1. Introduction
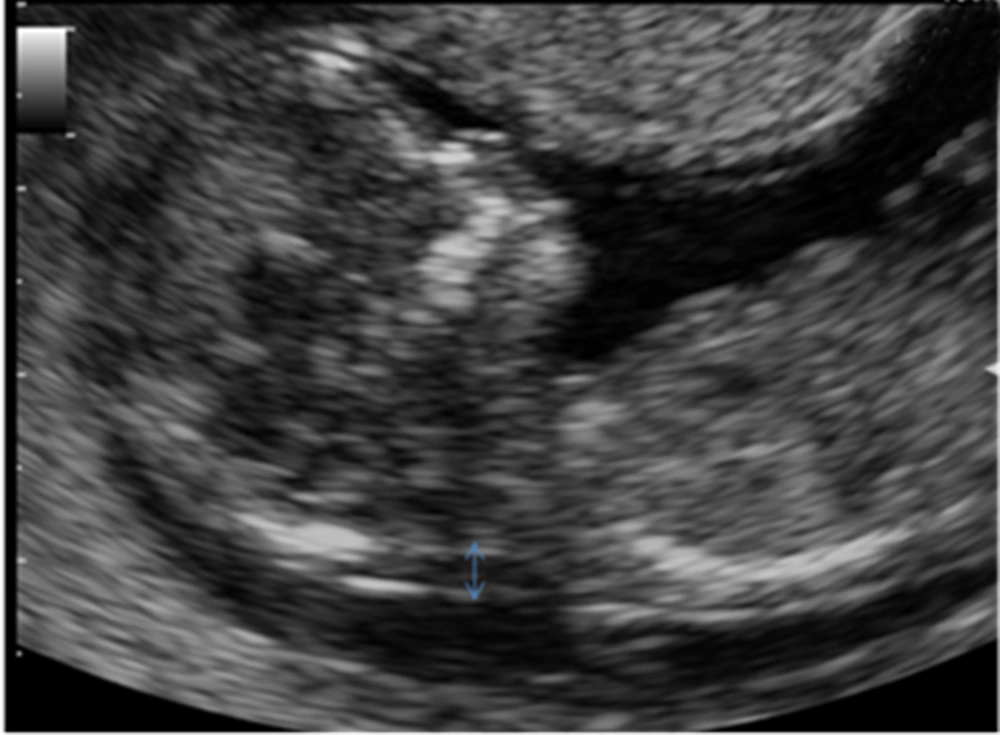
Fetal nuchal translucency (NT) refers to the sonographic appearance of subcutaneous edema in the fetal neck measured according to the fetal medicine foundation (FMF) guidelines. NT is defined as the maximal thickness of the sonolucent zone (fluid accumulation) between the inner aspect of the fetal skin and the outer aspect of the soft tissue overlying the cervical spine or the occipital bone (Figure 1). To avoid false negative or positive results, the fetus should be in a neutral position, with the head in line with the spine. During the scan, more than one measurement must be taken and the maximum one that meets the criteria should be considered.
For this report, the outcome of 703 pregnancies presenting at Royan Institute after intra cytoplasmic sperm injection (ICSI) between the years 2008 and 2009 were reviewed. First trimester measurements of NT were performed during the routine first trimester screening for 856 fetuses. A total of 12 fetuses with an increased NT (NT ≥ 3) were considered for further investigation. In the follow-up ultrasounds, six out of 12 fetuses showed no anomalies and the result of amniocentesis (karyotype), fetal echocardiography and triple test or double test (the biochemical markers of pregnancy-associated plasma protein-A and free β-human chorionic gonadotropin) were also normal. Six healthy neonates were followed during their first and second year by routine pediatrician visits and the mental, physical or motor developmental delay was not observed in any of the cases and their functions were normal.
All sonographic measurements were carried out by an expert radiologist with 10 years of experience and FMF certification in the measurement of NT. Images were saved and re-checked by another expert radiologist. Increased NT can be associated with a high incidence rate of chromosomal and non-chromosomal abnormalities. However, in nine studies that have addressed the issue of pediatric long-term follow-up of chromosomally and anatomically normal fetuses with increased NT, this measurement was suggested to be an indefinite indicator for the evaluation of fetal anomalies (1-9).
2. Case Presentation
2.1. Case 1
A 28-year-old woman with a twin pregnancy, which was conceived by ICSI, was referred for routine screening test in the first trimester. The result of semen analysis showed a low motility (35%) with a high abnormal morphology (87%). In the routine first trimester screening at 12 weeks and 2 days of gestation, the NT measurements of the first fetus was 3.4 mm (normal range for this age is 1.2-3.1 mm). Although she refused to undergo the triple test and we had no result for amniocentesis (karyotype) and fetus echocardiography, follow-up ultrasounds revealed normal results. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 3400 grams. Neonates were followed during the first 2 years of their life and none of them had developmental delay.
2.2. Case2
A 35-year-old woman, who was conceived by ICSI, was referred for the routine screening test during her pregnancy. Her obstetric and medical history revealed primary infertility for a period of 7 years, mild endometriosis and polycystic ovaries. The result of semen analysis indicated low motility (35%) and high abnormal morphology (88%). During the routine first trimester screening at 13 weeks of gestation, NT was measured at 3 mm. The normal range of NT for this age is 1.6-2.4 mm. Nuchal skin fold (NF) measurements and prenatal follow-up ultrasound findings were normal. A Triple test was performed, and it showed a positive result and a high risk of trisomy 21. The patient was referred for amniocentesis or chorionic villus sampling. The amniocentesis findings were normal and a healthy baby girl (weight = 3600 grams) was born after a full-term pregnancy. She was followed during the first and second year of life and no developmental delay was detected.
2.3. Case 3
A 33-year-old pregnant woman conceived by ICSI was referred for a routine screening test. Her obstetric and medical histories were unremarkable. The result of semen analysis indicated low motility (30%) and high abnormal morphology (81%). The result of the routine first trimester screening at 11 weeks and 5 days gestation showed a significant increased NT (NT = 5). The normal range of NT for this age is 1-2.8 mm. Later examination revealed that collection of fluid was not confined to the neck but was enveloped throughout the fetus. The result of follow-up such as prenatal ultrasound findings, result of an amniocentesis (karyotype) and echocardiography were reported normal. She gave birth to a healthy baby boy (weight = 3500 grams) at 37 weeks of pregnancy by elective cesarean section at term. Follow-up after birth till 2 years has revealed no developmental delay.
2.4. Case 4
A 26-year-old woman who was conceived by ICSI was referred for a routine screening test during her pregnancy. Her obstetric and medical history showed 8 years of primary infertility and polycystic ovaries. The result of semen analysis showed a low sperm concentration with a low total sperm count, low motility (30%) and high abnormal morphology (86%). First trimester measurement of NT at 12 weeks of gestation was 3.2 mm during the routine first trimester screening. The normal range of NT for this age is 1.1-3 mm. Although she refused to undergo amniocentesis (karyotype) and fetal echocardiography, triple test and follow-up prenatal ultrasound findings were normal. She gave birth at term to a healthy baby boy at 38 weeks (weight = 3500 grams). The 2-year follow-up after birth revealed no developmental delay.
2.5. Case 5
Following the routine screening test during pregnancy, a 31-year-old woman (conceived by ICSI) was referred to this institute. Her obstetric and medical history apart from 7 years primary infertility was unremarkable. The result of semen analysis revealed a low motility (35%) and a high abnormal morphology (92%). The result of routine first trimester screening at 12 weeks and 5 days of gestation showed an increased NT (3.3 mm) and generalized edema. The normal range of NT for this age is 1.5-3 mm. Although she refused to do the triple test and fetal echocardiography, follow-up prenatal ultrasound findings and amniocentesis (karyotype) were normal. She gave birth to a healthy term baby girl (weight = 3400 grams). Follow-up after birth revealed no developmental delay.
2.6. Case 6
A 30-year-old patient (conceived by ICSI) first presented to our institute at 12 weeks and 1 day of gestation and a twin pregnancy was detected. The second fetus was diagnosed with an increased NT (NT = 3.5 mm). The normal range of NT for this age is 1.2-3 mm. The couples’ history was significant for abnormal semen analysis. The result of semen analysis showed a sperm motility of 35% and an abnormal morphology of 80%. In this case, follow-up prenatal ultrasound findings and triple test were normal. Amniocentesis (karyotype) and echocardiography were cancelled because the patient refused to do so. Two healthy babies (boy and girl) were born at 37 weeks of pregnancy. The weights of the newborns were 2400 grams and 2900 grams. The neonates were followed for the first and second year of their life and none of them had developmental delay.
3. Discussion
Although measurement of the NT thickness combined with biochemical markers has a false-positive rate of 5% (10), it is regarded as a basic screening test with high sensitivity for identifying fetuses at risk for aneuploidy (1, 11, 12). However, NT is increased in 4.4% of euploid fetuses who are at risk for fetal anomalies and an adverse pregnancy outcome (12).
For this report first trimester ultrasound screening was performed for 703 women with a total number of 856 fetuses who were conceived by ICSI. First trimester measurement of NT was performed for 856 fetuses and 12 out of 856 fetuses with increased NT (NT ≥ 3) were taken for further investigation. In this report, six out of 12 cases who were chromosomally and anatomically normal fetuses with increased first trimester NT were described in detail. All these six fetuses had favorable prognosis despite the increased NT. We had no chromosomal report of the remained six fetuses because of reduction due to multiple pregnancies (4/12) and intrauterine fetal death (IUFD 2/12).
The chance of delivering a healthy baby decreases with NT thickness from approximately 70% for an NT of 3.5-4.4 mm to about 15% for an NT of 6.5 mm or more (13). Based on previous studies, fetuses with increased NT (less than 4 mm), normal karyotype and normal findings in the 20-week scan, showed a markedly increased favorable outcome (14). After a normal detailed genetic sonography and fetal echocardiography, the incidence of adverse outcome and developmental delay were not significantly different from the normal population (9). According to studies performed by Souka et al. fetuses with increased NT thickness have a high risk of adverse or poor pregnancy outcome (1, 13). In this study, we only had one case of increased NT and intrauterine fetal death (IUFD) and one case of premature rupture of the membranes (PROM).
This report is limited in number and should be further completed. In this series, semen analysis of all six cases were abnormal with a low motility of 30-35% and a high abnormal morphology of 80-92%. Although specific semen preparation technique in the case of impaired semen parameters in ART cycles is advisable, couples diagnosed with male-factor infertility should receive genetic counseling about the increased risk of congenital abnormalities before IVF-ICSI (15). This report provided six cases of increased NT with normal outcomes. It may help increase the confidence of couples who are reluctant to terminate the pregnancy. However, caution is necessary in cases of increased NT and parents should be offered a detailed fetal evaluation (genetic sonography) at the end of the first trimester and also at 18-22 weeks of gestation. Triple test, amniocentesis, fetal echocardiography and follow-up after birth are necessary.