1. Introduction
Spontaneous rupture of an ovarian artery aneurysm is extremely rare and it can be a life-threatening condition. In a total 20 patients, 21 ovarian artery aneurysms were reported in the English literatures (1-10). These patients present with retroperitoneal hemorrhage and a painful mass in the lower back (3, 5, 8). Most of these cases occurred either late in pregnancy or in the puerperium (1-4, 7). In the past, most patients were treated by laparotomy, including adnexectomy and ligation of the involved ovarian artery (1, 4, 5). Recently, transcatheter arterial embolization is used as an alternative procedure for treatment of ruptured ovarian artery aneurysm. However, selective transcatheter embolization is a difficult procedure due to tortuosity and easy spasm of the ovarian artery (8, 9). Here, we report a 52-year-old post-menopausal patient with a spontaneously ruptured ovarian artery aneurysm, successfully treated by percutaneous transcatheter embolization, using n-butyl-cyanoacrylate (NBCA).
2. Case Presentation
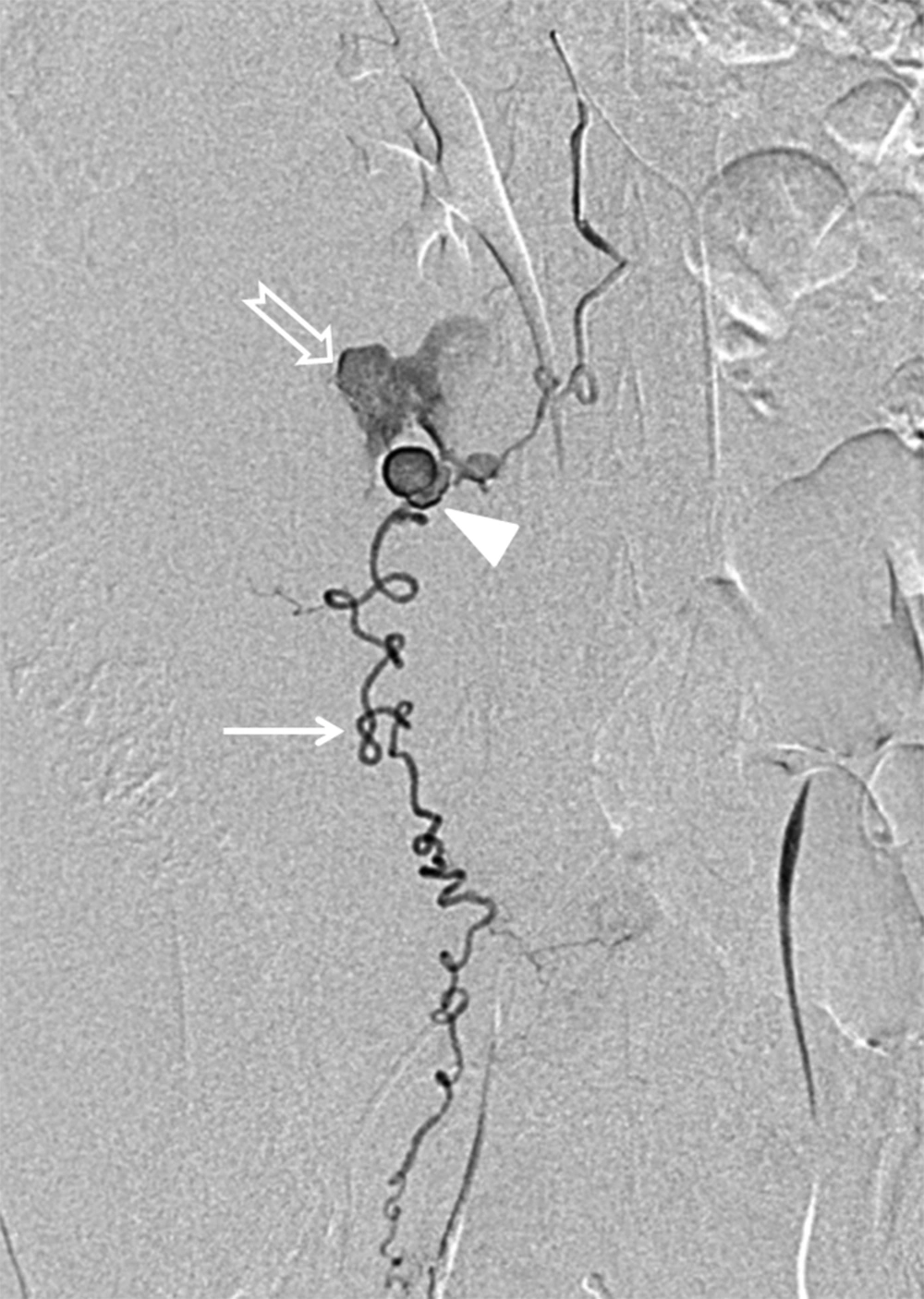
A 52-year-old post-menopausal woman without a previous history of pelvic or retroperitoneal surgical procedure, gravid 2 and para 2, presented to the hospital with a sudden onset of abdominal pain in the right lower quadrant for duration of one hour and a half with a squeezing nature. She had nausea and a chilling sense and no fever, vomiting, constipation, and diarrhea. She denied having any trauma or sexual intercourse. On arrival, her vital signs were: blood pressure, 87/63 mm Hg; pulse rate, 62 beats/minute; respiratory rate, 19 breaths/minute; and body temperature, 36.6 °C. On physical examination, the patient was pale and complained of tenderness and rebound tenderness over the right lower quadrant of the abdomen. She had no rigidity or muscle guarding of the abdominal wall. The hemoglobin level, which was 8.5 g/dL on arrival, decreased to 6.4 g/dL after a few hours. Emergency multi-detector computed tomography (MDCT) scan of the abdomen and pelvis showed a massive retroperitoneal hematoma with active contrast extravasation located at the right peri-renal and para-renal spaces, extending to the pelvis. A 64-slice MDCT scanner was used for scanning (Somatom Sensation 64; Siemens, Forchheim, Germany) with 120 cc of contrast medium (Ultravist; Bayer Schering Pharma AG, Berlin, Germany) in a rate of 3cc/sec. Coronal reformatted MDCT image revealed a tortuous right ovarian artery with aneurysm at the proximal portion of the ovarian artery (Figure 1). The diagnosis of rupture of an aneurysm of the right ovarian artery was suggested. After the initial resuscitation by normal saline loading and two pints of pRBC transfusion, her vital signs recovered: blood pressure, 119/64 mm Hg; and heart rate, 65 beats/minute. After discussion with the surgeon, it was decided to perform angiography and embolization, rather than laparotomy for the treatment of retroperitoneal bleeding because the vital signs of the patient were stabilized and MDCT image showed a rupture in the right ovarian artery aneurysm as a bleeding focus. Informed consent was obtained before the embolization procedure. Transfemoral angiography was undertaken to perform arterial embolization in an angiography suite (Axiom Artis; Siemens, Münhen, Germany). The abdominal aortogram revealed a 7.5mm-sized aneurysm and active contrast extravasation at the right lower paraspinal area (L2-3 level), which was identified at the proximal portion of the right ovarian artery. The right ovarian artery arose from the abdominal aorta, just near the orifice of the right renal artery. Selective right ovarian arteriography using a 5 Fr Cobra catheter and a 2.0 Fr microcatheter (ProgreatTMMicrocatheter System, Terumo Corporation, Tokyo, Japan) showed a characteristic tortuous course of the enlarged ovarian artery with an aneurysm and active contrast extravasation from the aneurysm (Figure 2). We planned to embolize the ruptured ovarian artery aneurysm, including the ovarian artery proximal and distal to the aneurysm, using liquid embolic material because the right ovarian artery, distal to the aneurysm, was too tortuous to insert the microcatheter. The aneurysm and proximal and distal portion of the feeding ovarian artery were successfully embolized by NBCA and lipiodol mixture (NBCA:lipiodol = 1:2) via microcatheter, which was positioned at the 2-3 cm proximal portion of the aneurysm. NBCA and lipiodol mixture was distributed well into the ovarian artery aneurysm and the adjacent ovarian artery proximal and distal to the aneurysm (Figure 3). 0.5cc NBCA was mixed with 1 cc of lipiodol. A NBCA and lipiodol mixture of approximately 0.75cc was used to embolizethe ovarian artery. Post-embolization aortography showed a complete exclusion of the ruptured right ovarian artery aneurysm and no collateral vessels supplying the occluded right ovarian artery. For angiography and embolization, 200 cc of contrast medium (Bonorex; CMS, Seoul, Korea) was used. The patient was transfused with an additional four pints of pRBC after embolization. The patient’s condition rapidly improved over the next 24 hours to normal clinical and hemodynamic parameters. The patient was discharged 12 days after embolization. At the 6-month clinical follow up, the patient was asymptomatic.
A 52-year-old post-menopausal woman with acute abdominal pain in the right lower quadrant. A) Arterial phase contrast-enhanced axial MDCT image shows an enhancing round aneurysm (small arrow) in the retroperitoneal hematoma (long arrow) B) Coronal MDCT image shows a tortuous right ovarian artery (small arrow) and aneurysm (empty arrow) located in the retroperitoneal hematoma (long arrow).
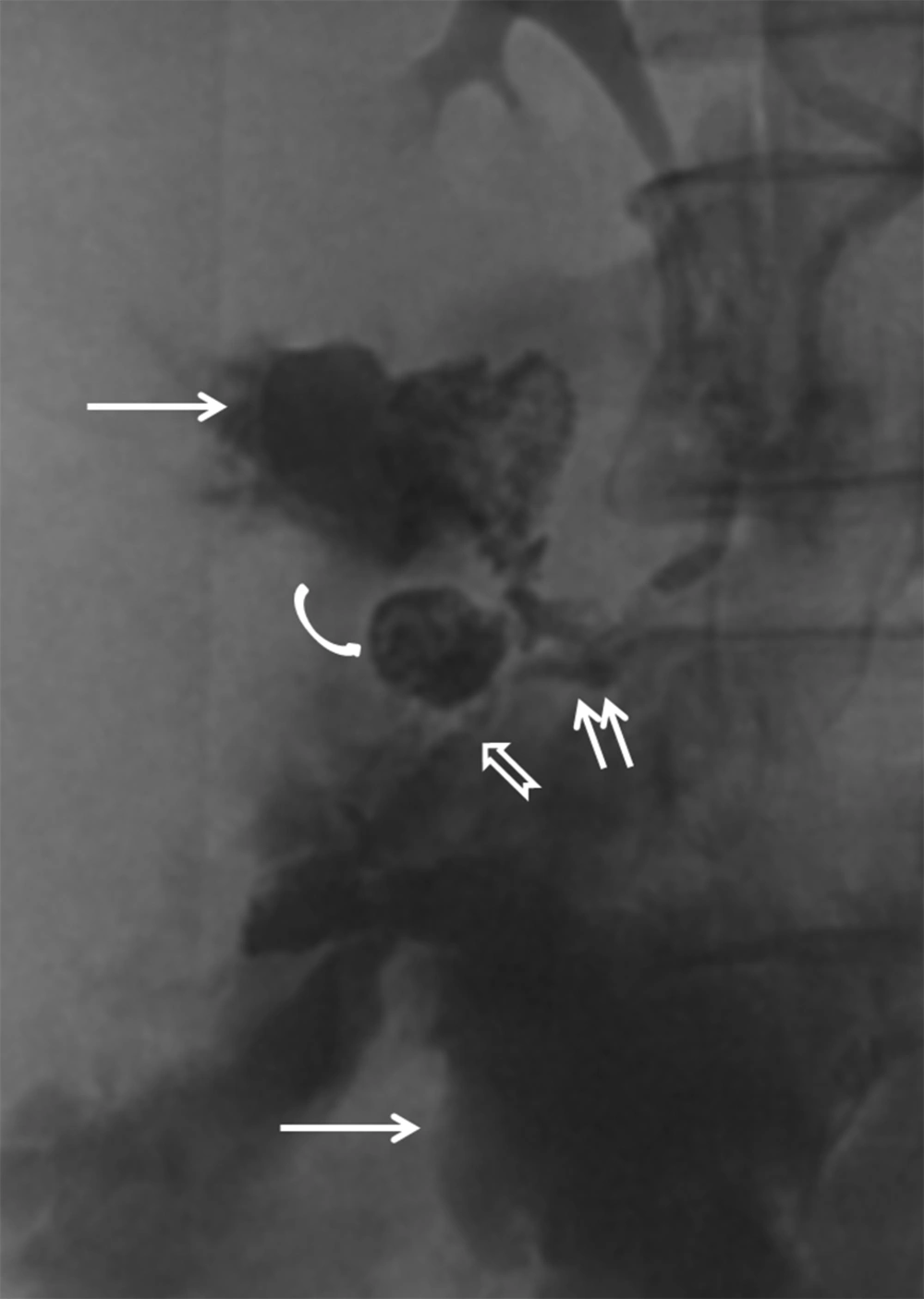
Spot image after embolization shows distribution of the glue located in the right ovarian artery in the same patient. The glue and lipiodol mixtures are located proximal (short arrows) and distal (empty arrow) to the ovarian artery aneurysm (curved arrow). Note the large amount of extravasated contrast media (long arrows) around the ovarian artery and the aneurysm during angiography and transcatheter embolization.
3. Discussions
The mechanism of ovarian aneurysm formation is not well understood. However, several important factors, ie, pregnancy-related hemodynamic and hormonal changes are implicated in the formation of ovarian artery aneurysm. Hemodynamic changes include increased cardiac output and systemic blood volume and variations in the blood pressure of the aorta and ovarian artery due to the expanded uterus. Microscopic vascular wall changes, which are related to hormonal changes during pregnancy, are known to make ovarian artery vulnerable to aneurysm formation. Failure of the normal process of involution of the ovarian artery may predispose to aneurysm formation (1-3). Most cases in the reported literatures occurred either late in pregnancy or in the peurperium(1-5, 7). Nakajo et al. reported embolization of the spontaneously ruptured ovarian artery aneurysm (6). They believed that prior pelvic surgery and uterine fibroid made a significant variation in the distribution of the blood flow; thereby, inducing structural changes in the ovarian artery and formation of an aneurysm. In our case, we think that multiparity of the patient may be the predisposing factor for formation of the aneurysm and spontaneous rupture. In patients with retroperitoneal hemorrhage due to spontaneous rupture of an ovarian artery aneurysm, persistent hemodynamic instability despite appropriate intensive care is an indication for surgery (3). Until now, almost all patients presenting ruptured ovarian artery aneurysm underwent exploratory surgery, and the most frequent treatment was adnexectomy and ligation of the artery, proximal and distal to the site of rupture (3, 9). In our case, we could primarily perform angiography and embolization of the right ovarian artery, including the spontaneously ruptured ovarian aneurysm because the vital signs of the patient were stabilized after initial vigorous fluid resuscitation and transfusion and MDCT image exactly showed active bleeding, with a focus on the right ovarian artery aneurysm as the cause of the right retroperitoneal hematoma. The embolic material used in embolization of the spontaneously ruptured ovarian artery aneurysms are as follows. Coils were used in three ovarian arteries in three patients (2, 3, 7). Coil with gelatin sponge particles were used in one ovarian artery in one patient (6). Kirk et al. reported a case in which the left ovarian artery and ruptured aneurysm were embolized by particulates, Thrombin-JMI, because coil embolization was proved to be difficult, due to vessel tortuosity and spasm (9). In that case, incidentally, a right ovarian artery aneurysm was embolized electively by coils a week later (9). It is the principle to place coils at both proximal and distal sides to the aneurysmal neck to prevent recanalization of the aneurysm through collateral circulation (6). However, coils were placed at the proximal portion of the aneurysm due to tortuosity and spasm of the ovarian artery (2, 3, 7). In our case, we planned to use liquid embolic material to embolize the proximal and distal portion of the ruptured ovarian artery aneurysm because the right ovarian artery showed severe tortuosity on selective ovarian artery angiography. NBCA was injected into the ovarian artery as close as possible to the ruptured aneurysm. The ruptured ovarian artery aneurysm, including the ovarian artery proximal and distal to the aneurysm was successfully embolized using NBCA. Although recanalization of the ovarian artery did not occur in the previously reported cases, in which embolization was performed by coils at the proximal portion of the aneurysm (2, 3, 7), we think that it is more reasonable to embolize by particulate or liquid embolic materials, such as NBCA, at both the proximal and distal sides of the aneurysm to prevent recanalization through the collateral vessels. It has been reported that catheterization of the ovarian artery had failed in two cases due to the small caliber of the ovarian arteries in patients with spontaneously ruptured ovarian artery aneurysm (8, 10). Although it is difficult to make definite recommendations regarding the optimal treatment strategies due to the small number of reported cases, catheter-directed embolization treatment could be considered as the first line treatment option in patients with spontaneously ruptured ovarian artery aneurysm unless the vital signs are unstable. In case of spontaneously ruptured ovarian artery aneurysm, use of liquid embolic material would be a better choice than coil because the ovarian artery usually shows a severely tortuous course.