1. Introduction
The heel spur, also known as the plantar calcaneal spur (PCS), manifests as a bony protrusion originating from the calcaneal tuberosity. This anatomical feature is notably associated with plantar heel pain, a prevalent concern among adults. The consequential pain can be incapacitating, significantly impacting daily activities and functionality (1, 2). The hallmark manifestation of the calcaneal spur is talalgia, widely recognized as pain in the heel region (3). In a comprehensive study encompassing both normal subjects and patients afflicted with plantar heel pain, the occurrence of the calcaneal spur was observed in 15.5% of the former (62 out of 400) and 65.9% of the latter (54 out of 82), respectively (4). Notably, around half of the patients diagnosed with plantar fasciitis, who concurrently exhibit plantar heel pain, are also identified to possess heel spurs (5). This data underscores the substantial prevalence of calcaneal spur among those experiencing plantar heel pain, signifying its clinical relevance in this specific context.
The study revealed intriguing findings regarding the length of calcaneal spurs among the participants, with a mean length of 3.86 ± 3.36 mm and a range spanning from 0 to 12.2 mm (6). The etiology of heel spurs is complex, with theories suggesting a combination of factors, including repetitive stress, inflammation, adaptive response to biomechanical forces, and genetic predisposition (1). Heel spurs are commonly observed in patients with heel pain, but their classification based on size is not well established (7). The average size of calcaneal spurs generally ranges from 3 to 5 mm; however, they can vary widely, with spurs larger than 10 mm being less common (8). One study noted that spurs larger than 20 mm are uncommon, with a reported frequency of approximately 1% to 5% in a population of patients with plantar fasciitis or heel pain (8). Cases of spurs larger than 25 mm are even rarer and have been documented in a few case reports (9).
The following discourse will present a unique instance of a 31 mm heel spur. This remarkable size defies conventional norms and offers valuable insights into the formation and implications of heel spurs.
2. Case Presentation
The patient is a 38-year-old male presenting with a prolonged history of plantar fasciitis and heel spur discomfort. He reports experiencing these symptoms for several years. Additionally, the affected foot has a congenital shortening of a few centimeters, though this condition was asymptomatic before the onset of his current complaints. Several years ago, the patient initially sought medical attention due to persistent heel pain and was administered an unidentified injection to the affected area, which provided temporary relief. However, over the last three months, the pain has significantly intensified, becoming more debilitating. The chief complaint is heel pain, exacerbated in the mornings and after rest periods. The pain diminishes with activity but remains persistent. On a pain scale of 1 to 10, the patient rates it at 8, experiencing more discomfort when walking barefoot.
Clinical examination reveals a prominent bony projection upon palpation, and X-ray demonstrates a 34 mm × 17 mm heel spur at the plantar calcaneal tuberosity. The patient has no evident limitations in mobility or physical activity. He is employed at the Red Crescent and stands for prolonged durations as part of his job responsibilities. Besides the history of an injection to the foot for heel pain several years ago, the patient has no known history of significant trauma or other foot-related issues. He noted swelling in the affected foot concurrent with the pain, alongside a positive response to non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief.
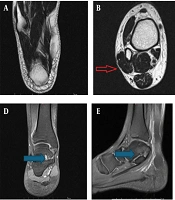
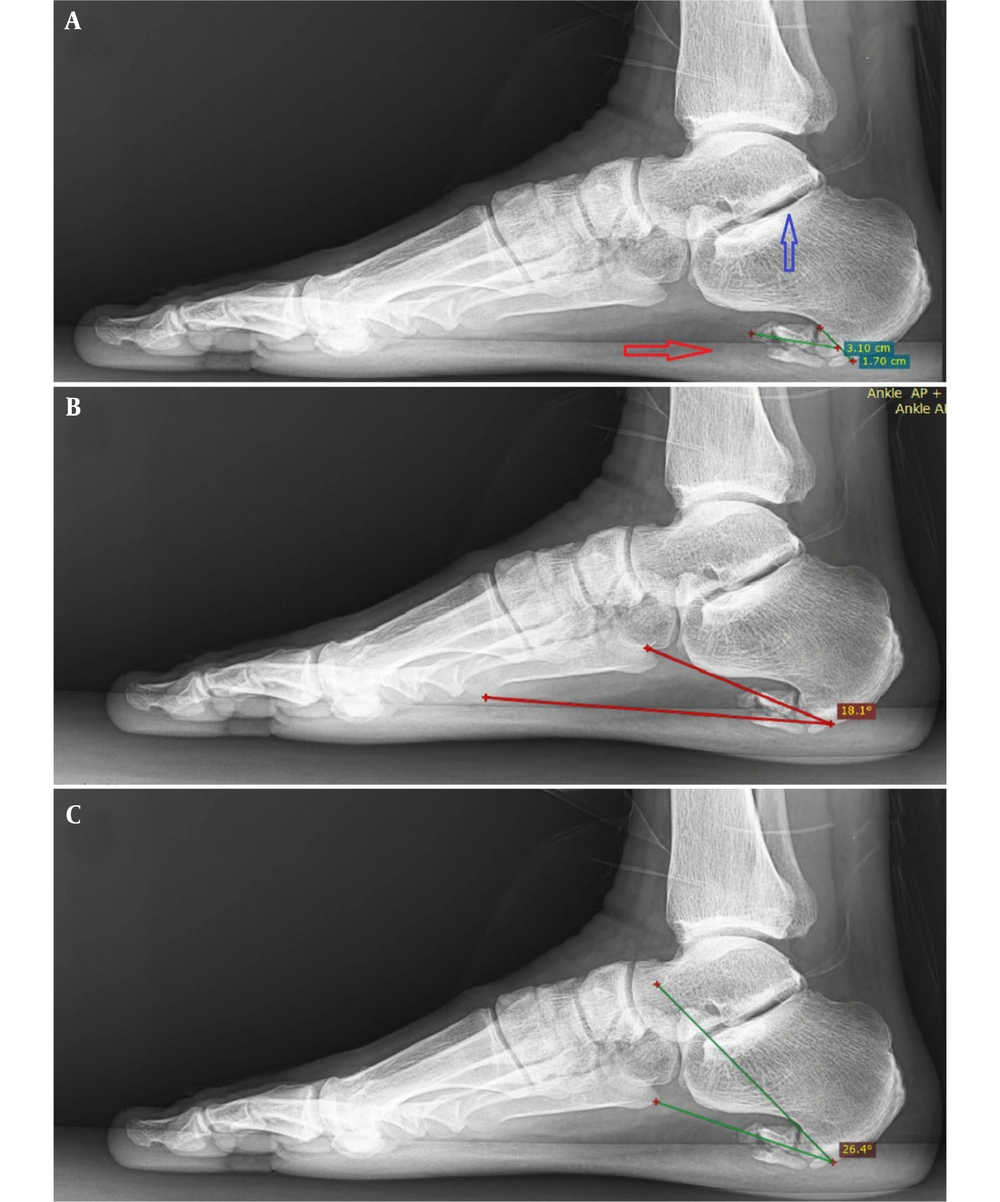
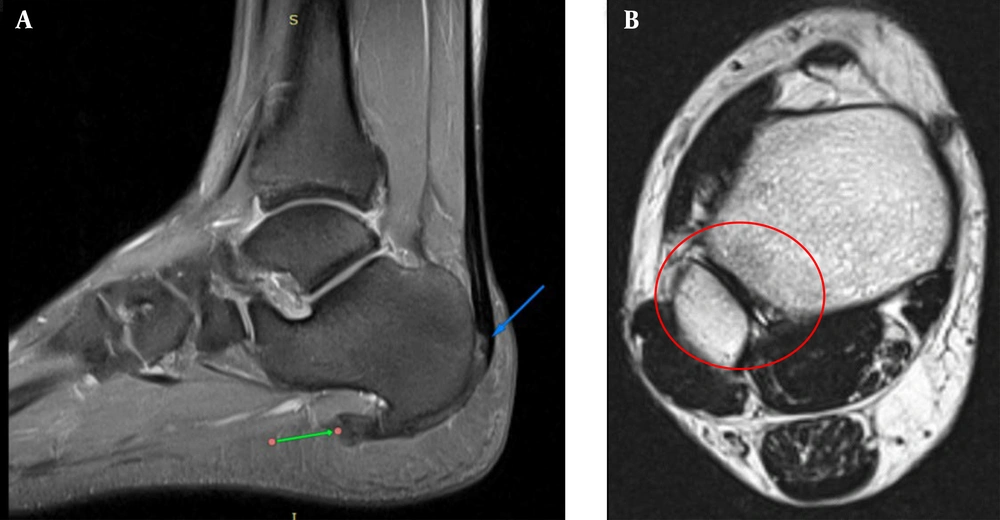
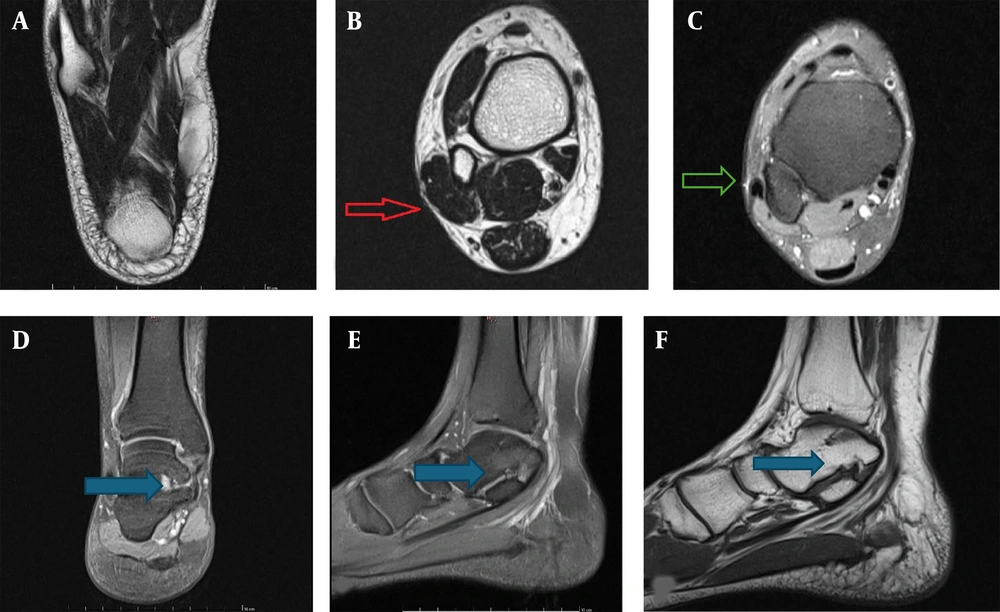
X-ray studies confirmed the presence of a sizable fragmented heel spur at the plantar calcaneal tuberosity, measuring 31 × 17 mm, coupled with degenerative changes at the lateral talar facet (Figure 1). The slope of the calcaneal spur is measured at 26.4 degrees (type B), and the calcaneal pitch angle is 18 degrees. Ankle MRI revealed multiple findings, including an extraosseous talocalcaneal coalition with subtle degenerative changes, hypertrophic posterior tibialis tendinosis with insertional interstitial tearing at the medial navicular bone, chronic subluxation of peroneus tendons with lateralization through a torn superior peroneal retinaculum with a large accessory muscle as peroneus quadratus. Additionally, there is a split tendon tear in both the peroneus longus and brevis tendons, along with a dysplastic calcaneus showing a rounded contour of the superior process. There is also evidence of Achilles tendon enthesopathy with trace retrocalcaneal bursitis. A large calcaneal spur with enthesophytic changes involving the origin of the plantar aponeurosis muscle atrophy is seen (Figures 2 - 4).
A 38-year-old male complained of heel pain for three months and a history of calcaneal spur some years ago. Lateral foot X-Ray analysis. A, Fragmented heel spurs (indicated by red arrow) and degenerative changes at the lateral talar facet (indicated by blue arrow); B, Plantar calcaneal spur (PCS) slope is 18.1 degrees (type B) (red angle); C, The calcaneal pitch angle is 26.4 degrees (green angle).
A, These proton density fat-saturated (PDFS) MRI sequences sagittal views show a large calcaneal spur (green arrow) with dysplastic calcaneus with a rounded contour to the superior process with Achilles tendon enthesopathy (blue arrow), tendinitis, and trace retrocalcaneal bursitis; B, Axial T2-weighted non-fat-saturated sequence shows no usual shape of the tibia and fibula with dysplastic changes to these bones (red circle).
A, This T2 axial view represents normal muscles with no atrophy; B, An accessory muscle in the peroneus compartment (red arrow) as peroneus quadratus; C, On axial PDFS, chronic subluxation of peroneus tendons with lateralization through a torn superior peroneal retinaculum with a large accessory muscle (green arrow). D-F, On coronal and sagittal PDFS, sagittal T2W: An extra-articular non-osseous talocalcaneal coalition (blue arrow).
The patient has experienced relief with pharmacologic intervention using NSAIDs. However, specific treatment and management beyond this modality have not yet been initiated. The patient is scheduled for further evaluation and discussion of potential treatment options, considering the persistent and worsening nature of the symptoms.
3. Discussion
This rare case of a 31 mm calcaneal spur emphasizes the diagnostic and therapeutic complexities associated with large heel spurs. Although commonly seen in patients with plantar heel pain, the role of heel spur size in symptom severity remains unclear. Plantar fasciitis, often the underlying pathology, is present in over two-thirds of symptomatic individuals seeking care for heel pain. Our patient also presented with tarsal coalition, an abnormal fusion between two or more tarsal bones, which is a known contributor to flatfoot and biomechanical alterations. These coalitions may be fibrous, cartilaginous, or bony in nature and can lead to restricted joint motion and subsequent structural changes, including plantar fasciitis and spur formation (10-12). Non-osseous coalitions may be subtle radiographically, requiring MRI for definitive diagnosis. In this case, only secondary degenerative changes were apparent on plain radiographs. MRI revealed multiple abnormalities, including peroneal tendon tears, posterior tibial tendon involvement, ligament thickening, and plantar fascia inflammation, likely a cumulative result of altered biomechanics and chronic traction due to the coalition. The patient also had a congenital or early developmental transposition of the peroneal tendon and superior peroneal retinaculum tear, further contributing to functional instability. While the exact cause of the large spur remains uncertain, the combination of congenital anomalies and mechanical dysfunction provides a plausible explanation.
Studies suggest a potential relationship between calcaneal spur dimensions and symptom severity. One study found that 80% of plantar fasciitis patients with morning stiffness also had heel spurs, with a significant correlation between spur length and pain (6). Other research found associations between spur angle, length, and pain intensity (13). However, some studies report no such correlation (14). Notably, spurs measuring 10 - 12 mm or more are considered large and are relatively uncommon. One study documented just 6 cases with spurs > 10 mm among 109 patients (15). A few rare case reports describe spurs exceeding 25 mm, including one measuring 35 mm (16). These findings support the idea that unusually large spurs may warrant more aggressive treatment.
Conservative management remains the first line, particularly in cases involving tarsal coalitions, with surgery reserved for persistent or severe symptoms. Factors such as obesity, female gender, and biomechanical stress have been linked to spur formation (17, 18). Emerging non-invasive treatments like percutaneous needle electrolysis (PNE), extracorporeal shock wave therapy (ESWT), low-dose radiation, and high-intensity laser therapy (HILT) have demonstrated potential benefits in treating plantar fasciitis, especially in refractory or complex cases involving large spurs (19-22).
In conclusion, this case illustrates the clinical and radiologic complexity of a rare, unusually large 31 mm calcaneal spur in the presence of underlying structural anomalies, including tarsal coalition and dysplastic calcaneus. While the precise relationship between spur size and pain remains uncertain, this case highlights the value of advanced imaging and comprehensive biomechanical evaluation in patients with chronic heel pain. Given the rarity of similar reports, more documented cases are needed to better understand the implications and management of large calcaneal spurs.