1. Introduction
Uterine leiomyoma is the most common benign gynecological tumor in women of menstrual age, and uterine artery embolization (UAE) has been increasingly utilized to manage symptomatic leiomyomas (1). Numerous randomized controlled trials and observational studies support its use as a uterine-sparing procedure for women who may consider future fertility (2).
The internal iliac artery, from which the uterine artery normally originates, is well known for its prominent collateral formation when proximal blood flow is compromised due to various causes, such as atherosclerotic occlusion, surgical ligation, and others.
This report presents a brief case review of successful UAE for uterine leiomyoma via collaterals from the lumbar artery in a case where the ipsilateral internal iliac artery was compromised due to previous kidney transplantation.
2. Case Presentation
A 44-year-old female patient presented with complaints of menorrhagia, dysmenorrhea, abdominal discomfort, and frequent voiding. She had a history of kidney transplantation 5 years ago due to end-stage renal disease caused by IgA nephropathy.
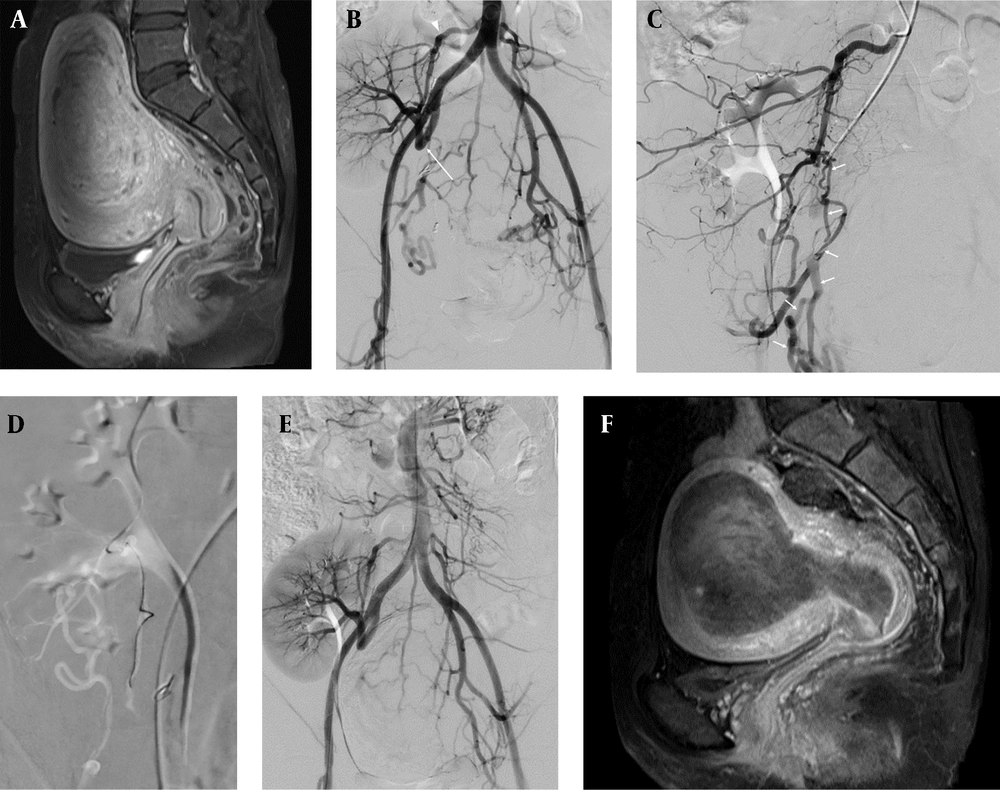
The laboratory results showed a normal hemoglobin level of 12.8 g/dL. Contrast-enhanced pelvic magnetic resonance imaging (MRI) revealed multiple submucosal and intramural uterine leiomyomas, with a maximal diameter of 9.4 cm (Figure 1A).
For UAE, the right common femoral artery was punctured under ultrasound guidance using an 18-gauge Seldinger needle, and a 6 French vascular sheath was inserted. Abdominal aortography using a 5 French pigtail catheter (Cook, Inc., Bloomington, IN, USA) revealed multiple hypervascular stains in the uterus, suggestive of uterine leiomyomas. While the left uterine artery originated normally from the ipsilateral internal iliac artery, the right internal iliac artery had been ligated just proximal to the bifurcation of the anterior and posterior divisions and was anastomosed with the graft renal artery using the end-to-end method. The distal portion of the right internal iliac artery, including the uterine artery, was opacified via collateral circulation (Figure 1B).
A 44-year-old female patient with multiple submucosal and intramural uterine leiomyomas, who was a candidate for uterine artery embolization and had a previous history of kidney transplantation. A, the initial contrast enhanced magnetic resonance imaging (MRI) showed a well-circumscribed enhancing mass in the uterine cavity, with maximal diameter of 9.4 cm; B, abdominal aortogram showed ligated right internal iliac artery (long arrow) and hypertrophied right lumbar artery (arrowhead); C, selective right lumbar arteriogram showed opacification of right uterine artery via tortuous collaterals (arrows); D, successful catheterization of the right uterine artery was achieved using a 2.4 French microcatheter and 0.016” guide wire; E, final abdominal aortogram showed completely resolved previous hypervascular staining from the uterus; F, follow-up contrast enhanced MRI after 3 months showed extensive hemorrhagic necrosis and size reduction of the previous uterine leiomyoma.
First, the left uterine artery was selected using a 5 French Robert’s uterine catheter (RUC, Jungsung Medical, Seongnam, South Korea), and selective embolization was performed using 3 vials of microspheres (Embospheres; Biosphere Medical, Rockland, MA USA, 500 - 700 µm and 710 - 1000 µm) and 2 vials of PVA particles (Contour, 500 - 710 µm, Boston Scientific, Natick, MA, USA) via a 2.4 French microcatheter (Progreat; Terumo, Japan).
For right UAE, selective right external iliac arteriography was performed to identify any collateral supply to the uterus. No visualized collateral supply was found. The hypertrophied right lumbar artery, originating from the distal abdominal aorta, was selected using a 5 French Robert’s uterine catheter, and selective angiography was performed. The right uterine artery was visualized through a tortuous and fine connection from the lumbar artery (Figure 1C). Using a 2.4 French microcatheter (Progreat) and a 0.016” guide wire (Meister; Asahi Intecc Co. Ltd., Japan), successful access to the right uterine artery was achieved. This was performed as distally as possible, passing through the narrow and abnormal connection between the lumbar and right uterine arteries. Any risky branches were carefully evaluated using digital subtraction angiography before embolization. The embolic materials were injected slowly, with extreme care taken to prevent reflux into the proximal portions. Finally, selective embolization was successfully performed (Figure 1D).
The final angiogram showed complete resolution of the previous hypervascular staining in the uterus (Figure 1E). A follow-up contrast-enhanced MRI taken 3 months after the procedure showed that the uterine leiomyomas had lost contrast enhancement, with a mild decrease in size (Figure 1F). The patient remained symptom-free at a 2-year follow-up via outpatient clinic visits.
3. Discussion
Here, we present a rare case of successful embolization of uterine leiomyoma through collateral vessels from the ipsilateral lumbar artery in a patient with a compromised internal iliac artery due to a previous kidney transplantation. Al-Dhawi et al. reported a similar case of UAE in a patient with prior ipsilateral internal iliac artery ligation due to postpartum hemorrhage, with collateral formation from the ipsilateral external iliac artery (3).
The uterus is well known for its abundant arterial supply. Even in cases with a patent internal iliac artery, leiomyomas can be supplied by extra-uterine collaterals from ovarian arteries and extragonadal arteries, such as the inferior mesenteric artery (IMA) or lumbar artery (4, 5). Pelage et al. reported that in about 5 - 10% of cases, even when both uterine arteries are normal, additional supply to the fibroid may come from other sources, such as ovarian arteries (5). According to their study, the risk factors for ovarian artery collateral supply to the uterus include prior pelvic surgery, tubo-ovarian pathology, or large fundal fibroids (4, 5). Several case reports have described IMA embolization for uterine fibroid embolization, often due to adhesions between the uterus and large bowel caused by pelvic inflammatory disease, such as endometriosis, trauma (including surgical), or neoplasms (4, 6). Chang et al. also reported a higher incidence of IMA collaterals in patients with adenomyosis compared to those with fibroids alone (4).
There are a few reports regarding repeated UAE in patients who had previously undergone embolization or ligation of the uterine artery. Dixon et al. reported a case of a 47-year-old patient with a history of UAE using polyvinyl alcohol and coils 15 years ago. Repeated embolization was performed for uterine leiomyoma via de novo recruitment of collateral supply from the IMA (7). According to a case report by Heaston et al., a 22-year-old female had bilateral surgical ligation of the internal iliac arteries and total abdominal hysterectomy due to postpartum hemorrhage. Selective embolization was performed for collaterals from the external iliac artery due to persistent vaginal bleeding (8). Donmez et al. also reported a case of intractable postpartum hemorrhage despite bilateral internal iliac artery ligation, where embolization of a uterine artery pseudoaneurysm was performed via an external iliac artery collateral route (9).
Limited studies have dealt with changes in uterine perfusion after kidney transplantation, although there have been some studies regarding penile vascularity and sexual dysfunction after kidney transplantation (10). In terms of pelvic organ perfusion, we could presume that the consequence of kidney transplantation might be similar to that of iliac artery occlusion. According to Burchell’s report on hemodynamic changes after internal iliac artery ligation in 45 patients, the ligation altered the pathways and reversed the direction of flow in some arteries but did not prevent flow to any pelvic arteries (11). The collateral route can be variable and depends on the site of occlusion and dominant hemodynamic flow.
In conclusion, UAE can be successfully performed even in cases of proximal internal iliac artery ligation via a collateral pathway. This may require thorough examination of angiography to evaluate collateral pathways.