1. Background
Chronic low back pain could result from the lumbar facet or zygapophyseal joints (1). Pain originating from the facet joint could cause pain that spreads to the lower back, hips and proximal lower extremity, inguinal region and posterior thigh. Furthermore, it may cause paravertebral sensitivity resulting in pseudoradicular pain (2).
Clinical diagnosis of facet joint syndrome is made by excluding other possible reasons for the pain (3-5). Facet joint syndrome is characterized by an increase in back pain during movements that irritates the facet joints and is the cause of pseudoradicular pain in the hips, posterior thigh or inguinal region (2).
Nonsteroidal anti-inflammatory drugs (NSAID), electrotherapy (ultrasound, transcutaneous electrical nerve stimulation [TENS], and fluid therapy), facet joint ablation, radiofrequency (RF), facet joint injection and neurotomy (on the medial branch of the ramus dorsalis) are the treatment options for facet joint syndrome (6). Facet joint injection in spinal surgery is a common method for presurgery diagnosis and the treatment of facet joint syndrome. Facet joint blockage may also be used to decide on dynamic or rigid segmental stabilization (7). Facet joint blockage is a type of regional anesthesia which is performed selectively on the medial branch of the ramus dorsalis of the spinal nerve and is a current approach for the treatment of pain originating from facet arthropathy (6).
2. Objectives
The purpose of the current study was to determine the accuracy of the anatomic placement of facet joint blockage performed with ultrasonography with the reference of C-arm fluoroscopy.
3. Patients and Methods
3.1. Study Design and Patient Selection
We obtained ethical approval for this study from the Institutional Review Board of our hospital with the registration number of RY-2018-09. All the patients signed the informed consent form. Patients with chronic low back pain were evaluated. The criteria for inclusion in the study were age of > 18 years, no radiculopathy findings, paravertebral muscle strain, pain in lateral flexion and lumbar hyperextension. Patients with local or systemic infection, who were allergic to steroids or lidocaine and/or who demonstrated findings other than facet joint arthrosis on MRI were excluded from the study. A total of 22 patients (seven males and 15 females) who were diagnosed with facet joint syndrome at L3 - L4, L4 - L5 and L5 - S1 levels were included in the study. Their mean age was 63 years (range, 48-80). The diagnosis of the patients was made by examination and radiography (lumbar anteroposterior, lateral and oblique x-rays). The patients had more hypertrophy of the L3 - L4, L4 - L5 and L5 - S1 facets. When drug treatment and physical examination (about 3 months) failed in the patients, facet joint blockage was performed.
3.2. Procedure
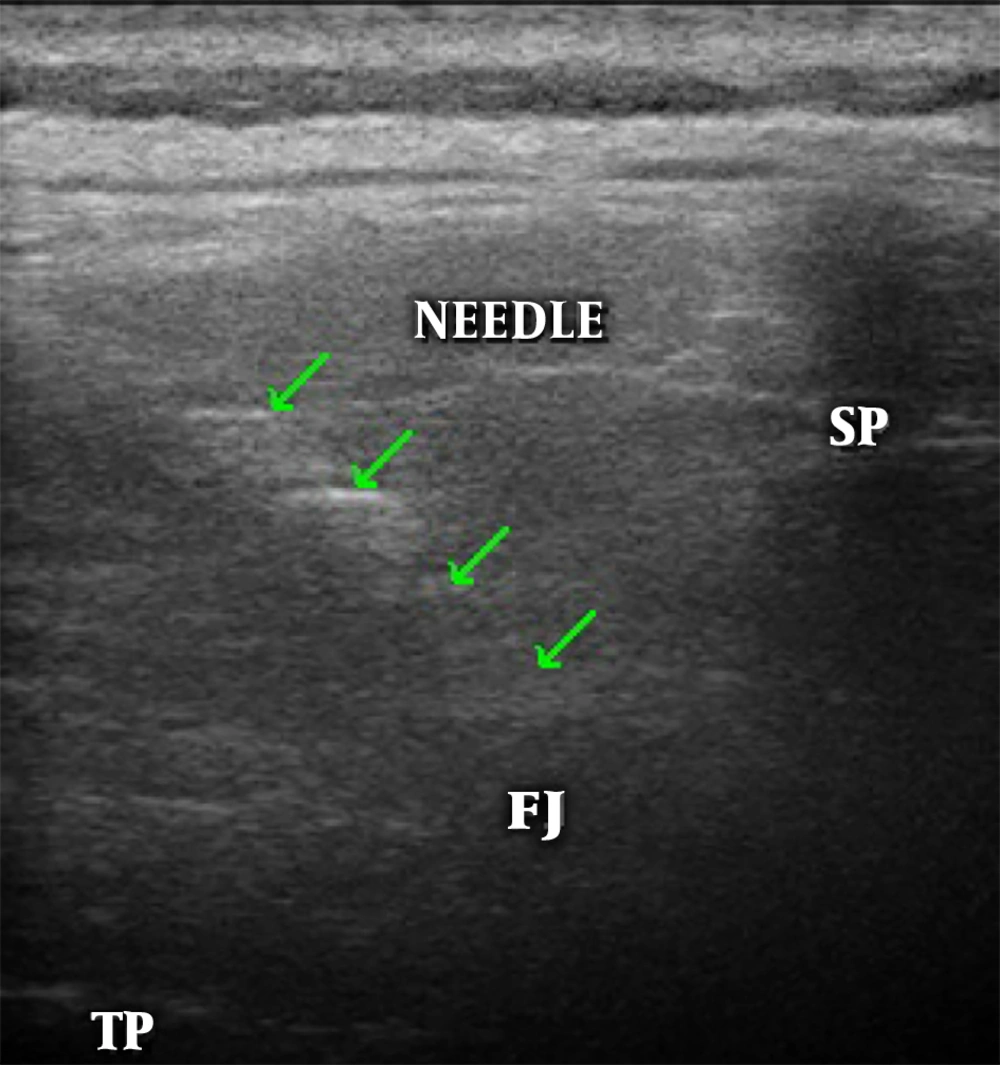
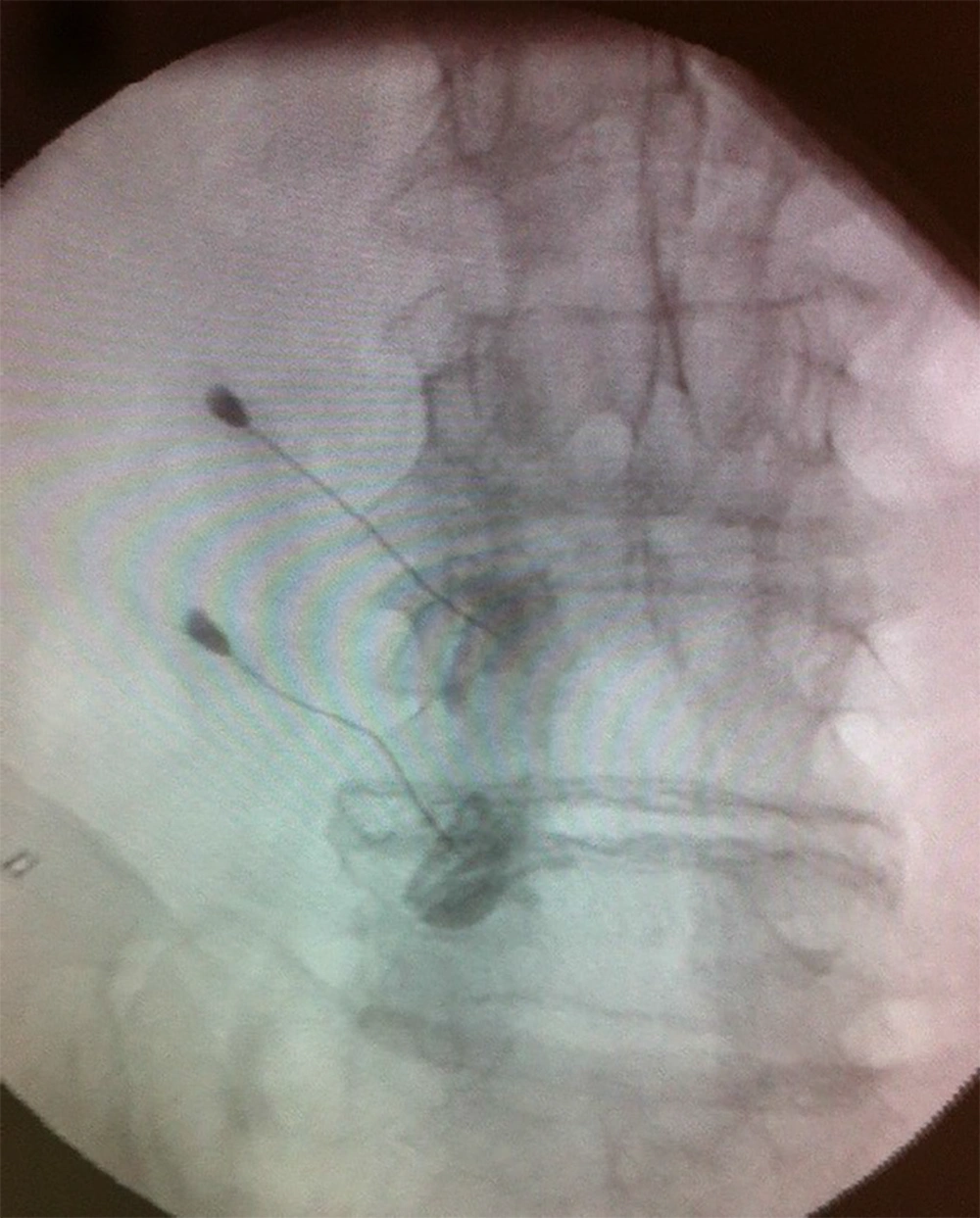
The facet joint blockage was performed under sterile conditions in an operating theatre with the patient in a prone position. The iliac crest, lumbar spinous processes and presumed injection points were located with palpation and marked. Local anesthesia (lidocaine hydrochloride) was applied to the region before the intervention. The spinous processes were found in the longitudinal axis using a 5 MHz convex transducer (Esaote MyLab 5). The facet joints were then located at a depth of 40 - 50 mm by shifting the transducer 2 - 2.5 cm laterally. When detecting the facet level in the practice segment, the transducer was adjusted to the transverse position so that the spinous process and facet joint transverse processes were imaged at the same time. Using the in-plane technique, at 1 cm lateral of the transducer, a 21 Gauge injector containing 0.5 mL radio-opaque agent (ioheksol) was inserted through the skin at an angle of 15° - 20° (Figure 1). After detection of the superolateral corner of the facet joint as the target point, the radio opaque substance was administered and checked with a C-arm fluoroscopy (Figure 2). After verifying the localization, a mixture of 40 mg triamcinolone and 1 cc 2% lidocaine was injected. The patients were discharged after the procedure on the same day.
3.3. Data Analysis
Mean, standard deviation, median lowest, highest, frequency and ratio values were used in the descriptive statistics of the data. The distribution of the variables was measured by the Kolmogorov-Simirnov test. Wilcoxon test was used in the analysis of the dependent quantitative data. SPSS 22.0 (IBM Corp., Released 2013, IBM SPSS Statistics for Windows, Ver. 22, Armonk, NY, USA) was used for analyses.
4. Results
Nerve blockage was applied to 67 facet joints at the L3 - L4, L4 - L5 and L5 - S1 levels in a total of 22 patients diagnosed with facet joint syndrome. Patients mean age was 63 (range, 48 - 80), the mean body mass index was 28.4 (range, 18.9 - 38.1), the mean symptoms duration time was 18 months (range, 12 - 36) and the mean time to determine facet localization with USG was 240 seconds (range, 140 - 320). The lumbar facet nerve block was performed on 23 at the L3 - L4 level, 32 at the L4 - L5 level and 12 at the L5 - S1 level (Table 1). Successful USG imaging was obtained at 61 of the 67 segments (Table 2). The facet joints could not be detected with USG in one patients 2 levels due to morbid obesity (body mass index [BMI]: 38, 1). In the C-arm fluoroscopy control after the injection of radio opaque material, the needle was found to be located in the lamina in 4 segments and it was relocated. Therefore, we corrected four faulty locations. Patients mean visual analog scale (VAS) decreased from 7 (range, 6 - 9) to 2.5 (range, 1 - 6) at the minimum 3 day after the procedure in the outpatient clinic (Table 3). This study concluded that the location of the facet joint with USG guidance is possible with 91% sensitivity and 100% positive predictive value. It took 235.9 ± 56.1 seconds to detect facet joint localization with the USG probe. No complications were observed.
| Min - Max | Median | Mean ± SD | % | |
|---|---|---|---|---|
| Age | 48 - 80 | 63.0 | 62.5 ± 8.2 | |
| BMI | 18.9 - 38.1 | 28.4 | 27.6 ± 4.6 | |
| Time to determine localization with USG, second | 140 - 320 | 240.0 | 235.9 ± 56.1 | |
| Symptoms duration, month | 12 - 36 | 18.0 | 20.2 ± 8.0 | |
| Gender | ||||
| Female | 15 | 68.2 | ||
| Male | 7 | 31.8 | ||
| L3 - L4 | ||||
| Right | 5 | 7.4 | ||
| Left | 2 | 2.9 | ||
| Bilateral | 8 | 23.8 | ||
| L4 - L5 | ||||
| Right | 4 | 5.9 | ||
| Left | 2 | 2.9 | ||
| Bilateral | 13 | 38.8 | ||
| L5 - S1 | ||||
| Right | 3 | 4.4 | ||
| Left | 1 | 1.4 | ||
| Bilateral | 4 | 11.9 |
Abbreviations: BMI, body mass index; SD, standard deviation; USG, ultrasonography.
| C-arm (skopi) | Sensitivity | Positive predictive value | ||
|---|---|---|---|---|
| (+) | (-) | |||
| USG | 91.0% | 100.0% | ||
| (+) | 61 | 0 | ||
| (-) | 6 | 0 | ||
Abbreviation: USG, ultrasonography.
| Min-Max | Median | Mean ± SD | P value | |
|---|---|---|---|---|
| VAS | < 0.000a | |||
| Preoperation | 6.0-9.0 | 7.0 | 7.2 ± 0.9 | |
| Postoperation | 1.0-6.0 | 2.5 | 2.9 ± 1.4 |
Abbreviations: SD, standard deviation; VAS, visual analog scale.
aWilcoxon test.
5. Discussion
Apart from the pain originating from the facet joint, situations that could cause pathological pain such as tumor, infection, disc herniation and vertebral fracture must be eliminated through detailed clinical and radiological assessments (8, 9). Low back pain detected as facet joint arthrosis through imaging methods that does not respond to symptomatic treatment and has been ongoing for 6 months, constitutes the main indication for facet joint blockage. However, it is contraindicated in systemic infection, allergy (to steroid or local anesthetic), coagulopathy or pregnancy (9, 10). In the examination, pain typically intensifies with flexion and extension, and decreases with contralateral flexion and spinal flexion. While facet joint injections can be used as a treatment method for low back pain, it can also be used for diagnosis to determine whether or not the pain originates from the facet joint (10).
C-arm fluoroscopy is a method that facilitates the accurate application of facet joint blockage and enhances the treatment success rate and clinical effect (11). However, there is the disadvantage that both the patient and practitioner are exposed to radiation, which has been well documented in the literature to enhance the risk of cancer and damage to the skin, muscles and the eye lens (12). The main advantage of ultrasonography over C-arm fluoroscopy is that it does not involve radiation. The mobility of the device and the relatively low cost are other advantages (13). The disadvantage of ultrasound is that it is a technician-dependent method that requires experience. Only four facet joint levels were misplaced and two facet levels were not localized by ultrason in four different patients. The mean BMI of all 22 patients’ was 28.4, while in these four patients, the mean BMI was 33.6. These findings suggest that the elevation of BMI reduces the effectiveness of ultrasonography in determining facet joint localization.
In a CT-controlled cadaver study to assess the reliability of USG, Galiano et al. noted that USG was both applicable and highly accurate (14). Using a probe with an accurate frequency and with placement in the accurate localization, the target tissue could be seen clearly in a few seconds and moreover, vascular formations in the injection area could be eliminated with a simultaneous doppler signal to ensure that the target tissue is reached safely. Additionally, USG makes the practice possible without exposing the patients or physicians to radiation, which can damage skin, bones, parathyroid glands and lungs. After repeated applications, pigmentation in the nails and hands has been reported (15). Injection under USG guidance could be a preferred method in clinics, since it is practical and does not entail exposure to radiation.
In a study conducted by Yun et al., the time was calculated between prone positioning of the patient and injection, under the guidance of USG or C-arm fluoroscopy. The duration of using C-arm fluoroscopy was 248.7 ± 6.5 seconds, whereas with USG, it was determined as 263.4 ± 5.9 seconds (2). However, those durations did not include preparation procedures and when the C-arm equipment preparation time was taken into consideration, USG guidance was seen to be more advantageous in terms of time. Nevertheless, the duration depends on the experience of the person. Although complications are rarely seen in facet joint blockage, they may be observed while placing the needle and giving the medication. These complications include bleeding related or unrelated to the intravascular entry, infection, dural injury, spinal anesthesia, neural trauma, spinal cord trauma, pneumothorax, exposure to radiation, hematoma and side effects related to steroids. In ultrasonography, the ability to visualize the vascular formation with Doppler decreases the risk of complications, which may occur as a result of intravascular entry (16-20). No complications occurred in our patients.
Although facet joint blockage for low back pain is a simple, reliable and cost-effective technique, most previous studies have been noncontrolled group studies (21, 22).
The limitations of the current study are that the patient group was small and the procedure was limited to L3 - L4, L4 - L5 and L5 - S1 levels. It should be considered that facet joints are vertical and imaging with USG may be more difficult at upper levels of the spine.
In this study, reliability of USG was compared with C-arm fluoroscopy and the results demonstrated that ultrasonography is as effective as C-arm fluoroscopy in locating the joint. USG can be considered to be a more practical and effective method than C-arm fluoroscopy for facet injections in clinics.