1. Background
Sex determination from skeletal bones is very important for forensic science and anthropology (1-3).The pelvis and skull are the most commonly used bones for this purpose (1, 3-6). The highest number of bones with the most determinative features for sex differentiation are those of the pelvis (7-9). The anatomical differences observed in this region between men and women are entirely due to functional differences. The female pelvis shows favorable characteristics for carrying and delivering a baby (4).
Although sex determination is mostly performed based on pelvic bones, many different anatomical structures could also be used, examples of which are the subpubic angle, sciatic notch, acetabulum and the shape of foramen obturatum (FO) (2, 4).The subpubic angle and sciatic notch in the female pelvis are wider than those in the male pelvis (1, 2, 5, 8). Acetabulum is smaller in women and bigger in men. The shape of FO is large and oval in males but smaller and nearly triangular in females (10). All these evaluations for sex determination could be undertaken by morphological or metric methods (2, 4, 8, 9, 11-13). The morphological method is based entirely on visual evaluation (2, 13). It allows rapid evaluation but requires an experienced practitioner (8, 12) and interobserver agreement is highly variable (2, 4, 8, 12, 13). Furthermore, since statistical analysis is not possible, this type of evaluation is considered to be subjective (4). In contrast, metric methods provide a more objective assessment (4, 8, 12, 13), involving the measurement of various angles and lengths (4, 8). These methods allow a statistical analysis to be made based on the obtained numerical data obtained in order to reach a general conclusion and determine safety rates (6, 11). For this purpose, metric studies have been carried out in various ancestry groups using various techniques and parameters (3, 4, 8, 9, 14, 15). The commonly used imaging methods are X-ray and computed tomography (CT) (2, 8, 16) and one of the frequently evaluated parameters is the subpubic angle (1, 2, 8). To the best of our knowledge, no study has assessed the FO aspect ratio in terms of its value in sex determination.
2. Objectives
In this study, we aimed to evaluate the accuracy rate of the subpubic angle and aspect ratio of FO in sex determination and determine the cut-off values for differentiating between genders in Turkey. We used three dimensional (3D) volume-rendered images obtained by multidetector computed tomography (MDCT) of the pelvic bones.
3. Patients and Methods
The Medical Faculty of Eskisehir Osmangazi University Ethics Committee approved the study. The study was conducted in accordance with the principles of the Declaration of Helsinki. The study was performed by retrospective evaluation of pelvic CT images recorded between January and February 2018 and obtained from the hospital image archive.
3.1. Patient Selection
Randomly selected 50 females (age range: 25 - 91 years, mean age 56.7 ± 15.06 years) and 50 males (age range: 24 - 85 years, mean age 61.1 ± 13.9 years), who underwent pelvic CT at our hospital for any cause other than trauma (acute abdomen etiology, malignancy screening, and follow-up of solid organ tumors) were included in the study. None of the patients had any morphological disruption, such as history of pelvic bone surgery, metabolic bone disease or developmental hip dysplasia.
3.2. CT Imaging
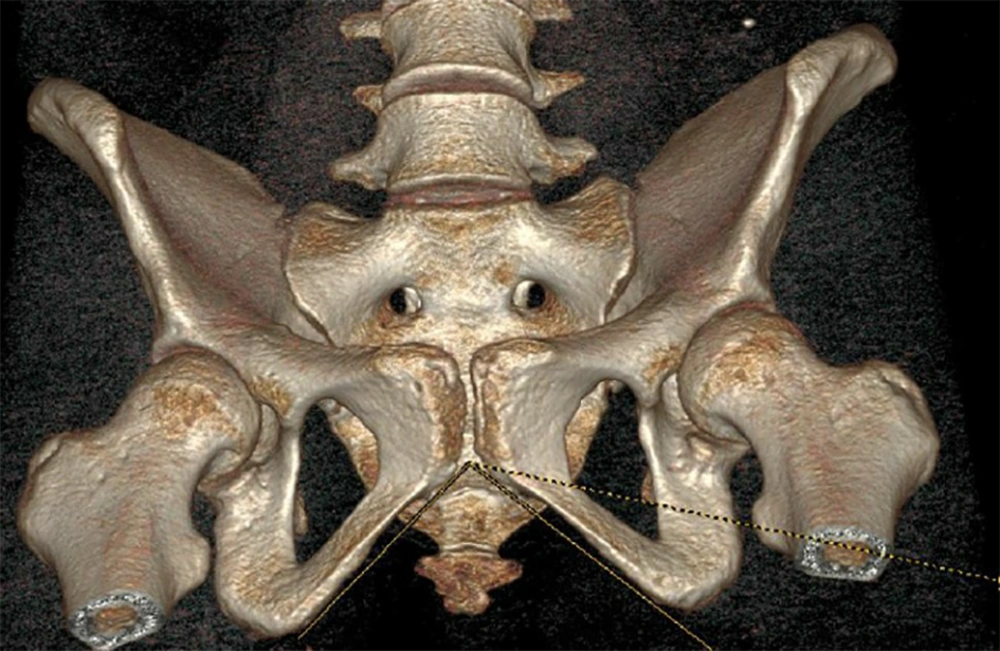
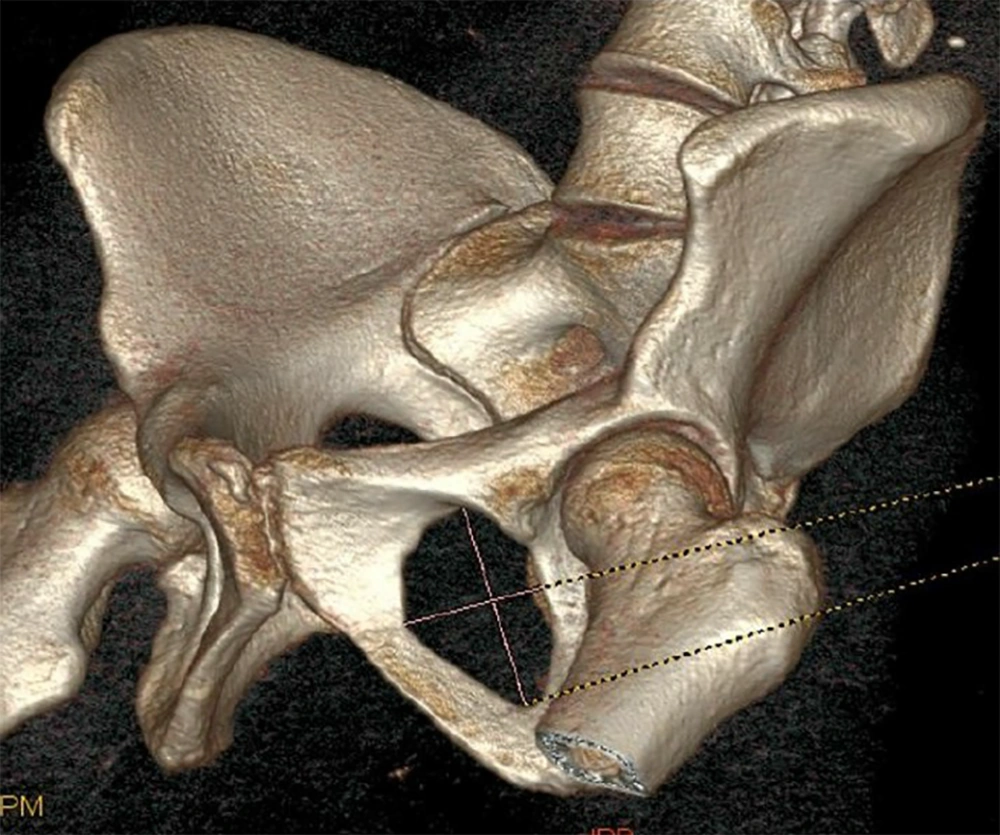
All imaging was performed using a 64-slice (Toshiba, Activion 16, Toshiba Medical Systems, Otowara, Japan) or a 128-slice (GE, Revolution EVO, USA) MDCT scanner. The imaging parameters were as follows: tube voltage 120 kV, tube flow 100 mA, and isotropic spatial resolution 0.5 mm. Volumetric datasets were processed on a dedicated image analysis workstation (GE, Advantage Workstation 4.3, USA) with advanced 3D volume rendering by a single senior radiologist with 10 years’ experience. The pelvic bones were visualized on the volume-rendered images. The angle between the ventral faces of bilateral inferior pubic ramus (the subpubic angle) were measured using an automatic angle meter (Figure 1). FO was best displayed on the right and left oblique images, and the aspect ratio was determined by the ratio of the largest transverse diameter to the largest longitudinal diameter (Figure 2). All measurements were performed by the first author, who is experienced in the hardware and software of analysis. For each parameter evaluated, two measurements were obtained on two different days in order to avoid possible technical errors. For statistical analysis, only mean values were used.
3.3. Statistical Analysis
Statistical analysis was performed using SPSS software V. 20.0 (Chicago, IL). The Shapiro-Wilk test was applied to check the normality. Intra-class correlation coefficient (ICC) was used to evaluate the intra-rater reliability. Inter-rater evaluation was not undertaken because the measurements were evaluated by a single radiologist.
ICC (95% confidence interval) was used to analyze intra-rater reproducibility. Based on the 95% confident interval of the ICC estimate, values less than 0.5, 0.5 to 0.75, 0.75 to 0.9, and greater than 0.90 indicate poor, moderate, good, and excellent reliability, respectively.
The parameter differences between the male and female sex were evaluated using the t-test. The Pearson correlation test was used to determine the relationship between the subpubic angle and the aspect ratio of FO by age. A P value of < 0.05 was considered statistically significant. The receiver operating characteristic (ROC) curve analysis and area of under the curve (AUC) were employed to determine the cut-off value. The following diagnostic indices were recorded for each cut-off value at the 95% confidence interval; sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and the accuracy rate.
4. Results
To determine ICC, the measurements were performed by the same author on two separate days. The ICC test showed excellent intra-rater reproducibility (0.94).
The descriptive statistics for the subpubic angle and aspect ratio of FO are summarized in Table 1. The subpubic angle varied between 75.9 and 101.2 in females (mean: 82.92 ± 15.06) and 47.4 and 91.5 in males (mean: 67.91 ± 9.15). There was a significant difference between the males and females regarding the subpubic angle (t-test, P < 0.0001). The ROC curve analysis of subpubic angle showed an AUC of 0.950. The best cut-off value of this curve was determined at 79.45 and based on this cut off point, we calculated the sensitivity of 98%, specificity of 94%, PPV of 94%, and NPV of 97% for sex determination. Furthermore, the accuracy rate of the subpubic angle in sex determination was 96%. Finally, the subpubic angle was found to be associated with age (Pearson correlation coefficients r = 0.247, P = 0.013).
| Sample size (no.) | Mean | Minimum | Maximum | Standard deviation | |
|---|---|---|---|---|---|
| Age | |||||
| Female | 50 | 56.7 | 25 | 91 | 15.06 |
| Male | 50 | 61.1 | 24 | 85 | 13.90 |
| Subpubic angle | |||||
| Female | 50 | 82.9 | 75.9 | 101.2 | 15.06 |
| Male | 50 | 67.9 | 47.4 | 91.5 | 9.15 |
| Aspect ratio of the right FO | |||||
| Female | 50 | 0.60 | 0.48 | 0.74 | 0.039 |
| Male | 50 | 0.55 | 0.45 | 0.68 | 0.058 |
| Aspect ratio of the left FO | |||||
| Female | 50 | 0.60 | 0.48 | 0.72 | 0.054 |
| Male | 50 | 0.54 | 0.45 | 0.69 | 0.052 |
Summary of the Descriptive Statistics for the Aspect Ratio of FO and Subpubic Angle
The aspect ratio of FO was 0.48-0.74 (mean: 0.60 ± 0.039) for the right side and 0.48 - 0.72 (mean: 0.60 ± 0.054) for the left side in females, and 0.45 - 0.68 (mean: 0.55 ± 0.058) for the right side and 0.45 - 0.69 (mean: 0.54 ± 0.052) for the left side in males. The differences in the FO aspect ratios between the two genders were statistically significant for each side (t-test, P = 0.01 for the right side and P = 0.01 for the left side). The ROC curve analysis of aspect ratio of FO for the right side showed an AUC of 0.797. The best cut-off value of this curve was determined at 0.615 and based on this cut off point, we calculated the sensitivity of 84%, specificity of 74%, PPV of 76%, and NPV of 82% for sex determination. The accuracy rate of the right-side FO in sex determination was 79%. The ROC curve analysis of aspect ratio of FO for the left side showed an AUC of 0.775. The best cut-off value of this curve was determined at 0.635 and based on this cut off point, we calculated the sensitivity of 98%, specificity of 32%, PPV of 59%, and NPV of 94% for sex determination. The accuracy rate of the left-side FO in sex determination was 65%. The aspect ratio of FO was not associated with age (Pearson correlation coefficients r = 0.078 P = 0.43 for the right side and r = 0.077 P = 0.44 for the left side).
5. Discussion
Male and female children and adults differ in terms of their skeletal structure, due to the influence of sex hormones, and therefore, skeletal measurements are widely used in sex determination (2). The adult female and male skeletons are different in size and shape. When assessed in terms of size, the male skeleton is generally larger than the female skeleton (4). However, it is not always possible to distinguish between large-sized female skeletons and small-sized male skeletons. Concerning shape assessment, the skull and pelvic bones are mostly investigated due to the clear differences between males and females (6, 7). However, the pelvis is known to provide more accurate results in sex determination than any other bone, including the skull (2, 7).
Determination of sex from skeleton could be undertaken by direct examination of bone structures or radiological methods (2, 11, 12, 16, 17). There are certain advantages of performing osteometric measurements radiologically, including keeping the bones intact, ease of use, and availability of this application in living cases. The X-ray used to be the preferred method in sex determination studies to investigate the pelvic skeleton, but recently MDCT has received increasing attention from researchers (2, 8, 11, 12, 16, 17). Problems originating from projection in the X-ray are not a problem for CT (12, 17). MDCT allows obtaining 3D volumetric images with high spatial resolution, making it easier to perform osteometric assessments (12, 17). The results of MDCT studies show that it is a highly reproducible method of examination and could be safely used in sex determination. For this reason, in this study, we chose to evaluate 3D volumetric images.
One of the most frequently used parameters in sex determination from the pelvis is the subpubic angle (1, 2, 8). In the literature, high accuracy rates reaching 95% - 98% have been reported (14, 18). In the current study, the accuracy of the subpubic angle in sex determination was 96%, which was even higher. In an MDCT study performed on people living in Anatolia, the average subpubic angle was found to be 65.9 in males and 82.6 in females, and the accuracy rate of this parameter in sex determination was calculated as 90.8% (2). In our study, we determined this angle to be 82.92 for females and 67.91 for males. This shows a good consistency between the results of this study and those of the previous research (2), both conducted to investigate the same ancestry in the same geography. It could be concluded that the subpubic angle alone is a highly reliable and reproducible parameter for sex determination.
It is not always possible to visualize skeletal bones as a whole. This often makes it difficult or even impossible to perform metric pelvic examinations that concern both hip bones, such as the subpubic angle (5). The shape of FO is an alternative parameter that could be used for sex determination only when the unilateral hip bone cannot be reached. However, using the visual shape for evaluation is subjective; thus, objective data and metric results are needed for more accurate results (4, 8, 12, 13). For this reason, in this study, we examined the usability of the FO width/height ratio in sex determination. In the literature, foramen magnum has been frequently used for this purpose, but to the best of our knowledge, the aspect ratio of FO has not been investigated before. In the current study, we found that the FO aspect ratio differs in male and female skeletons for both right and left sides. Our results suggest that when available, using the right-side hip measurements provides more accurate results. It is known that all body bones and anatomical structures are not always symmetric (7, 15). This could be explained by general anatomical variations and asymmetry. The data obtained from our study contribute to the literature in this sense.
The subpubic angle is one of the parameters with a high accuracy rate in predicting sex when compared to other measurements (1, 2, 8). Combined with other parameters from the pelvic region (iliac bone width, width of sciatic notch, diameter of acetabulum, pubic length, pubic thickness, ischial length, and shape of FO), the diagnostic accuracy of the subpubic angle can be further increased (15). In this study, we used the shape of FO, but future studies could be performed to evaluate other parameters listed above to create a database and ancestry-specific pelvic osteometry atlas. Multicentric surveys would provide sufficient samples for each age group. The cut-off values could be set for each ancestral line and ethnic group. We consider that this would eventually allow making sex determination with 100% accuracy using only pelvis bones.
In conclusion, the subpubic angle and aspect ratio of FO obtained from MDCT images present as parameters with a high accuracy rate for sex determination. The former had the highest accuracy in this study; however, based on our results, we consider that the aspect ratio of FO could also be useful for this purpose.