1. Background
Malignant pleural mesothelioma (MPM) is a rare malignant neoplasm that typically affects individuals occupationally exposed to asbestos through a variety of industries. MPM is cancerous proliferation of mesothelial cells that involves a large extent of the pleural cavity and is the most common primary neoplasm of the pleura. The patients experience an insidious onset of symptoms including dyspnea, chest pain, cough, malaise, and weight loss (1).
Metastatic pleural tumor is a type of cancer that has spread from another organ to the membrane (pleura) surrounding the lungs. Lung and breast cancers most commonly spread to the lung. However, almost any type of cancer can spread to the lungs. The pathological diagnosis of MPM is difficult and special stains or immunohistological or ultra-structural analysis may be required to differentiate MPM from metastatic carcinoma of the pleura. Imaging plays an essential role in the evaluation of MPM. The radiographic findings of mesothelioma are nonspecific and more common diseases such as benign asbestos related pleural disease and metastatic carcinoma can look radiographically identical to mesothelioma. Computed tomography is the primary imaging modality used for diagnosis and staging of MPM. Generally, the combination of accurate history, examination, radiology, and the acquisition of pathology is essential to diagnose mesothelioma (2-4).
2. Objectives
The aim of this study is to differentiate MPM from metastatic carcinoma of the pleura by pathological and radiological assessment in order to investigate ability and accuracy of CT scan in this regard and also to evaluate CT features of these two diseases.
3. Patients and Methods
We conducted a retrospective study of 55 pleural malignancy patients including MPM and metastatic pleural disease cases hospitalized from 2009 through 2012 at a chronic respiratory center in Iran. Pathology and immunohistochemistry reports were considered as gold standard. The IHC panel of antibodies for differentiating malignant mesothelioma and metastatic carcinoma were HBME7, WT9, 0240, calretinin, CEA, MOC31, and CK5/6. Chest CT scans were performed in all patients with and without contrast with a single detector row CT scanner (Somatom plus; Siemens, Germany).
CT scans were observed by a chest radiologist, unaware of pathologic diagnosis. A checklist of relevant findings was fulfilled for each case and the most probable diagnosis according to CT scan was made by the radiologist.
Studied CT features consisted of pleural and pericardial effusion, pleural and pericardial thickening, parenchymal infiltration, fibrotic band, subpleural nodule, contralateral extension, contraction of involved hemithorax, pleural mediastinal shift, lymphadenopathy, thickening of the interlobar fissure, diaphragmatic involvement, and chest wall/hepatic/intraperitoneal invasion.
Data analysis was carried out using SPSS ver. 16 (SPSS for Windows, SPSS Inc., Chicago, IL) and the accuracy of radiology for differentiating MPM and metastatic carcinoma of the pleura was evaluated. Continuous variables were described by mean and standard deviation (SD) and categorical variables were described by frequency and percentage. CT findings were classified according to their prevalence and their contributing role for differentiating between mesothelioma and metastatic carcinoma.
4. Results
Fifty-five patients including 29 males and 26 females were evaluated in this study. According to pathology reports, 17 patients (11 males and 6 females) had mesothelioma and 38 patients (18 males and 20 females) were diagnosed with metastatic carcinoma of the pleura (30.9% mesothelioma and 69.1% metastatic carcinoma). On the other hand, according to radiology reports, 22 patients (14 males and 8 females) had mesothelioma and 33 patients (15 males and 18 females) were diagnosed with metastatic carcinoma (40% mesothelioma and 60% metastatic carcinoma).
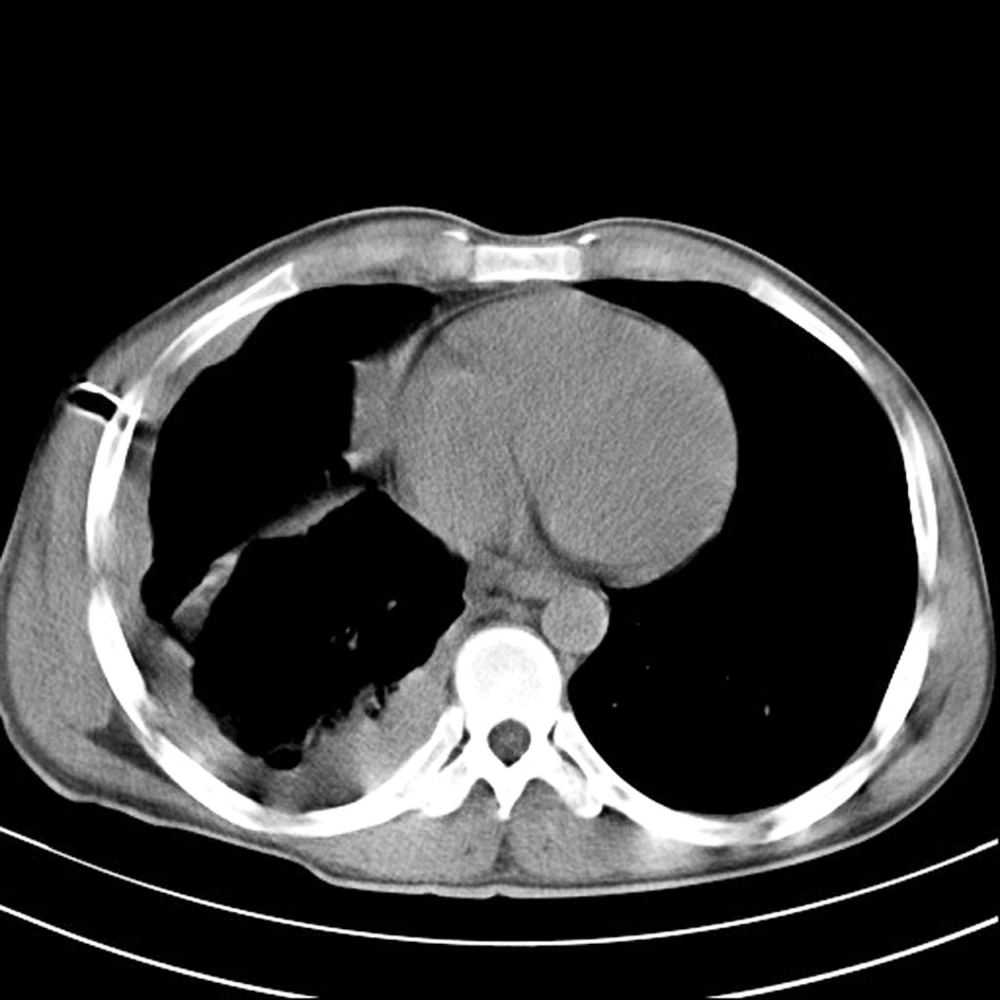
By radiology, 82% of patients with mesothelioma and 79% of patients with metastatic carcinoma of the pleura were diagnosed correctly. Among all 55 cases, the most common finding was pleural thickening (70.9%, n = 39) (Figure 1) followed by free pleural effusion (60%) and parenchymal infiltration (56.4%).
Based on pathology, we divided our cases into two groups of malignant mesothelioma (17 cases) and metastatic carcinoma (38 cases). Twenty imaging findings were assessed and their frequencies in each group are reported in Table 1.
| CT-Scan Findings | Malignant Mesothelioma | Metastatic Carcinoma | All Patients |
|---|---|---|---|
| Pleural thickening | 88.2 | 63.2 | 70.9 |
| Free pleural effusion | 35.3 | 71.7 | 60 |
| Massive pleural effusion | 11.8 | 55.3 | 41.8 |
| Mild/moderate pleural effusion | 23.5 | 15.8 | 18.2 |
| Loculated pleural effusion | 58.8 | 36.8 | 43.6 |
| Thickening of interlobar fissure | 47.1 | 18.4 | 27.3 |
| Contraction of involved hemithorax | 41.2 | 23.7 | 29.1 |
| Mediastinal Shift | 29.4 | 23.7 | 25.5 |
| Parenchymal infiltration | 35.3 | 65.8 | 56.4 |
| Subpleural nodule | 17.6 | 28.95 | 25.5 |
| Fibrotic bands | 41.2 | 42.1 | 41.8 |
| Contralateral extension | 17.6 | 26.3 | 23.65 |
| Lymphadenopathy | 23.5 | 39.55 | 34.5 |
| Diaphragmatic involvement | 23.55 | 13.2 | 16.4 |
| Chest wall invasion | 11.8 | 2.6 | 5.5 |
| Hepatic invasion | 5.9 | 0 | 1.85 |
| Intraperitoneal invasion | 17.6 | 2.6 | 7.3 |
| Pericardial effusion | 11.8 | 13.2 | 12.7 |
| Pericardial thickening | 23.5 | 13.2 | 16.4 |
a The values are presented as %.
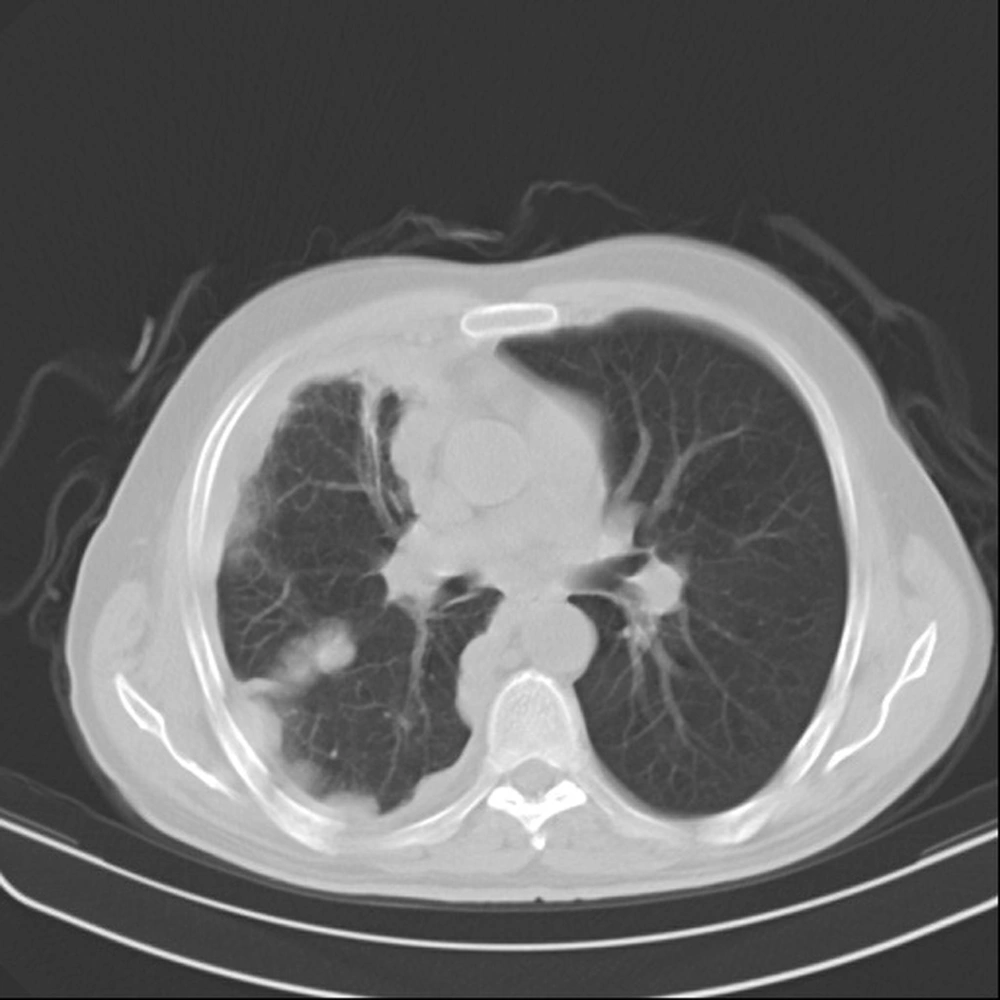
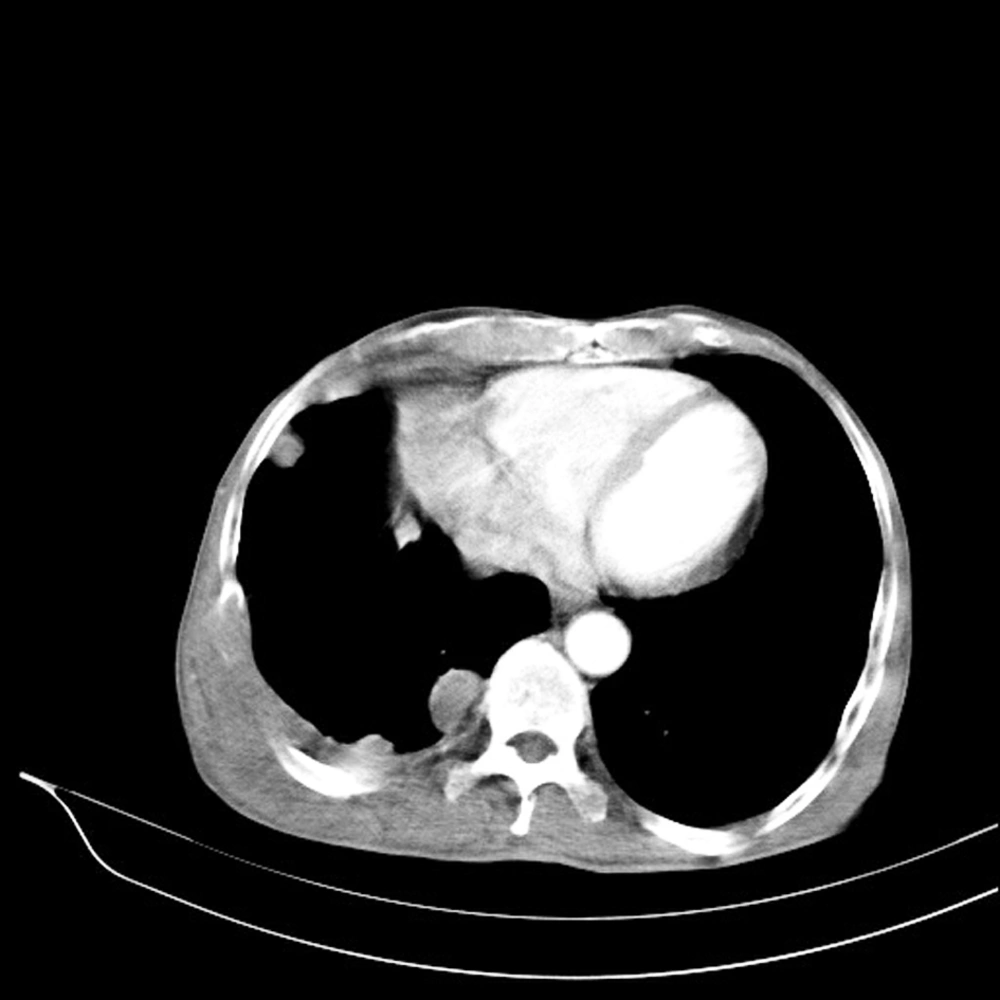
The most prevalent finding in the mesothelioma group was pleural thickening seen in 88.2% (n = 15) followed by loculated effusion in 58.8%, and thickening of interlobar fissure in 47.1% (Figure 2, 3 and 4). The least common finding in the mesothelioma group was hepatic invasion detected in one case. Other findings were observed at least in two cases.
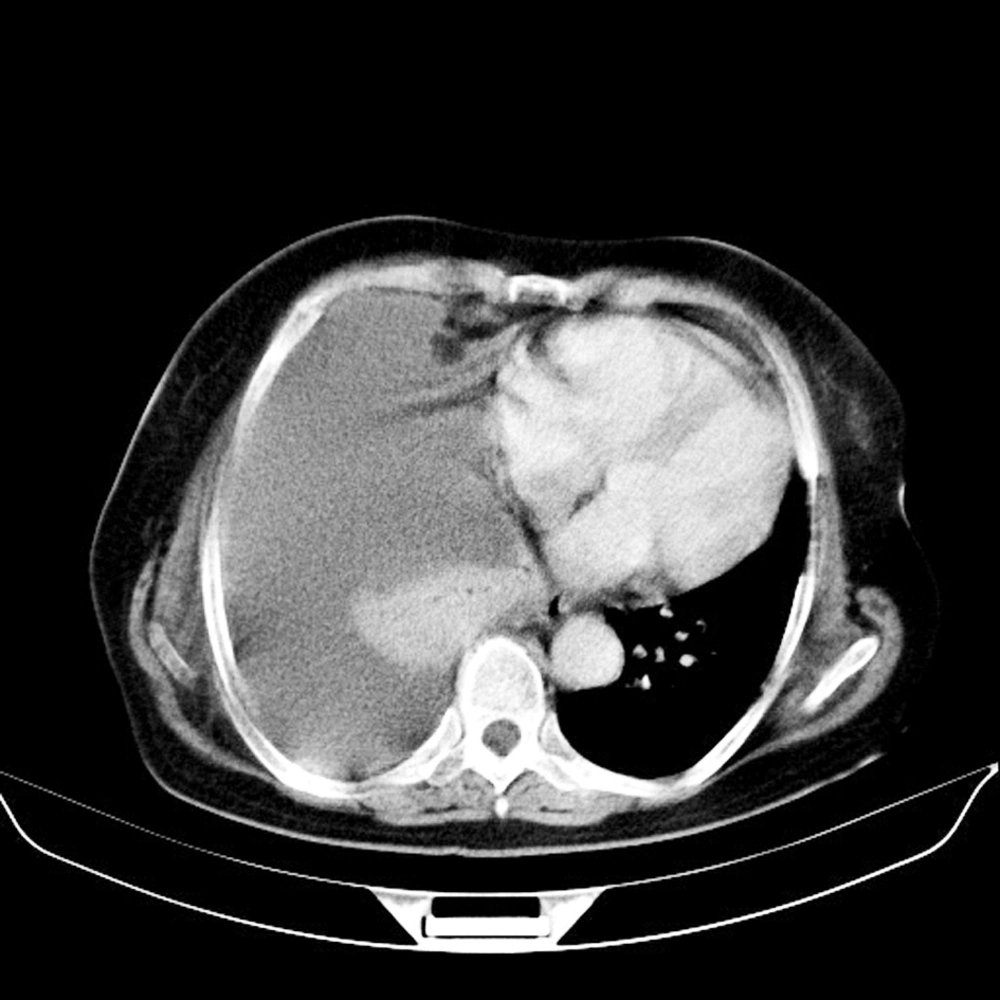
Among the metastatic group, the most common finding was free pleural effusion (71.7%, n = 27) and it mostly appeared as massive volumes rather than mild or moderate volumes (55.3% vs. 15.8%) (Figure 5). Parenchymal infiltration (65.8%) and pleural thickening (63.2%) were ranked second and third common findings, respectively, with an almost similar prevalence. None of the metastatic cases showed hepatic invasion, but chest wall and intraperitoneal invasion each were seen in one patient (Figure 6). Other findings were detected at least in two patients.
5. Discussion
Malignant pleural mesothelioma is a rare pleural malignancy that is diagnosed by imaging and histology assessment. One of its important differential diagnoses is pleural metastatic carcinoma with several similar imaging findings. In this study, we compared the radiologist and pathologist’s diagnoses on 55 pleural malignancy cases and investigated their CT findings.
According to chest CT scans in our study, 14 out of 17 mesothelioma and 30 out of 38 metastatic pleural malignancy cases were diagnosed correctly. It means that 82% of the patients with mesothelioma and 80% of the patients with metastatic carcinoma of the pleura were correctly diagnosed by the radiologist. It shows the high accuracy of CT scan in differentiating these two pleural malignancies.
Seely et al. in their study on 92 mesothelioma patients concluded that interobserver agreement (pathology and radiology) was excellent (5). Moore et al. said that the combination of radiology and acquisition of pathology is essential in the diagnosis of mesothelioma (6). Senyigit and colleagues mentioned in their study that although CT findings of MPM vary, they may provide a valuable clue to the diagnosis, at least in patients with a history of asbestos exposure (7).
According to our results, the three most common findings of pleural malignancies were pleural thickening, free pleural effusion and parenchymal infiltration. Similarly, in an article by Moore et al., nodular pleural thickening and pleural thickening > 1 cm are named as most helpful CT findings suggesting malignant pleural disease (6). We noticed that tumor invasion to the chest wall, liver and peritoneum are rarely seen among all cases, but they were more common in malignant mesothelioma compared to metastatic carcinoma. In the study performed by Wang et al., it has been mentioned that MPM is locally aggressive with frequent invasion to the chest wall, mediastinum and diaphragm (8).
In our study, among malignant mesothelioma cases, pleural thickening, loculated pleural effusion and thickening of the inter lobar fissure were the most prevalent CT findings and the least common ones were hepatic/chest wall invasion, massive pleural effusion, and pericardial effusion. In metastatic pleural disease cases, free pleural effusion, parenchymal infiltration, and pleural thickening were the most common CT findings and invasion to other organs, pericardial effusion, and thickening had the lowest rate in this disease.
Senyigit et al. in their study in 2000 on 117 mesothelioma patients reported that pleural effusion (89%), pleural thickening (82%), mediastinal pleural involvement (66%), and thickening of the interlobar fissure (53%) are the most common CT findings in mesothelioma patients (7). In a study conducted by Ng and colleagues on 70 MPM patients, pleural thickening (94%) and pleural effusion (76%) were the most common pretreatment findings (9) similar to a study carried out by Sahin et al on 84 MPM patients (10). Wang et al. named unilateral pleural effusion, nodular pleural thickening, and thickening of interlobar fissure the key CT finding of MPM (8). Also, in a study on 92 mesothelioma cases in 2009 by Seely and colleagues, pleural thickening was detected in all patients. They reported 87% pleural effusion in mesothelioma patients, which is different to our result, but they also confirmed that massive pleural effusion is not common in mesothelioma(5). Kawashima and Lidshitz also mentioned pleural thickening (92%) as the most common finding in MPM (11). Philippe Grenier wrote in his article that malignant pleural effusion is the most common manifestation of metastatic involvement, similar to our result (12).
Comparing the two groups, pleural thickening (P = 0.05) and thickening of the interlobar fissure (P = 0.02) are more prevalent in malignant mesothelioma; therefore, they can be considered as important parameters in favor of malignant mesothelioma.
Free pleural effusion is significantly more prevalent in metastatic pleural disease (P = 0.01) while its prevalence is modest in malignant mesothelioma. Massive pleural effusion (P = 0.003) and parenchymal infiltration (P = 0.03) are significantly more common in metastatic pleural disease as well. Therefore, they should be considered as important findings to differentiate these two diseases and parameters leading to the diagnosis of metastatic carcinoma of the pleura.
A study by Yilmaz et al. in 2005 demonstrated findings of malignant mesothelioma as involvement of interlobar fissure (sensitivity of 30%, specificity of 92%) and pleural thickening greater than 1 cm (sensitivity of 60%, specificity of 77%), whereas those of metastatic pleural disease are mediastinal/hilar lymph node enlargement and lung parenchymal involvement (13).
In Metintas and colleagues’ study which reviewed 99 MPM and 39 malignant pleural disease in 2002, ring-like pleural involvement, mediastinal pleural involvement, and pleural thickness more than 1 cm were considered as independent CT findings for differentiating between MPM and malignant pleural disease with the sensitivity/specificity values of 70/85 and 59/82,respectively (14).
Generally, this data analysis manifests that CT scan is highly accurate in differentiating malignant pleural mesothelioma and metastatic pleural diseases. Comparing malignant mesothelioma and metastatic carcinoma of the pleura, pleural thickening and thickening of the interlobar fissure lead us to the diagnosis of malignant mesothelioma and massive free pleural effusion insists on metastatic carcinoma diagnosis.