1. Introduction
Anomalous drainage of the inferior vena cava (IVC) into the left atrium is a rare congenital vascular disorder (1). It can occur with atrial septal defect (ASD), anomalous pulmonary venous drainage, and pulmonary arteriovenous fistula (2). This case report describes the computed tomography (CT) findings of a rare combination of drainage of the inferior vena cava associated with atrial septal defect and partial anomalous pulmonary venous return.
2. Case Presentation
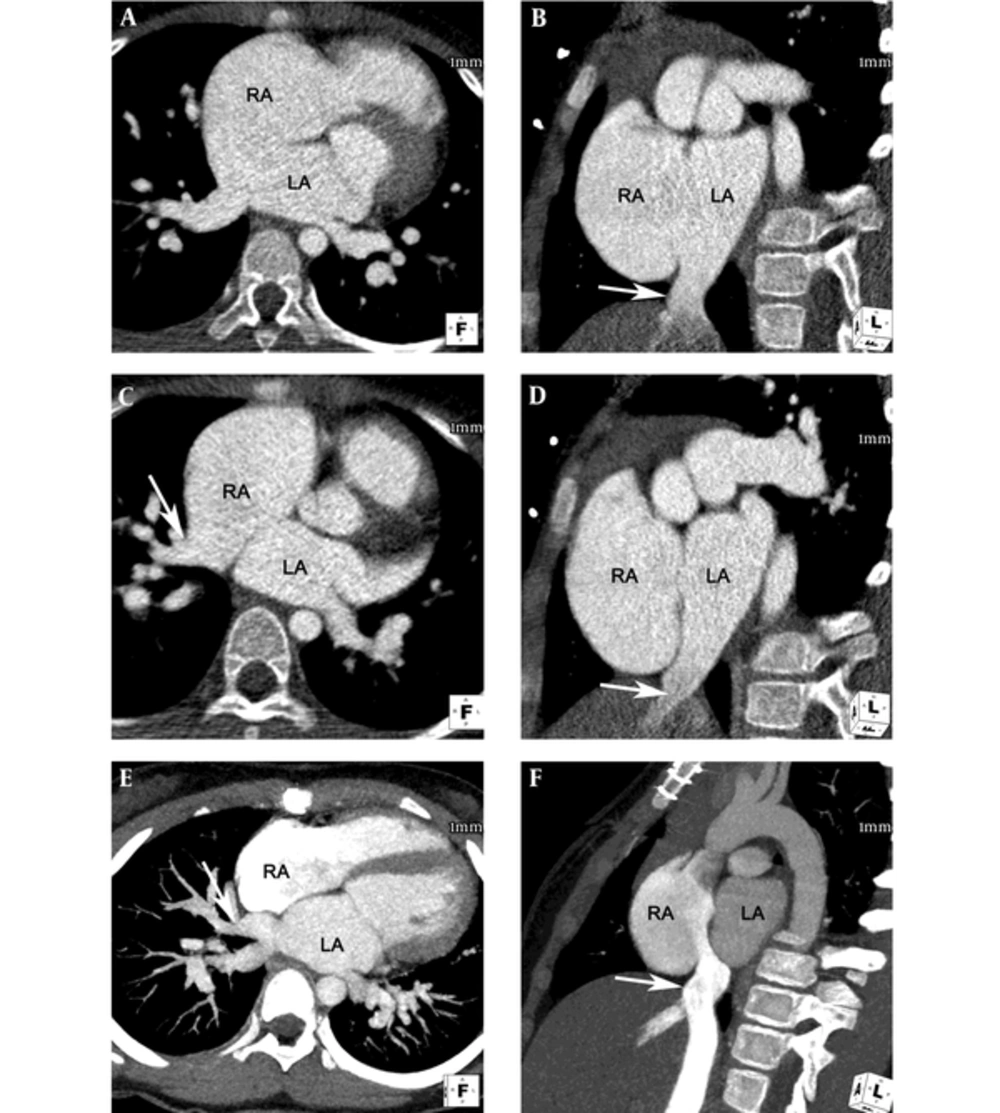
A 7-year-old girl was referred to our hospital for evaluation of palpitations and chest discomfort she had for 3 years. Clinically, there was no auscultatory abnormality. Her blood pressure was 90/60 mmHg and heart rate was 91 beats/min. Oxygen saturation was 98% at rest. An electrocardiogram (ECG) showed normal sinus rhythm and right ventricular hypertrophy. A chest radiograph revealed mild cardiomegaly with clear lung fields. Transthoracic echocardiography (TTE) revealed a large ASD with no posterior rim. The right ventricle was dilated, with a left-to-right shunt. However, there was no evidence of partial anomalous pulmonary venous return (PAPVR) or other vascular anomaly on TTE. To evaluate the combined anomaly, retrospective ECG-gated CT angiography was performed. CT angiography showed S, D, S segmental anatomy with atrioventricular and ventriculoarterial concordance. A large ASD secundum, 3.1 cm × 3.8 cm in size (Figure 1A and B) was noted, and the right superior pulmonary vein was seen draining into the right atrium, suggestive of PAPVR (Figure 1C). Abnormal drainage of the IVC into the left atrium was likewise suspected (Figure 1D). There was no evidence of pulmonary arteriovenous fistula or other cardiac anomalies.
Axial reformatted image (A) and short axis image (B) of retrospective electrocardiogram-gated computed tomography (CT) angiography showed large atrial septal defect (ASD, secundum type) with posterior rim deficiency. The size of the ASD was 3.1 × 3.8 cm. Axial reformatted image (C) showed right superior pulmonary vein (arrow) draining into the right atrium, suggestive of partial anomalous pulmonary venous return (PAPVR). Oblique sagittal reformatted image (D) and short axis image (B) demonstrate the inferior vena cava (IVC) (arrow) draining directly into the left atrium. Maximum intensity projection images of postoperative follow-up CT angiography show successful correction of the ASD, PAPVR, and anomalous drainage of the IVC into the left atrium. Note the superior pulmonary vein (arrow) draining into the left atrium (E) and the IVC (arrow) draining into the right atrium without significant stenosis (F).
The operation was conducted via median sternotomy. Cardiopulmonary bypass was established with bicaval cannulation, and the heart was arrested using antegrade cold blood cardioplegia. The right atrium was opened, which revealed a large ASD secundum, the left-ward shift of IVC, and PAPVR. The defect was closed with a patch of fresh autologous pericardium. The right superior pulmonary vein was redirected to the left atrium and the IVC was redirected to the right atrium. The postoperative course was uneventful. Prospective ECG-gated CT angiography performed 2 years after the operation revealed successful correction of ASD, PAPVR, and anomalous drainage of the IVC into the left atrium (Figure 1E and F).
3. Discussion
Anomalous drainage of the IVC into the left atrium is a rare congenital vascular disorder, first described by Gardner in 1955 (1). Only 19 cases with anomalous drainage of the IVC into the left atrium including our case have been reported in the English literature (Table 1). An ASD occurs with the condition in approximately 70% of the reported cases. Anomalous pulmonary venous drainage and pulmonary arteriovenous fistula may also be associated (2). Although two patients had a combined PAPVR and ASD similar to our patient, invasive angiography was used for diagnosis.
| No. | Author, Year | Gender/Age | Clinical Symptom | Resting O2 Saturation | Imaging Modality Used | Combined Cardiovascular Anomaly | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | Gardner, 1955 (1) | F/32 | DOE, cyanosis, clubbing, frequent miscarriages | Unknown | Chest X-ray | No | Sudden death |
| 2 | Meadows, 1961 (3) | M/37 | Cyanosis, clubbing, polycythemia, frequent headache | 82 | Chest X-ray, Invasive angiography | No | No treatment |
| 3 | Gallaher, 1963 (4) | M/26 | Cyanosis, clubbing, murmur | 94 | Chest X-ray, Invasive angiography | Secudum ASD with prominent Eustachian valve | Uneventful after operation |
| 4 | Black, 1964 (5) | F/30 | Cyanosis, clubbing, dyspnea, fatigue, lower limb edema | 70 | Chest X-ray, Invasive angiography | Pulmonary arteriovenous fistula | Death 47 days after operation due to sepsis |
| 5 | Guatam, 1968 (6) | F/34 | Dyspnea, cyanosis, clubbing, murmur | 89 | Chest X-ray, Invasive angiography | Secundum ASD | Uneventful after operation |
| 6 | Kim, 1971 (7) | M/12 | Minimal nail bed cyanosis, murmur | 93 | Chest X-ray, Invasive angiography | PDA, secundum ASD | Seizure, hypoxia with brain injury after operation; improved |
| 7 | Singh, 1976 (8) | M/6 | Murmur | 99 | Invasive angiography | Secundum ASD, sinus venosus ASD. PAPVR | Uneventful after operation |
| 8 | Richardson, 1979 (9) | Unknown/5 mon | Murmur | 92 | Invasive angiography | PFO | Uneventful after operation |
| 9 | Sanchez, 1986 (10) | M/6 | Murmur | 93 | Chest X-ray, Invasive angiography | TOF, ASD | Uneventful after operation |
| 10 | Sanchez, 1986 (10) | F/4 | Cyanosis, murmur | 95 | Chest X-ray, Echocardiography, Invasive angiography | ASD, PAPVR | Uneventful after operation |
| 11 | Lamb, 1987 (11) | M/3 | Cyanosis, clubbing | 89 | Invasive angiography | Secundum ASD, TAPVR | Uneventful after operation |
| 12 | Mayers, 1987 (12) | M/41 | Cyanosis, clubbing, hypoxemia, one episode of exertion, headache | 89 | Echocardiography, MRI, Invasive angiography | Secundum ASD, PFO | Uneventful after operation |
| 13 | Cabrera, 1994 (13) | F/3 | Respiratory distress, murmur | 90 | Chest X-ray, Echocardiography, Invasive angiography | ASD | Uneventful after operation |
| 14 | Genoni, 1999 (14) | F/7 | DOE, cyanosis, clubbing | 72 | Echocardiography, Invasive angiography | No | Uneventful after operation |
| 15 | Burri, 2003 (15) | F/54 | DOE, cyanosis, clubbing, murmur, ankle edema, palpitation, cerebellar deficit | 81 | Echocardiography, MRI, Invasive angiography | Secundum ASD, coronary sinus draining into left atrium | Uneventful after operation |
| 16 | AL-Ammouri, 2010 (16) | F/32 | Dyspnea, polycythemia, fatigue, cyanosis, clubbing, arthritis | 80 | Echocardiography, Invasive angiography | ASD | Uneventful after operation |
| 17 | Aliter, 2011 (2) | F/17 | Cyanosis, clubbing | 95 | Echocardiography, CT, Invasive angiography | Secundum ASD | Uneventful after operation |
| 18 | Basquin, 2013 (17) | F/4 | Dyspnea, cyanosis | unknown | Echocardiography, CT, Invasive angiography | ASD | Uneventful after operation |
| 19 | Present case | F/7 | Palpitation, chest discomfort | 98 | Chest X-ray, Echocardiography, CT | Secundum ASD, PAPVR | Uneventful after operation |
Abbreviations: ASD, atrial septal defect; DOE, dyspnea on exertion; O2, oxygen; PAPVR, partial anomalous pulmonary venous return; PDA, patent ductus arteriosus; PFO, patent foramen ovale; TAPVR, total anomalous pulmonary venous return; TOF, tetralogy of Fallot.
Anomalous drainage of the IVC into the left atrium results from persistence of the right valve of the sinus venosus. In the embryo, the sinus venosus receives the cardinal, umbilical, and vitelline veins. The sinus venosus communicates with the primitive atrium via an orifice that has a right and left valve. As the heart develops, the IVC formed then drains into the sinus venosus, which normally migrates to the right of the midline. The right valve of the sinus venosus usually atrophies, leaving only the crista terminalis, Eustachian valve, and Thebesian valves (Figure 2). If the right sinus venosus valve fails to regress and fuses with the superior part of the septum secundum, the IVC will drain into the left atrium (2, 5, 18).
Schema of the development of venous valves in 5th week of pregnancy (A) and fetal stage (B) [modified from (18)].
We herein present a case of a 7-year-old girl with ASD combined with PAPVR and drainage of the IVC into the left atrium. In our case, the TTE failed to demonstrate the anomalous IVC drainage into the left atrium and the PAPVR in a patient with ASD because of the limited echocardiographic window. The diagnosis was eventually established using CT angiography. CT angiography can be useful for early detection of this complex anomaly and for proper surgical planning. To our knowledge, CT images of this rare combination and postoperative follow-up CT have not been reported in English literature.

![Schema of the development of venous valves in 5th week of pregnancy (A) and fetal stage (B) [modified from (<a href="#A13878REF18">18</a>)]. Schema of the development of venous valves in 5th week of pregnancy (A) and fetal stage (B) [modified from (<a href="#A13878REF18">18</a>)].](https://services.brieflands.com/cdn/serve/3170b/aea49bac407ca05f52bcb635b2656fb100ac8a09/iranjradiol-15-2-13878-i002-preview-preview.webp)