involvement of lymph nodes in the abdomen and pelvis, it was not well correlated with the number of involved lymph nodes (single or multiple). Thirdly, there was no significant correlation between the total serum PSA and the Gleason score (pathological grade) of prostate cancer, assuming that the total PSA cannot accurately represent the aggressiveness of prostate cancer. Fourthly, the value of the SUVmax index was not correlated with the Gleason score, assuming that the SUVmax value cannot provide an accurate representation of prostate cancer aggressiveness.
Based on the present results, there was no significant relationship between the SUVmax index and the total PSA level. On the other hand, there was a significant relationship between the Gleason score and increased 68Ga-PSMA uptake in prostate cancer, which was a predictable finding. Therefore, 68Ga-PSMA PET/CT is not a strong predictor of tumor invasiveness in prostate cancer. One reason for this finding may be the physical characteristics of 68Ga-PSMA radiotracer and differences in the emitted positron energy and range compared to the FDG radiotracer. Overall, the semi-quantitative parameters of 68Ga-PSMA PET are less reliable than those of 18F-FDG PET scan.
Additionally, there are other studies in the literature on the value of 68Ga-PSMA PET/CT scan in the evaluation of prostate cancer characteristics which reported inconsistent results. In a study by Kallur et al. (12), contrary to the present findings, 68Ga-PSMA PET/CT scan could detect extra-prostate metastatic lesions with 95% sensitivity at a predictive value of 98%. Besides, they predicted tumor progression in 100% of progressed cases; however, they reported a relatively low sensitivity for predicting response to treatment. The findings of 68Ga-PSMA PET/CT scan had no significant correlation with the PSA level. In another study by Demirci et al. (13), in contrast to the current study, there was a strong correlation between the SUVmax and tumor grade in patients, and the value of SUVmax was higher in high-grade cases. Moreover, in a study by Uprimny et al. (14), the correlation between the Gleason score and SUVmax was significant, and tumors with a Gleason score of 6 - 7 showed lower 68Ga-PSMA uptake compared to patients with a Gleason score > 7. Besides, in a study by Dadgar et al. (15), the progression of lesions was completely associated with an increase in the PSA level. In their study, the PET/CT technique could identify the majority of metastatic lesions in patients. Therefore, the lack of correlation between the SUVmax index and the pathological index (Gleason score) and the total PSA level reported in this study requires further investigations.
In conclusion, the SUVmax value in 68Ga-PSMA PET/CT scan provides a reliable predictor for neither the grade of prostate cancer, nor the metastatic status associated with cancer progression. The measurement of total PSA may predict metastasis to the abdominal and pelvic lymph nodes caused by prostate cancer.
The following limitations can be mentioned in this study. First, the sample size was limited, and therefore, the study did not have high power. Second, interpretation of PET/CT findings requires a high level of experience, and the diagnostician’s experience may be a confounding factor in the final assessment of 68Ga-PSMA PET/CT images
.jpg)