Dear Editor
Intrauterine Contraceptive Devices (IUDs) are a form of long-term, reversible, and safe contraception, which are commonly used worldwide. A regular medical check-up is necessary to determine its position within the uterus, up to six months after IUD insertion. The complications of translocation have a wide range from displacement of IUD in myometrium to uterine perforation. Predisposing factors which are considered to be associated with dislocation include postpartum insertion, inexperienced operator insertion technique, and position of the uterus (1). Clinical history, physical examination, and transvaginal ultrasonography (US) are common procedures for the evaluation of IUDs and related complications.
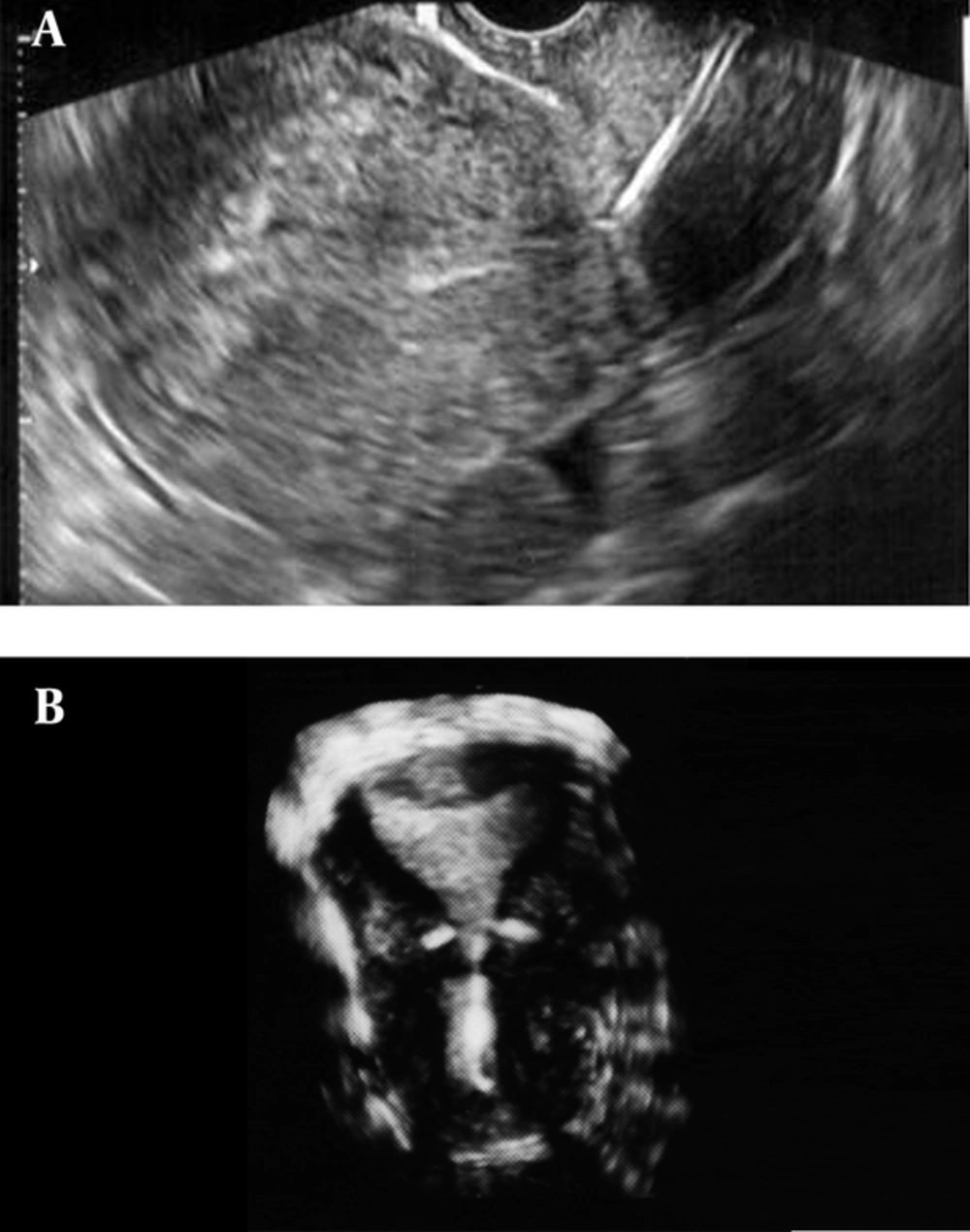
Although two-dimensional (2D) US (2DUS) is a routine modality in practice, it has a limited role for verifying two arms of IUD within the same plane; therefore, it may fail to detect IUD displacement (2). Furthermore, the most currently introduced hormonal IUDs can be demonstrated only by a vague shadow and might be remained unnoticed in 2DUS due to their low echogenicity (3). Recently, the availability of advanced US modalities has changed the management of IUDs by optimal evaluation of entire uterine cavity. Coronal view on three-dimensional (3D) US (3DUS) is particularly helpful to visualize the shaft and both horizontal arms in a single plane. In symptomatic patients with pelvic pain or abnormal bleeding, many IUDs, which appeared to be placed correctly or low on 2DUS, were confirmed to be imbedded, at least in part, within the myometrium with further investigations using hysteroscopy or 3DUS (4). The 3DUS is extremely useful in the management of IUDs by coronal views of the uterus and 3D-reconstructed views of the endometrium and adjacent myometrium.
Many studies demonstrated the overall outstanding effectiveness of 3DUS in determining IUDs’ location, particularly for symptomatic patients with complications or patients with hormonal IUDs. Valsky et al. reported that 3DUS has a great value in symptomatic patients when the location of IUD cannot be correctly identified with traditional 2DUS (5). Bonilla-Musoles et al. designed a comparative study for the identification and location of IUDs in 66 asymptomatic women by 2DUS and 3DUS. While position of all IUDs were identified accurately with 3DUS, 2DUS failed to identify the type of IUD in 9% as well as the position of IUDs in 3%, and misidentified IUDs in 12% of patients, which was later confirmed on 3DUS (2). Lee et al. claimed the complete visualization of IUDs in 95% of patients on 3DUS vs 64% on 2DUS (6).
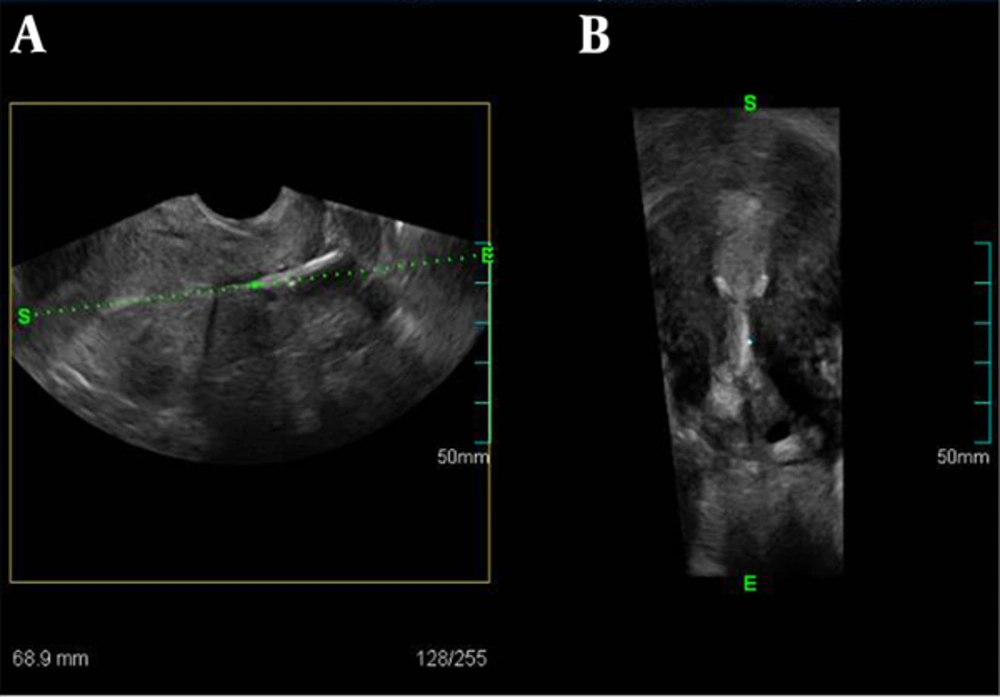
A, A low-lying of intrauterine device (IUD) in the lower uterine segment using standard two-dimensional imaging in second patient; B, The results of three-dimensional ultrasonography revealed t-shaped intrauterine device dislocated in endometrial cavity with arms of the intrauterine device imbedded within the myometrium.
In this paper, we present 2D and 3D images of three patients with a history of IUD, placed one to three years earlier, with complaints of abdominal pain or spotting. Low positioned IUDs were identified on 2DUS. Further investigation by 3DUS was required in these symptomatic patients in order to determine the exact location of IUDs. The 3DUS was performed using 3DXI (ACCUVIX XQ, Medison, South Korea) US device with a 6.5 MHz transvaginal probe. The 2DUS and 3DUS images of patients are compared in Figures 1 - 3.
Comparing two images of 2DUS and 3DUS demonstrated the additional information helping in identifying the cause of abdominal pain or spotting. Sites of IUD translocation vary in terms of their clinical significance and selection of subsequent therapeutic plan. Although menorrhagia and intermenstrual bleeding have been considered as a common adverse effect of IUD placement, pelvic pain and bleeding should raise the possibility of dislodgement, perforation, or passage. The 3DUS has a crucial role in the management of both asymptomatic patients and those with suspected complications, whilst IUDs location may remain unnoticed on physical examination and 2DUS.