1. Introduction
Computed tomography (CT)-guided percutaneous biopsy is widely recognized as a safe and cost-effective diagnostic procedure, particularly for abdominal lesions. As a minimally invasive alternative to surgical biopsy, it has become a cornerstone in modern diagnostic approaches. However, the technique is not without limitations, as anatomical structures along the needle trajectory can pose significant challenges, increasing procedural complexity and the risk of collateral injury. Abdominal procedures, in particular, demand careful planning to navigate critical structures such as the intestines, blood vessels, and vital organs. Transorgan traversal is associated with organ-specific risks. For instance, a trans-splenic approach may increase the risk of intraperitoneal hemorrhage due to the spleen’s rich vascularity, while a transpancreatic route raises concern for traumatic pancreatitis (1). Gastrointestinal tract transgression during biopsy has been linked to contamination of both the biopsy specimen and sterile procedural field, thereby increasing the risk of infection (2, 3). Furthermore, serious complications requiring further intervention, such as abscess formation, gastrointestinal perforation, and hemorrhage requiring transcatheter arterial embolization, have also been reported in the literature (4, 5).
To address these challenges, various strategies and technical modifications have been proposed. Among them, the use of a coaxial needle without a stylet to displace intestinal structures offers a promising solution to reduce the risk of injury during biopsy. This report presents a case of CT-guided abdominal biopsy, highlighting the innovative application of this technique and discussing its safety, feasibility, and clinical implications. The present study aimed to demonstrate the potential of the stylet-free coaxial needle technique as a simple and effective method for anatomical displacement during biopsies involving challenging anatomical conditions.
2. Case Presentation
An 85-year-old male with a medical history of traumatic brain injury, hypertension, type II diabetes mellitus, and hyperlipidemia presented with chest tightness. A chest X-ray revealed a lesion in the left upper lobe of the lung. Subsequent chest CT imaging identified a 6 × 6 × 8.5 cm mass in the left upper lobe, which was subsequently confirmed to be carcinoma via ultrasound-guided biopsy. Additionally, multiple small hypodense lesions were observed in the liver, raising suspicion for metastasis. Further evaluation with liver MRI confirmed the absence of liver metastases; however, a small protruding hypovascular tumor was incidentally noted in the left kidney. To determine whether the renal lesion represented a metastatic deposit or a second primary malignancy, a CT-guided biopsy was scheduled.
3. Technique Description
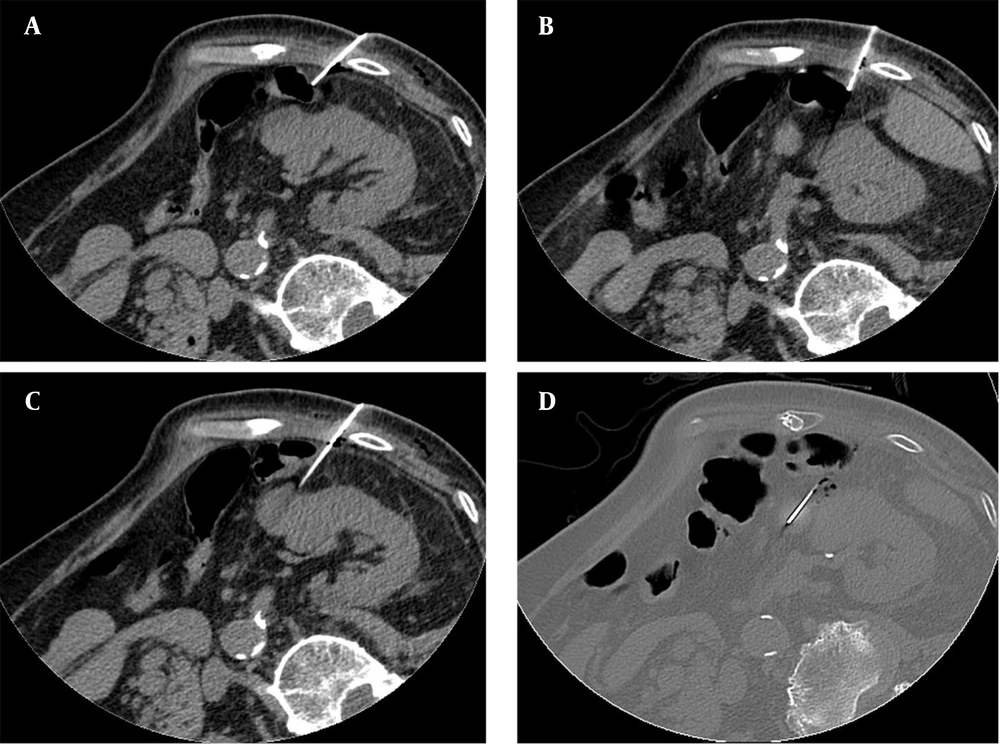
While a posterior retroperitoneal route is generally favored for renal biopsies, the target lesion in this case was located on the anterior aspect of the kidney, making the transabdominal path the most direct and practical route for tissue acquisition. The biopsy was performed with the patient positioned in the right lateral decubitus position, using a TEMNO™ biopsy gun (Merit Medical Systems, Inc., South Jordan, UT, USA) with a 19-gauge 10 cm coaxial needle and a 20-gauge 15 cm biopsy gun. The needle was inserted through the right abdominal wall. During the procedure, the needle path was obstructed by a segment of the colon. After advancing the coaxial needle into the abdominal wall, the stylet was removed, leaving only the blunt, rounded tip of the coaxial needle exposed. The coaxial needle was then carefully advanced to gradually displace the obstructing colonic segment. After several attempts, the colon was successfully repositioned, allowing the biopsy to be performed without incident (Figure 1).
An 85-year-old patient with a small protruding hypovascular tumor of the left kidney that was indicated for CT-guided biopsy. Axial CT image reconstructed with 5 mm slice thickness and 5 mm interval, from source images acquired at 2.5 mm thickness. A, A segment of the bowel was obstructing the planned needle trajectory; B and C, To address this, the stylet was removed from the coaxial needle, and the coaxial needle was carefully advanced to gradually displace the obstructing bowel. Throughout the procedure, CT imaging was utilized to monitor the position of the bowel and ensure that no injury occurred; D, After several attempts, the bowel was successfully displaced, allowing for the safe advancement of the needle into the target tissue.
Post-procedural CT imaging revealed a small amount of hemoperitoneum, with no evidence of pneumoperitoneum. Considering the potential risk of occult bowel perforation, the patient was kept nil per os (NPO) for 24 hours following the procedure. Close clinical monitoring was conducted to observe for any signs of peritonitis or gastrointestinal complications. The patient remained clinically stable with no evidence of delayed complications during follow-up. Throughout the procedure, a total of 59 CT image acquisition sequences were performed. Each sequence consisted of nine axial slices acquired at 5 mm intervals, several of which were dedicated to confirming the successful displacement of the bowel away from the needle path. Histopathological analysis of the biopsy specimen confirmed a diagnosis of poorly differentiated carcinoma.
4. Discussion
The CT-guided percutaneous biopsy remains an essential tool in modern diagnostic medicine, offering a minimally invasive and cost-effective method for obtaining pathological diagnoses. This case demonstrates the successful application of a coaxial needle without a stylet for the displacement of obstructing anatomical structures, such as the colon, during an abdominal biopsy.
When applying this technique, determining the optimal timing for stylet removal is crucial. In our case, the stylet was retained during the initial advancement to provide sufficient rigidity and precise control, allowing smoother and more efficient passage through the skin and abdominal wall. This also helped minimize the number of CT scans required for trajectory adjustment. The stylet was only removed once the coaxial needle had entered the abdominal wall and approached adjacent anatomical structures. Thereafter, the blunt tip of the outer cannula alone was used under CT guidance to gently displace non-target tissues.
Various techniques have been proposed to reduce the risk of injury along the needle trajectory during CT-guided biopsy, including positioning of the patient (6), the use of saline injection to displace anatomical structures, and the application of specialized needles (7). Among these, the blunt-tip stylet technique shares similarities with our approach, as both aim to mitigate injury by eliminating the sharp needle tip (8, 9). However, a key distinction lies in the implementation: Our method directly utilizes the coaxial needle to engage with anatomical structures, whereas the blunt-tip stylet requires the insertion of an additional device.
While several techniques for bowel displacement during CT-guided interventions have been described, our case is, to our knowledge, the first to report the use of a stylet-free coaxial needle alone to displace obstructing bowel loops without the aid of additional devices or fluids. However, we also noted that similar approaches have been described in the context of CT-guided radiofrequency ablation (RFA). Ginat et al. reported the use of probe torquing to increase the separation between renal tumors and adjacent bowel during RFA. While the clinical goal in both reports was to prevent bowel injury by creating a safe working space, there are key methodological differences (10). The RFA technique primarily manipulated the kidney itself to reposition it away from the bowel. In particular, kidney displacement was achieved by applying leverage to the ablation probe at the skin entry site, effectively shifting the kidney posteriorly, rather than directly displacing the bowel.
We propose that the primary advantage of using a coaxial needle is its improved accessibility and versatility. In situations where obstructions are encountered during the biopsy, the coaxial needle allows for direct manipulation and displacement of anatomical structures without the need for supplementary instruments. This streamlines the procedure and reduces potential interruptions. Besides, compared to the blunt-tip stylet, which is limited to specific gauge options, the standard coaxial needle offers a wider range of gauge sizes, allowing it to better accommodate the requirements of different targets (9). However, a notable limitation is that, compared to the blunt-tip stylet, the coaxial needle retains relatively sharper components, which may pose a residual risk of tissue injury. To mitigate this risk, careful pre-procedural assessment and prudent intra-procedural decision-making are essential. For instance, if pre-procedural imaging reveals signs suggestive of bowel inflammation, the bowel wall may be more fragile and less amenable to displacement, rendering this technique inappropriate. Similarly, if significant resistance is encountered during the manipulation of adjacent structures, the procedure should be reconsidered or modified accordingly. Post-procedurally, closely monitoring for potential complications remains crucial. In our case, the patient was kept NPO for 24 hours following the procedure, with close clinical observation to detect any signs of complications.
Lastly, we would like to address the potential impact of this technique on pathological specimen quality. The absence of a stylet might theoretically increase the chance of sample contamination if non-target tissue is inadvertently introduced during repositioning. Furthermore, repeated needle repositioning, which is sometimes necessary in anatomically complex cases, has been associated with an elevated risk of specimen contamination (11). To ensure accurate targeting and preserve specimen quality, the stylet was retained during the initial advancement of the coaxial needle into the target zone to provide sufficient rigidity and precise control, thereby minimizing trajectory deviation and maintaining procedural accuracy. Interestingly, temporary removal of the stylet is also practiced in certain bone biopsy techniques, particularly after traversing cortical bone, suggesting that stylet-free advancement may not adversely affect diagnostic specimen quality in certain contexts. Although the specimen obtained in our case was diagnostic, further studies are warranted to evaluate the diagnostic yield of stylet-free approaches in a broader range of clinical scenarios. Further validation through additional clinical experience and case studies is necessary to establish the safety and efficacy of this technique.
In conclusion, this case highlights the use of the stylet-free coaxial needle technique as a safe and efficient method for CT-guided biopsy. While promising, further studies are needed to confirm its safety and broader applicability in challenging cases.