1. Background
Blunt abdominal injuries are one of major causes of traumatic morbidity and mortality.. In the last decades we have seen continuing controversy in determining the most appropriate and feasible screening modality in blunt abdominal trauma patients.. In dealing with blunt abdominal trauma ultrasonography was first used by Kristiansen in 1971. The capabilities of ultrasonography have continued to grow and the increasing popularity of this noninvasive diagnostic procedure led to a dedicated term “Focused Abdominal Sonography for Trauma” (FAST) for a target based ultrasonographic evaluation of blunt abdominal trauma patients since 1990s(1).
Currently, ultrasonography is the modality of choice in the detection of hemoperitoneum in patients with blunt abdominal trauma and it has replaced diagnostic peritoneal lavage (DPL) (2-4).The utility of FAST has been widely acknowledged, and it is being used in prehospital, combat, and veterinary settings, as well as out of earth space (5-7).The main focus of the FAST examination has been the detection of free fluid within the abdomen of blunt trauma patients and in this regard, a wide range of sensitivity has been reported in several studies (42-87%) (8, 9). The sensitivity depends on different factors; the two most important of which are expertise of the operator and the amount of free fluid in the peritoneal cavity at the time of sonography, especially for the inexperienced operators. Different studies have shown that a minimum of 100 to 600 cc of fluid is detectable by FAST exam (10, 11).The initial FAST examination is like a snapshot in time. Delayed secondary FAST examination performed as a part of follow-up physical examination of the blunt abdominal trauma patient may be useful in two ways. First, it may give the sonographer more time for a comprehensive exam after stabilization of the patient. Second, the amount of free fluid may increase with time and would be more amenable to sonographic detection. However, the value of secondary sonography has not been fully investigated. The aim of this study was to evaluate whether the secondary ultrasound examination will increase the sensitivity of FAST examination.
2. Objectives
The present study was conducted to determine the diagnostic accuracy of delayed ultrasound exam compared with primary ultrasound exam in detecting free intraperitoneal fluid in patients with blunt abdominal trauma.
3. Patients and Methods
3.1. Participants
We performed a prospective study on all stable multiple trauma patients with physical insults or injuries simultaneously in several parts of the body admitted to Poursina University Hospital from March to October 2010.
3.2. Test Methods
Primary (immediate) and secondary (delayed) sonographic exams were performed within 30 minutes and 12 hours after admission to the emergency ward, respectively. In our study, we scanned five intraperitoneal spaces conventionally assessed in patients with blunt abdominal trauma, including hepatorenal (Morison’s pouch), splenorenal, right and left subdiaphragmatic and pelvic spaces with a curvilinear probe (3.5 MHz transducer), as well as the interloop space with a linear probe (10 MHz transducer).
Ultrasound exam was considered positive if any free intraperitoneal fluid was detected; however, one exception was visualization of small amounts of free fluid within the pelvis of women of childbearing age. Regarding the previous studies, we ignored the small amounts of fluid in the pelvic space of this group unless abnormal clinical signs or accompanying fluid in other abdominal spaces was detected. All positive results were compared with intra-operative and/or computed tomography (CT) findings. CT scan or surgical intervention was delayed or performed in none of the patients based on study preferences and the only determinant in this regard was the preference of the referring surgeon and clinical indications. The patients who did not need abdominal CT scan or surgery in the serial follow up exams, were considered as normal. Based on previous studies (12, 13), a simple scoring system was developed. One point was given for each anatomic space in which the fluid was detected. The maximum and minimum scores were 6 and 0, respectively.
Parenchymal injury was searched during primary and secondary ultrasound exams and was reported if present, but only the presence of free fluid in peritoneal spaces was documented in our study data sheets. The presence of solid organ parenchymal injury or pleural and pericardial fluid was not included in hemoperitoneum scores.
In all cases, the FAST sonography was performed by four on call radiology residents using the ultrasound machine Ultrasonix sp (Ultrasonix Medical Corporation) with 3.5 MHz curvilinear and 10MHz linear probes. Radiology residents who performed the ultrasound exams in this study had the experience of more than 400 FAST examinations. This study was approved by the hospital’s Institutional Review Board and informed consent (written or oral) was obtained from all conscious patients or the patient’s relatives in case of unconsciousness.
3.3. Statistical Analysis
We used the SPSS software version 18.0 (SPSS Inc. Chicago, IL) for all data analyses. Statistical analysis was performed by using Wilcoxon and McNemar tests.
4. Results
During the study period, 372 blunt abdominal trauma patients entered the study and were evaluated by FAST examination. Sixty one of these patients did not undergo secondary ultrasound examination due to various reasons (e.g. expiration, being emergently transferred to the operating room and leaving the hospital) and were excluded from the study.The remaining 311 patients (243 males and 68 females) with the mean age of 35.5(3 to 84 years) underwent both primary and secondary ultrasound.
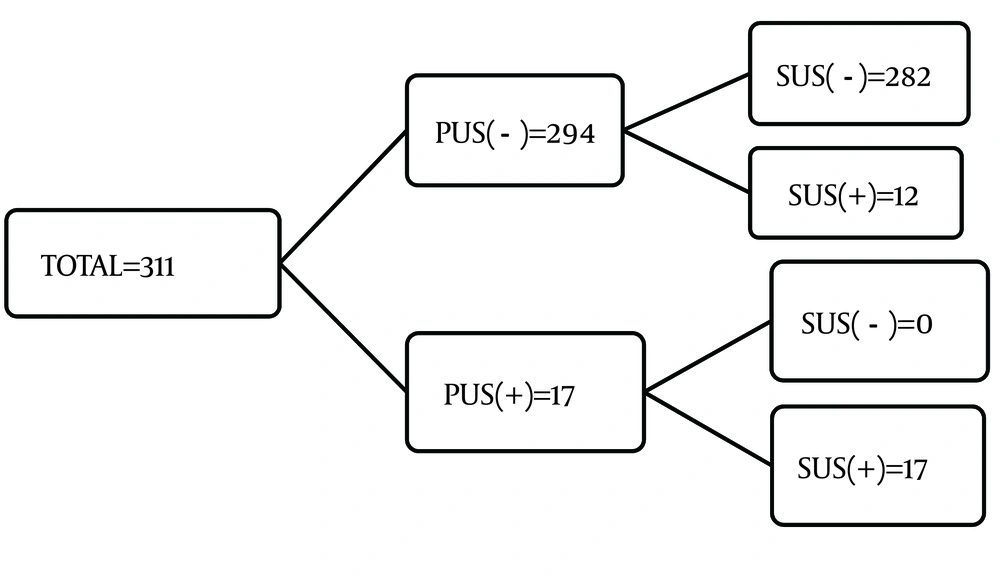
Forty one of 311 patients were found to have abdominal pathology (hemoperitoneum or parenchymal injury) with respect to their ultrasound, CT scan and/or intra-operative findings. As shown in Table 1, we divided our patients into nine groups. For the purpose of statistical analysis, we put patients with a positive finding only in the interloop area into a separate group. In 271 cases, neither the first nor the secondary ultrasound exam detected free fluid. For those cases with negative FAST scans, three were found to have free fluid by subsequent CT scans or intra-operative findings. CT scan or surgery was done in 62 of these patients either because of persistent abdominal pain or change in clinical condition.
Nine patients with a primary negative exam had a secondary positive exam; among whom five had delayed positive findings only in the interloop space (NEG-Only interloop POS) and four had secondary positive findings also in other spaces (NEG-POS).
Fourteen patients had fluid only in the interloop space in the first exam. In six of them, the fluid was detected in the same space in the secondary exam (Only interloop POS-Only interloop POS), and in the remaining eight, the fluid was distributed into other spaces (Only interloop POS-POS). Fifteen patients had positive findings in both primary and secondary exams (POS-POS).
All primary or secondary ultrasound positive results were compared with intra-operative and CT findings and/or clinical observation.
Only in two patients with a positive primary exam that was confirmed with a secondary exam, the CT scan showed no free fluid (false positive) (Figure 1).
| Primary US Exam | Secondary US Exam | CT Scan or Intraoperative Findings | Number |
|---|---|---|---|
| NEG | Only interloop POS | POS | 5 |
| NEG | POS | POS | 4 |
| Only interloop POS | Only interloop POS | POS | 6 |
| Only interloop POS | POS | POS | 8 |
| POS | POS | POS | 15 |
| POS | POS | NEG | 2 |
| NEG | NEG | POS | 3 |
| NEG | NEG | NEG | 59 |
| NEG | NEG | Not performed | 209 |
Patients Grouping Including the Results of Interloop Space Sonography a
The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the primary and secondary ultrasound exams were calculated based on CT, intra-operative and/or clinical findings (Table 2). We also measured the hemoperitoneum scores for primary and secondary exams (Table 3).
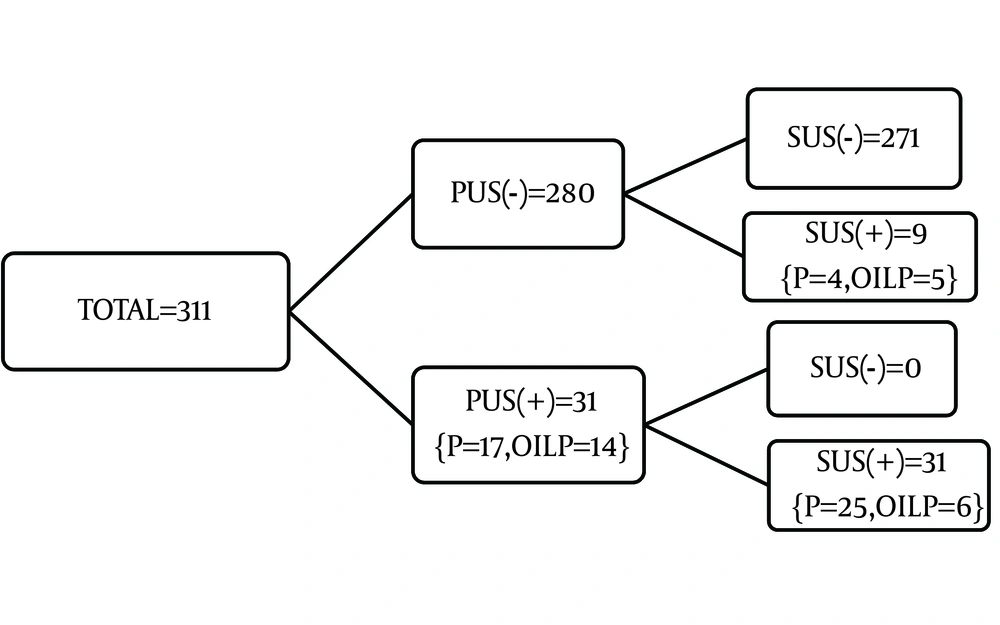
In order to evaluate the effect of examining the interloop space, which is not routinely evaluated in FAST exam, we analyzed our data again ignoring the results of examining the interloop space (Tables 4-6Figure 2). As shown in Table 4, this time, fluid detection only in the interloop space (Only interloop POS) would not be interpreted as positive. Combining only interloop POS-Only interloop POS and negative-Only interloop POS with NEG-NEG and also adding only interloop POS-POS groups to NEG-POS groups, we will have six groups instead of nine this time.
| Primary US Exam | Secondary US Exam | P Value, McNemar’s Test | |
|---|---|---|---|
| Sensitivity, % (95% CI) | 70.7(65.6-75.8) | 92.7 (89.8-95.6) | 0.01 |
| Specificity, % (95% CI) | 99.3 (98.2-100) | 99.3 (98.4-100) | 1 |
| PPV, % (95% CI) | 93 (90.2-95.8) | 95.7 (93.4-98) | 0.792 |
| NPV, % (95% CI) | 95.7 (92.6-97.4) | 98.9 (97.7-100) | 0.022 |
Diagnostic Accuracy Indices of Primary and Secondary Ultrasonography Exams a
| Primary US Exam | Secondary US Exam | CT Scan Intraoperative Findings | Number of Patients |
|---|---|---|---|
| NEG | POS | POS | 12 |
| POS | POS | POS | 15 |
| POS | POS | NEG | 2 |
| NEG | NEG | POS | 3 |
| NEG | NEG | NEG | 70 |
| NEG | NEG | Not performed | 209 |
Patients Grouping Ignoring the Interloop Space Sonography Results a
| Primary US Exam | Secondary US Exam | P Value, McNemar’s Test | |
|---|---|---|---|
| Sensitivity, % (95% CI) | 36.6 (31.2-42) | 65.9 (60.6-71.2) | 0.015 |
| Specificity, % (95% CI) | 99.3 (98.2-100) | 99.3 (98.2-100) | 1 |
| PPV, % (95% CI) | 88.2 (84.6-91.8) | 93.1 (90.3-95.9) | 0.572 |
| NPV, % (95% CI) | 91.2 (88.1-94.3) | 95.0 (92.6-97.4) | 0.73 |
Diagnostic Accuracy Indices of Primary and Secondary Ultrasonography Exams Ignoring the Interloop Space Sonography Results a
| Primary US Exam | Secondary US Exam | P Value (Wilcoxon Test) | |
|---|---|---|---|
| All patients | 0.12 ± 0.61 | 0.22 ± 0.8 | 0.0001 |
| Patients with pathology | 0.87 ± 1.48 | 1.63 ± 1.62 | 0.0001 |
Mean Hemoperitoneum Score Ignoring the Interloop Space Sonography Results (0 to 5) a
5. Discussion
It is believed that the role of FAST examination has evolved such that its greatest utility at present is the triage of hemodynamically unstable blunt trauma patients to the operating room when positive and allowing for further stabilization and more diagnostic testing such as CT scan and DPL in case of negative result to mitigate the risk of unnecessary laparotomy.
There are many factors that could influence the sensitivity of FAST exam. It is well known that ultrasound examination is operator dependent. Although the technique of FAST scan seems to be easily attainable in first impression, physicians do need extensive training to become familiarized with the skill. There is no international agreement about how long and how many exams the operator should perform to be accredited to do the FAST exam. For example, the American College of Emergency Physicians’ ultrasound guidelines recommendations published in 2001 recommended only 25-40 supervised examinations (14). In our study, the on call radiology residents who performed the exams had experience of over 400 supervised FAST exams.
As many studies showed, FAST exam is limited or unable to detect certain types of injuries, such as bowel, mesenteric, diaphragmatic, solid organ and retroperitoneal injuries (9, 15, 16). Other causes of false negative results are obesity, failure to recognize intra-abdominal blood clot and empty bladder for ultrasonic window (17).
The aim of FAST exam is to detect free intraperitoneal fluid secondary to bleeding from abdominal organ injury. Studies suggest that the average volume of fluid detectable by FAST scan ranges from 100 to 600 mL (10, 11).
According to the theory that there is a time lag for accumulation of a significant amount of blood in the peritoneal cavity to be detectable by sonography, repeating the ultrasound exam after a time lag may be an important factor.
Despite recommendations of several essays in performing “secondary ultrasonography” in patients with blunt abdominal trauma (15, 18, 19), the value of secondary sonography has not been fully investigated.
It is postulated that accumulation of further intraperitoneal fluid may allow it to be more easily detected in the secondary FAST when compared with the initial FAST exam. This subsequently leads to an increase in the sensitivity of secondary ultrasound exam compared with the primary exam in detecting intraperitoneal blood or injury. The significant increase in the mean hemoperitoneum score on the secondary exam compared with the primary exam in our study, in all patients, and especially in patients with positive results (0.2 to0.34 and 1.48 to 2.58, respectively) is in favor of this hypothesis.
Confirming the results of previous studies (20, 21), and as it is shown in Tables 2 and 5, our data show that performing secondary ultrasound exam does indeed increase the ability of ultrasound in detecting intraperitoneal fluid by significantly increasing the sensitivity from 70.7% to 92.7% and the negative predictive value from 95.7% to 98.9%. Use of secondary ultrasound exam also increased the positive predictive value from 93% to 95.7%, though it was not statistically significant in this study.
One of the original studies on the use of sonography in trauma patients outlined a single view of hepatorenal fossa, or Morison’s pouch to detect free fluid (22). Other studies have performed FAST examination in different ways (12, 13), but none of them has evaluated the importance of assessment of the interloop space as part of the FAST exam.
Before initializing this study, we noticed that the interloop space could be one of the primary spaces for collection of free fluid in blunt abdominal trauma patients.In order to test our hypothesis, we also examined the additional interloop space with linear high frequency probe both in primary and secondary FAST exams.
Free fluid in the interloop space is seen as a triangular hypoechoic area between bowel loops. Fluid-filled bowel loops may be misinterpreted as free fluid, but free fluid usually forms acute angles between the surrounding structures, and bowel loops may also have peristalsis.
We also analyzed both primary and secondary ultrasound exams with and without considering the results of examining the interloop space. We found that ignoring this space significantly decreases the sensitivity (from 70.7% to 36.6%), PPV (from 93.5% to 88.2%) and NPV (from 95.7% to 91.2%) of the primary exam, and the sensitivity (from 92.7% to 65.9%), PPV (from 95.0% to 93.1%) and NPV (from 98.9% to 95%) of the secondary exam in detecting intraperitoneal free fluid.
We concluded that adding the interloop space to our routine FAST examination could improve the ability of this test in detecting intraperitoneal blood.Comparison of primary and secondary FAST exam results with or without including the results of examining the interloop space showed that in both situations, the sensitivity of the secondary exam has significantly increased compared with the primary exam.Literature review showed that the sensitivity of FAST exam performed in blunt abdominal trauma patients ranged from 42%to 95% (9, 16, 22-29).
We have to emphasize that due to our inclusion and exclusion criteria, the values (sensitivity, specificity, NPV and PPV) for the FAST exam that we obtained in this study are not appropriate measures of everyday use of FAST examination and are only for comparison between primary and secondary ultrasound exam in the setting of the present study.
These values for FAST exam based on CT scan, intra-operative or clinical follow up results,, but it should be mentioned that it has not been proved that CT scan has an appropriate sensitivity. Second, the primary FAST exam sensitivity of 70.7% is relatively low compared to some similar studies in which the main purpose was to compare the diagnostic ability of ultrasound with other modalities (21, 22) and it may be explained by the fact that we did not include some of the patients with positive primary FAST results, who due to any reason did not undergo the second exam. Third, the importance of fluid in the interloop space was not our primary concern in this study and it should be evaluated by further studies. Forth, intra-observer and inter-observer variability of secondary FAST merits further investigation.
The optimal timing of secondary ultrasound scan should be defined. To avoid being too late or too early in performing the delayed scan and with attention to previous reports (20), we defined a wide range of time, from 30 minutes to 12 hours.
The deficiencies of an unblinded, prospective, clinical observation study are seen in our study.We can utilize the information obtained in this study to further increase the ability of FAST by performing a secondary exam and scanning the interloop area in any stable blunt trauma patient where the decision has been made not to perform an abdominal CT scan. Future studies will need to evaluate the added benefits of utrasonography (cost, time and radiation reduction) compared with CT scan in the evaluation of the abdomen in trauma patients.
Our data support the theory that secondary FAST scan will enhance the sensitivity of FAST examination by allowing enough fluid accumulation in the abdomen. Furthermore, scanning the interloop space in routine FAST exam may increase the sensitivity of FAST.