1. Background
Lumbar facet joints are one of the major contributors of chronic low-back pain, which can potentially lead to referred pain (1). Lumbar facet joint pain cannot be diagnosed by either physical assessments (2) or X-rays (3). A lumbar medial branch block is a diagnostic block for a lumbar facet joint pain diagnosis (4-7).
Years ago, physicians palpated anatomic landmarks for the insertion of the guide needle. More recently, fluoroscopic or computed tomography has been routinely used for guidance in our institution. Currently, slightly invasive and imaging-guided techniques have joined the tools used in pain management. The reason for their increased use is mainly due to their ease of use and high success rates in controlling chronic pain, which is of interest to practitioners (8, 9).
The use of ultrasound in pain medicine is rapidly growing, especially in various types of procedures for interventional pain management. Much of the recent research has investigated the procedures used under ultrasound guidance (10).
Fluoroscopy showing bone structure is a common practice, but cannot show the adjacent building. Ultrasound-guided techniques that show the communications between anatomical structures improve the accuracy of the procedure.
Lately, facet nerve blocks under ultrasound guidance have been done for chronic pain management. Because of the cost and lack of radiation exposure, the use of ultrasound guidance has been considered more beneficial (11, 12). The use of ultrasound in interventional pain management can also offer more advantages than that of conventional fluoroscopy (13, 14). Furthermore, ultrasound guidance can be used in various types of nerve blocks.
2. Objectives
The purposes of this study were to examine the relationship between bone anatomy and sonoanatomy using ultrasound guidance, and to evaluate the feasibility and success rates of ultrasound-guided lumbar medial branch nerve blocks.
3. Patients and Methods
This study was a prospective clinical trial (IRCT ID: IRCT201306168435N6). The study protocol was approved by the Shahid Beheshti University of Medical Science ethics committee. We evaluated 60 patients with chronic low back pain in the facet joint region who were referred to the pain clinics of Akhtar hospitals between 2011 and 2012. The patients with the following features were included: age > 18 years, symptoms of chronic low back pain (> 3 months), persistent back pain with or without pain radiating to the leg, focal lumbar tenderness and hyperextension pain, the absence of neural tube defects, contraindicated for lumbar surgery, an absence of radicular syndrome, and a failure to respond to traditional treatments. Patients were excluded if they had a malignancy, a coagulation disorder, or an allergy to the local anesthetic solutions. Furthermore, patients with behavioral problems, pregnancy, localized skin infection at the surgical site, spinal deformities, or patients who were uncooperative due to psychiatric disorders were also excluded.
All blocks were performed by one pain specialist. Patients in the prone position with lordosis support is destined to compensate. With a 7.5- to 12-MHz, 30-mm, broadband curved array transducer (HS-2600, Honda electronics Inc., Honda, Japan) targeted the lumbar vertebral joint with the longitudinal axis of the sacrum as measured by ultrasound was a turning point (15).
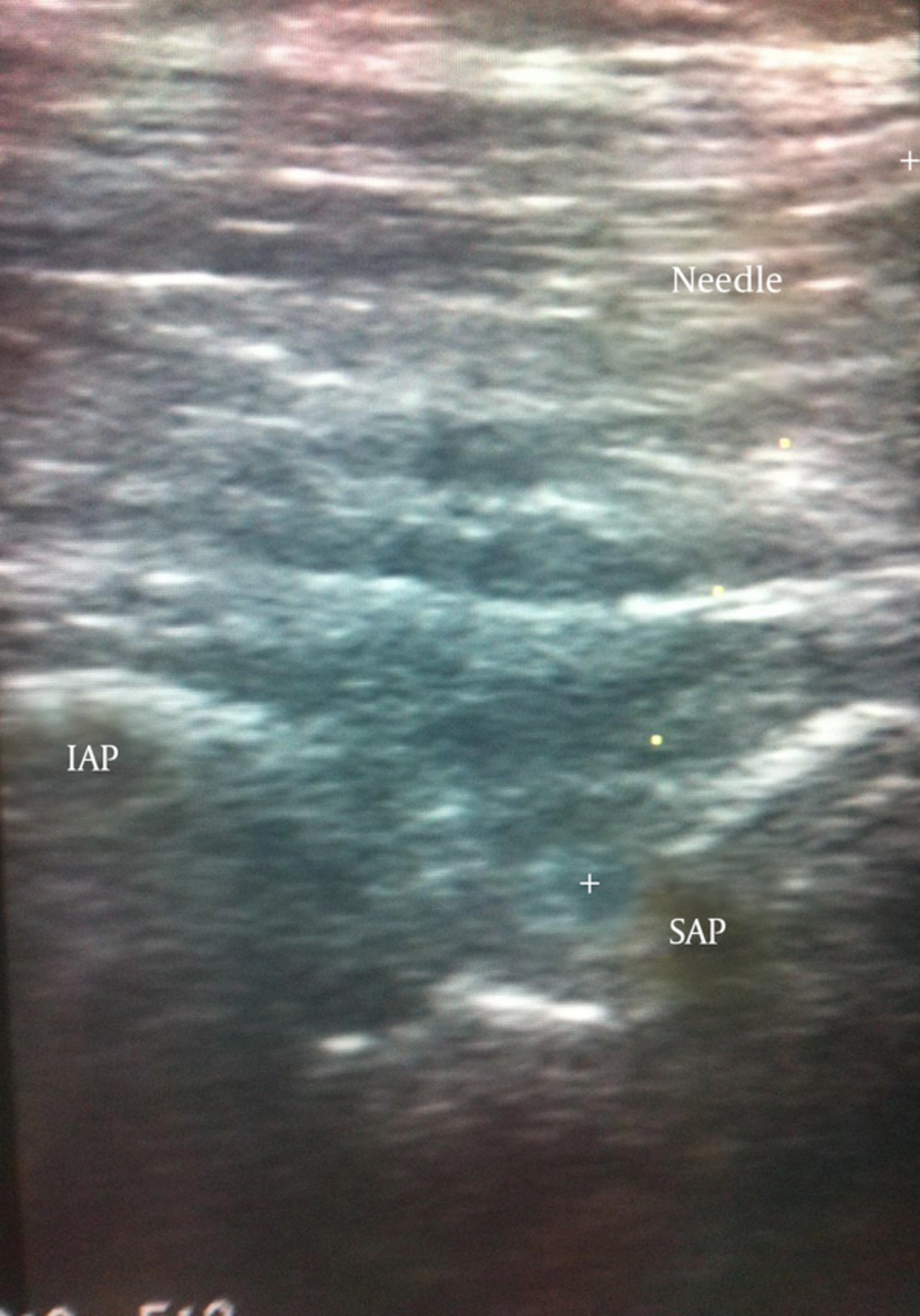
After identifying the target beads, to see the transverse and superior articular processes (SAP) and to obtain a view of the cross shaft became ultrasound probe to 90 degrees to show the distance from the cephalad margin of the adjacent groove side to the SAP (16), and the nearest skin surface was measured using an ultrasound caliper. Local anesthesia was performed with a 1% lidocaine injection (1 mL). A 21-gauge spinal needle with a length of 9 cm to the ultrasound disk and a 45- to 60-degree angle to the lateral and medial skin to its tip was inserted into the target bone is felt, driven. A brokerage ultrasound needle appropriate for the target site points out C-arm was performed to evaluate the correct insertion of the needle. The correct needle insertion at the target site was in accordance with the international guidelines of the spinal society forum. The correct needle insertion in the anterior posterior view was at the posterior edge of the SAP and above the Scotty dog's eye in the ultrasound diagonal view (15). If in view of the ultrasound needle was not put in the correct place, under the C-arm to guide the insertion needle has been modified, then the injection was carried out (Figures 1 and 2).
The combination of triamcinolone acetonide (40 mg) and 1% lidocaine (1 mL) at the L1-S1 levels on the right/left sides was injected for the treatment of lumbar facet joint pain.
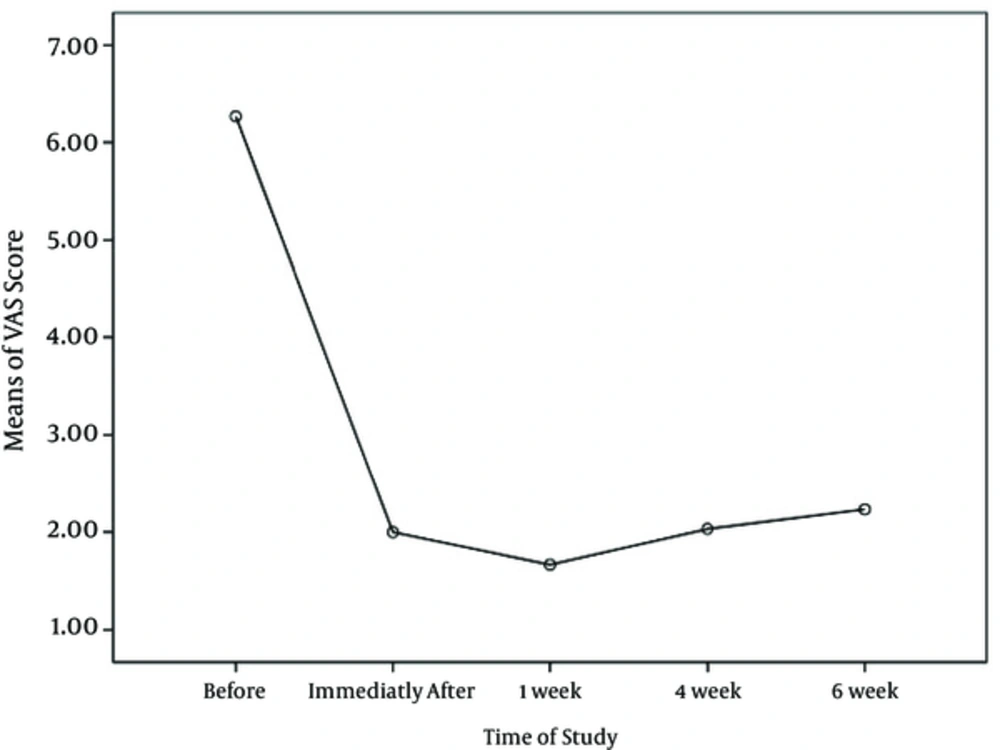
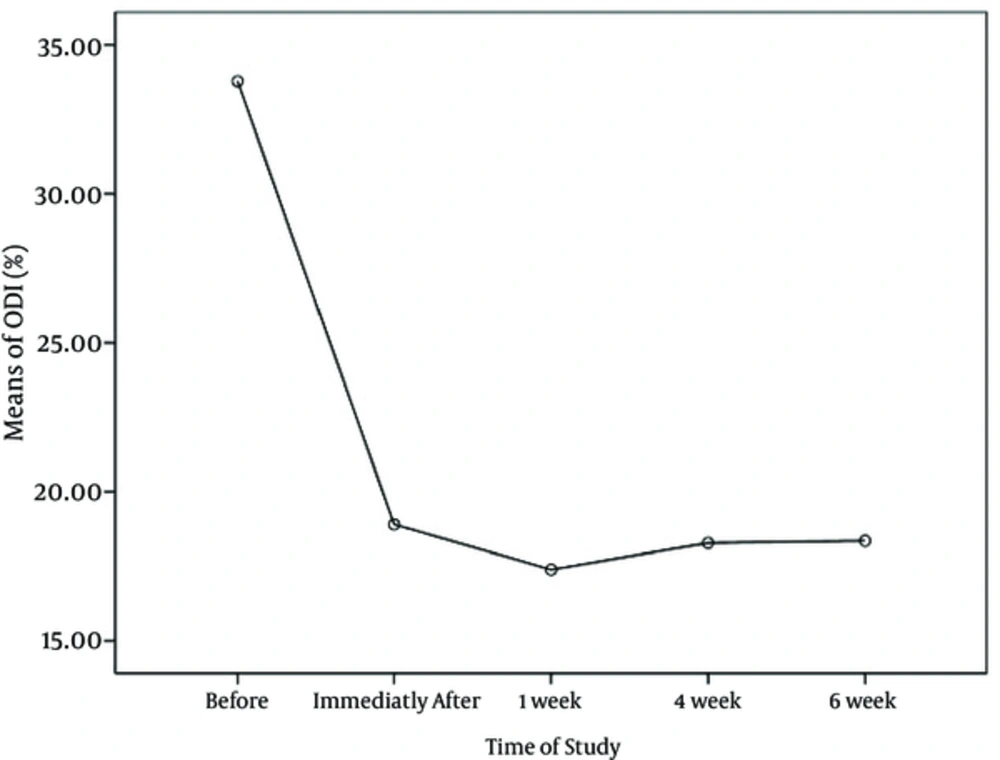
We recorded demographic characteristics including sex, age, body weight, height, and body mass index (BMI). Low back pain was assessed before, immediately after, and at 1 week, 4 weeks, and 6 weeks after the block by a visual analog scale (VAS; 0 = no pain; 10 = worst pain). The oswestry disability index (ODI) score was assessed before, immediately after, and at 1 week, 4 weeks, and 6 weeks after the block using a 5-point scale (0 = no disability; 5 = worst disability) (17). Patient satisfaction of pain control was assessed immediately after, and at 1 week, 4 weeks, and 6 weeks after the block using a 4-point scale (0 = poor satisfaction; 3 = excellent satisfaction). If the patient reported a VAS > 4 for pain, he/she received a anti-inflammatory drug (NSAID).
The procedure time from the beginning brokerage needle to the end of the injection was determined and recorded. The needle insertion, defined as the time from its insertion into the skin, was confirmed by fluoroscopic methods. If the needle tip was off-target and not visible by ultrasound, the attempt was considered a failure.
The sample size for this study had an 80% power. Data was evaluated with the statistical package for the social sciences (SPSS) software version 19 (SPSS Inc., Chicago, IL, USA). Normal distribution of samples was determined using Kolmogorov-Smirnov test. Descriptive parameters included frequency, percentage, mean, and standard deviation (SD). Comparisons of qualitative variables or quantitative variables without normal distribution were performed by the Wilcoxon and Friedman’s tests, while repeated measures analysis of variance (ANOVA) were performed for comparison of quantitative variables. A P value of < 0.05 was considered statistically significant.
4. Results
Thirty patients received ultrasound-guided medial branch blocks for lumbar facet joint pain. The mean age of the patients was 36.2 ± 10.8 (range: 18 - 58) years. Sixteen patients were men (53.3%) and 14 (46.7%) were women. The mean BMI was 24.7 ± 2.6 kg/m2. Ultrasound-guided medial branch blocks were performed in 11 patients (36.7%) for L3/4 and L4/5; 11 patients (36.7%) for L4/5 and L5/S1; 5 patients (16.7%) for L2/3 and L3/4; and 3 patients (10%) for L1/2 and L2/3. In terms of the practicality of cross-axis ultrasound to guide the needle in the 30 patients, all 89 medial branch blocks were performed. All needles were directed to the correct place, and the medial branches blocked included 30 for L3, 31 for L4, and 28 for L5. In 15 blocks, the needles were not confirmed in the longitudinal paravertebral view, then up and down along the groove in the cross-axis displays walked. Among the 89 blocks, 87 needles were placed in the correct position, resulting in a success rate of 98%. Only two needles needed minor adjustments after confirmation by the C-arm; these needles were slightly shifted laterally on the posterior side of the transverse process. The mean procedural time was 5.9 ± 1 minutes. The time required to insert the needle was 4 ± 1 minutes. There were no procedure-related complications. The mean VAS score was significantly reduced from 5 points (range: 4 - 8 points) preoperatively to 2.8 points (range: 1 - 4 points) at the final follow-up examination (P = 0.0001) (Figure 3).
The mean ODI was significantly reduced from 33.9 (range: 22 - 48) preoperatively to 18.3 (range: 10 - 26) at the final follow-up examination (P = 0.0001) (Figure 4).
Patient satisfaction was significantly improved from poor satisfaction immediately after the medial branch block to excellent satisfaction at the final follow-up examination (P = 0.0001).
Furthermore, analgesic requirements were significantly reduced at the final follow-up examination (P = 0.046).
5. Discussion
Lumbar facet joint pain cannot be diagnosed based on physical or radiology results alone (2, 3). A standard diagnostic block for facet joint pain is a medial branch block on the dorsal ramus of a spinal nerve that is adjacent to a facet joint, which is necessary to confirm the site of the pain (14).
To improve the precision of needle placements and reduce complication rates, fluoroscopic or computed tomography guidance has been considered compulsory (18). However, these techniques are associated with radiation exposure and higher costs (18). Alternatively, ultrasound guidance can be used for needle placement. Ultrasonography plays an important role in aiding regional nerve and peripheral-nerve blocks (19-22). Greher et al. reported a high success rate, clinical feasibility, and usefulness of ultrasound-guided lumbar medial branch blocks (11, 23). High-quality sonographic views depend on the technical expertise of the specialty pain physician and a specialized knowledge of radiology. The block used in this study was easy and it was visible in the joint. The needle’s cephalocaudal angle must be forward while the needle is in the groove, and the needle under the ultrasound waves is placed at an angle that is visible on the facade of the transverse axis. One problem of the cross-axis view concerns the direction of the needle at the target site since this view does not give the necessary information to the doctor. To increase the success rate of medial branch blocks, the needle tip is placed in the groove margin cephalad. In our experience, to obtain a cross profile interspinous space probe axis and move up and down where target site first seen and the ease of insertion needle in the margin of cephalad. In our experience, for the ease of insertion needle in the margin of cephalad, we move up and down probe axis where target site first seen. However, in view of the longitudinal axis of the needle tip approval often need to spend. Therefore, if the quality is poor, we set walk off the needle track in order to make it to the cephalad intervertebral foramen weaken and then to caudal in the walked bone. This movement in the cross axis view needle groove must be visible. In our study, we used a corticosteroid for the facet joint injections. Ultrasound can be used for corticosteroid injections for diagnostic blocks. The literature on the use of steroids in facet joint injections is controversial. Early trials failed to show improvements using facet joint injections with steroids. However, recent studies identified good outcome treatments with steroid injections (24, 25). Despite the suspicion surrounding steroid actions, some studies have subscribed to this treatment for clinical pain symptoms in their practices (26, 27).
We applied an injection volume of 1 mL. The optimal volume for a facet joint injection is still controversial, however, the usual amount for facet joints is 1 - 2 mL. In our study, during the short term follow up, pain relief was observed after facet joint injections, a finding confirmed by other studies (28). The results of facet joint injections can probably be improved with ultrasound guidance on certain patients to provide a better response to interventions. Most pain practitioners are largely used for facet joint injections. Also, when injections are performed under imaging guidance, complication rates are decreased and better outcomes are obtained (24, 29). Thus, the use of preciseness and safety equipment, such as ultrasound without radiation, have been highly requested. Ultrasound can produce improvements in clinical symptoms. In our study, patient satisfaction as well as good outcomes with significant differences in the degree of pain control and functional status improvement were obtained. Ultrasound is widely available, and in many patients, it is associated with a high degree of accuracy.
In conclusion, lumbar medial branch nerve blocks under ultrasound guidance can be used with a high rate of treatment success. Ultrasound is an invaluable tool for imaging the structure of soft tissues and bones, to guide needles, and to verify the progress of substances injected around the target. Moreover, it is a radiation-free method and ultrasound guidance can be used to replace traditional methods.