1. Introduction
The concomitant occurrence of cerebral aneurysms and arteriovenous malformations (AVMs) is often detected both within the AVM nidus and the proximal feeding vessels. Today, there are no standard guidelines for managing this condition. The treatments reported include gamma knife surgery, endovascular treatment, combined modality staging, and hybrid surgical treatment. However, flow diverters (FDs) have shown limited effectiveness in treating flow-related cerebral aneurysms associated with AVMs (1-3).
The Flow Redirection Endoluminal Device (FRED, MicroVention, Aliso Viejo, CA, USA) is a dual-layered FD that has shown promise in the treatment of large, wide-necked intracranial aneurysms. Unique to the FRED is its design of only 16 wires in the outer-stent portion. This design feature allows for improved maneuverability, reduced friction, and superior anchoring deployment in the parent vessel when compared to other FDs (4). However, there have been reports of the FRED failing to deploy in some patients. Specifically, the FRED did not expand as expected at points of vessel tortuosity (5). Another study reported that the stent strut of the FRED could not be penetrated (6). This study documents the first case where the middle part of the FRED failed to open during the treatment of an AVM flow-related aneurysm. The issue was addressed using the stent strut technique for coiling as a salvage treatment.
2. Case Presentation
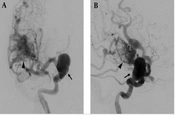
A 64-year-old woman, with no prior systemic disease, was admitted to our emergency department after losing consciousness due to a motorcycle accident. Upon arrival, she regained consciousness with a Glasgow Coma Scale score of E4V4-5M6 and showed no neurological deficits. A brain computed tomography (CT) scan revealed a subarachnoid hemorrhage (SAH) in the right frontal lobe, likely due to trauma, and incidentally discovered large aneurysms in the bilateral dorsal internal carotid artery (ICA) and an arteriovenous malformation (AVM) in the right temporal lobe. Further investigation with magnetic resonance imaging and angiography showed a right temporal AVM measuring approximately 2.5 cm, with superficial venous drainage through the veins of Trolard and Labbé and deep venous drainage through the middle cerebral vein and the basal vein of Rosenthal. The AVM was graded two on the Spetzler-Martin Scale. Additionally, a giant, multilobulated flow-related aneurysm measuring 2.5 × 1.4 cm in the right supraclinoid ICA and a saccular bilobed aneurysm measuring 1.1 × 0.9 cm in the left supraclinoid ICA were observed (Figure 1).
A 64-year-old woman experienced a brief loss of consciousness following a head injury. A subsequent brain CT scan revealed a subarachnoid hemorrhage (SAH). Additionally, large aneurysms were incidentally discovered in the bilateral dorsal internal carotid arteries, along with an arteriovenous malformation (AVM) in the right temporal lobe. The angiogram of the right internal carotid artery with anteroposterior (A) and lateral (B) views showed right temporal AVM (arrowhead) and right supraclinoid ICA aneurysm (arrow).
Given the potential for significant morbidity associated with surgical treatment for large aneurysms, as suggested by current literature, alternatives such as endovascular treatment are often explored. In this case, both aneurysms were large with wide necks, making standalone coil embolization unfeasible due to the risk of migration. As a result, a combined approach using an FD and coils was deemed appropriate. A right fronto-temporal craniotomy was performed for AVM excision after consulting with a neurosurgeon, and a staged endovascular treatment for the right giant ICA aneurysm was carried out one month post-discharge.
First endovascular intervention
All procedures were conducted under general anesthesia. The dual-catheter technique was employed for coil embolization. The Seldinger technique was also utilized to puncture the bilateral common femoral artery for FRED deployment. A 6-Fr shuttle (Cook Medical, Bloomington, IN, USA) was introduced through the right femoral artery, followed by the insertion of a 5-Fr Sofia intermediate catheter (MicroVention). Subsequently, a Headway 27 microcatheter (MicroVention) was extended over the aneurysm from the right ICA to the right middle cerebral artery. Due to the prolapse of the Headway 27 microcatheter into the large aneurysm sac, a Hyperglide balloon catheter (Medtronic Neurovascular, Irvine, CA, USA) was used to straighten the route for FRED. A 5 × 32-mm FRED was selected based on the preoperative diagnostic angiogram measurements.
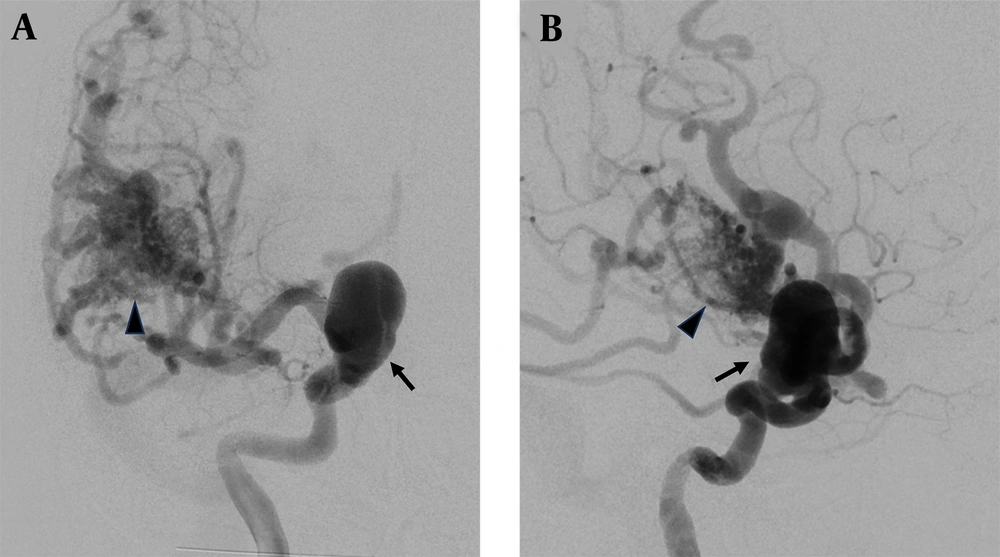
During the angiography, it was observed that the microcatheter was being pulled back from the distal end, and the FRED was expanding from the distal to the proximal end. However, it did not open in the middle segment. Initially, we believed that fully unsheathing the microcatheter would lead to its opening, but it remained closed in the middle section at the aneurysm neck, causing severe stenosis. Despite performing percutaneous transluminal angioplasty (PTA), the Headway 17 microcatheter could not progress past the stenotic site, even after multiple attempts with a black guidewire having a 0.014-inch shaft, 0.014-inch tip, and 0.018-inch outer diameter (Asahi Chikai Intecc, Nagoya, Japan) (Figure 2).
We observed the guidewire attempting to maneuver between the FRED and the vascular endothelium. However, due to the tight space, we were ultimately unable to secure a successful passage. No immediate neurological complications were observed; accordingly, we temporarily left the unopened FRED in place. The unsuccessful FRED procedure for the right-side aneurysm was deemed a treatment failure, and as a result, no antiplatelet therapy was administered. Since the stent could spontaneously open, we planned another endovascular treatment for the left supraclinoid ICA aneurysm using a Surpass Evolve FD (Stryker Neurovascular, Fremont, CA, USA), which was successfully combined with coil embolization. Two months later, we performed a salvage treatment for the right-side aneurysm.
Second salvage endovascular intervention
During the three-month follow-up after the initial endovascular treatment, no complications were reported. Postoperative follow-up angiography of the right ICA, after the unsuccessful FRED deployment, showed that blood flow continued through the aneurysm without any evidence of contrast agent retention within the aneurysm, and it extended to the distal intracranial region. As a result, we planned further bailout management with total right ICA coil trapping following an initial balloon occlusion test. The procedure was carried out under general anesthesia, and the right common femoral artery was punctured using the Seldinger technique with a 6-Fr shuttle. Next, we introduced a 6-Fr Neuron 070 guiding catheter (Penumbra, Alameda, CA, USA) and a Headway 17 microcatheter. On this occasion, the combination of the Headway 17 microcatheter and a 0.014-inch soft guidewire was able to successfully navigate past the stenotic site.
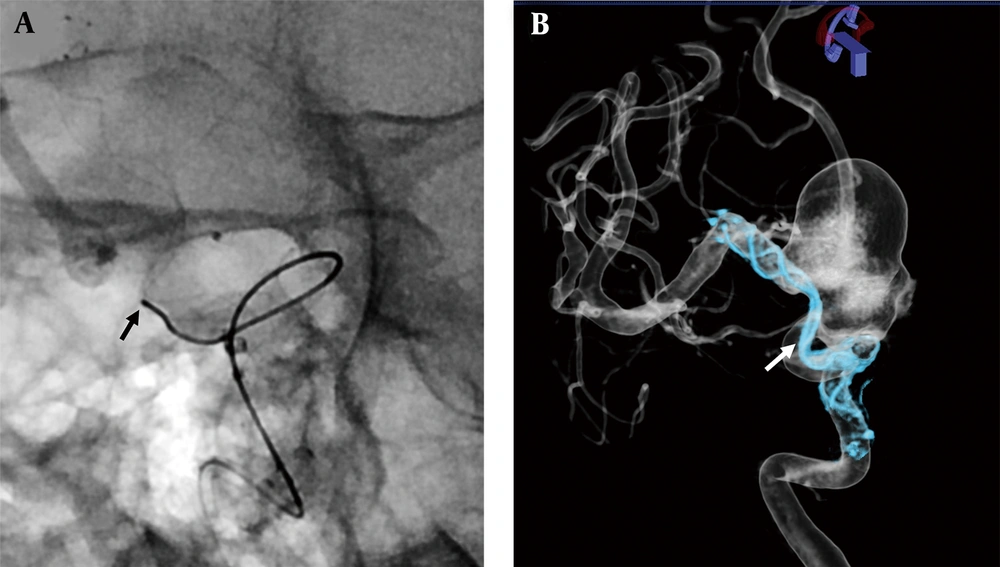
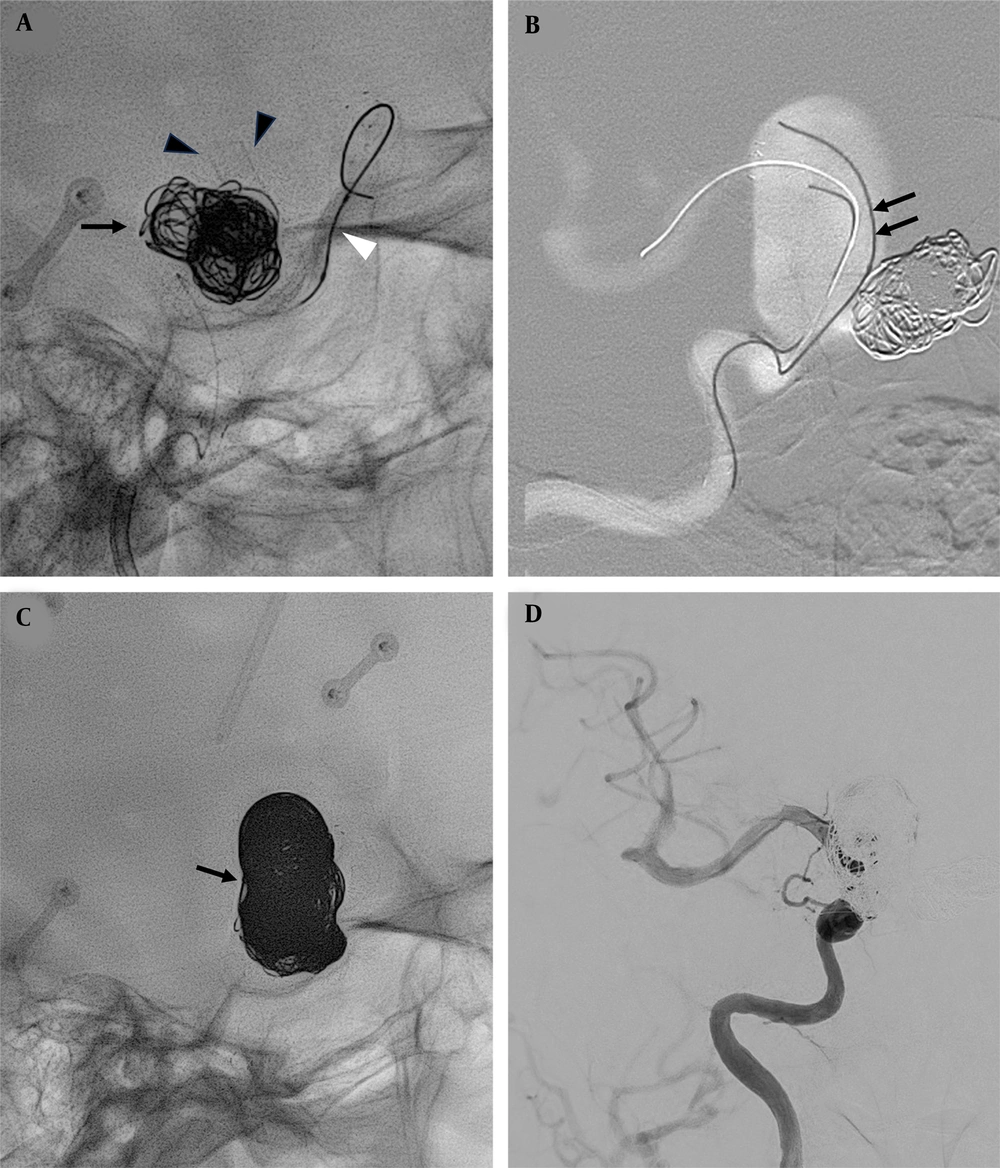
The PTA procedure was conducted using a Euphora semicompliant balloon dilatation catheter (Medtronic Neurovascular) sized between 1.5 and 2.5 mm. However, the FRED did not fully expand, resulting in poor wall apposition in the neck post-PTA. We then attempted coiling with the stent strut technique. Trapping was carried out from the left femoral artery puncture using the combo Headway Duo 156 (MicroVention), with the 0.014-inch soft Chikai guidewire successfully extending over the strut into the aneurysm sac. Coil embolization was then performed using a MicroPlex Coil System (MicroVention) and Micrusphere Microcoil (Codman Neurovascular, Raynham, MA, USA), deploying a total of 12 coils (size, 6–24 mm; length, 585 cm). This led to the near-total obliteration of the aneurysm sac and preservation of the right ICA without significant stenosis due to the coil mass effect (Figure 3). The entire procedure was carried out smoothly, and no immediate complications were observed during the six-month follow-up period.
A, Percutaneous transluminal angioplasty (PTA) was performed with a Euphora semicompliant balloon dilatation catheter (white arrowhead) after passing the guidewire over the stenotic site of the Flow Redirection Endoluminal Device (FRED). The aneurysm in the left supraclinoid internal carotid artery (ICA) was successfully embolized using a Surpass Evolve flow diverter (FD) (arrowheads) and coils (arrow); B, Successful advancing into the aneurysm sac over the strut with Headway Duo 156 microcatheter and 0.014-inch soft Chikai guidewire (arrows); C and D, Embolization was successfully performed on the right supraclinoid ICA aneurysm using 12 coils (arrow).
3. Discussion
Intracranial aneurysms are frequently associated with AVM. They are classified into three types: intranidal, flow-related, and unrelated to AVM. It has been reported that intranidal and flow-related aneurysms have a higher incidence of rupture compared to those that are unrelated to the AVM nidus (7-10). To the best of our knowledge, case reports involving the Pipeline Flex device (Medtronic Neurovascular) are limited (1, 3) and no study has reported the use of FREDs in this situation. Also, no consensus currently exists concerning the treatment of intracranial aneurysms associated with AVM (1).
The FRED is a self-expanding stent made of nickel titanium. It features a single-wire, braided, compliant, closed-cell paired-stent design. It consists of a low-porosity inner mesh with higher pore attenuation (48 nitinol wires) and a high-porosity outer stent (16 nitinol wires). It has a higher radial force that facilitates easier deployment. Numerous studies have shown the safety and effectiveness of FRED treatment in wide-necked, spindle-shaped, dissecting, or giant intracranial aneurysms. The O’Kelly–Marotta grading scale (OKM) C–D occlusion rates range from 84.6% to 89.3%, with an average morbidity of 3.9%, an average mortality of 1.4%, and low rates of complications, including ischemic, thrombotic, stenotic, or hemorrhagic events (1.5 - 6%) (4).
Although Waqas et al. (4) reported technical complications, including migration of the device and changes in the device morphology from “fish-mouthing” or “foreshortening” with a low incidence of approximately 3.6%, Suyama et al. (5) subsequently addressed cases where FREDs failed, with S-shaped curves or oversizing of more than 2 mm in the parent vessel. This shortcoming was resolved by retrieving the FRED converted to the pipeline or using more distal open-and-drag maneuvers. We incorrectly determined the size of the FRED to be 5.5 mm based on the preoperative diagnostic angiogram. On reviewing the angiogram image, we observed that the parent ICA diameter was reduced after AVM excision. The failed deployment caused by the tortuosity of the parent vessel in our case is consistent with that reported by Suyama et al. (5). The complication of FRED where the middle part remains unopened while both the distal and proximal ends are fully opened has not been documented. We propose that the unique “stent-within-stent” design of FRED could exert significant constraint force and cause self-twitching in highly tortuous vessels, despite its usual benefits of reduced friction and ease of deployment.
Matsuda et al. (6) designed a study using the brain and intracranial vessels from a human cadaver to compare the new low-profile visualized intraluminal support stent and the FRED. The conclusion was that it is impossible to employ a trans-cell approach with a Headway Duo microcatheter for FRED, a finding that contradicts our own. Although the manufacturer does not provide data on the relationship between FRED oversizing and the treated artery, we hypothesized that FRED shares similar characteristics with the Pipeline Embolization Device (Medtronic Neurovascular). Oversizing is understood to result in decreased metal coverage and increased porosity proximal to the twisting point (11). As demonstrated, it is applicable by using a Headway Duo microcatheter for the trans-cell approach for an unopened FRED.
Our study showed significant changes in the diameter of the parent vessel following the excision of an AVM. We also found that a vessel with a double or more tortuous curve significantly impacted the unsuccessful deployment of the FRED. Therefore, careful consideration is required when using FRED. This is a limitation of our case report. Future prospective studies should focus on unopened technical complications and compare the performance of FRED with other FDs. Additionally, in vitro studies examining the metal coverage of FRED in devices of different diameters are necessary.
In conclusion, the guidelines for managing aneurysms related to AVMs are not yet well-defined. It is important to note that the diameter of the parent vessel of an aneurysm undergoes changes following the excision of an AVM. Therefore, a re-evaluation of the diagnostic angiogram is necessary to determine the appropriate size for the FRED. The trans-cell method, utilizing a Headway Duo 156 microcatheter, could be considered a successful treatment strategy for salvaging an unopened FRED stent used for treating brain aneurysms.