1. Introduction
Occupying lesions of the right atrium include vegetation, tumor, and thrombus. While thrombus is less common than vegetation and tumor, ball thrombus as a special type of thrombi is rare. Pathogenesis of ball thrombus is still unclear. It is difficult to make an accurate diagnosis before surgery (1).
2. Case Presentation
A 72-year-old female patient was admitted to our hospital with chest tightness and bilateral lower extremity edema for over three days. Physical examination revealed a blood pressure of 130/85 mmHg, heart rate of 50 beats/min, and a completely regular rhythm with varying intensities of S1 heart sound. Electrocardiogram showed atrial fibrillation with a slow ventricular rate and incomplete right bundle branch block. The patient did not have a history of surgery, trauma, or deep vein thrombosis of the lower extremity.
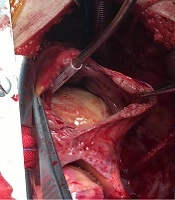
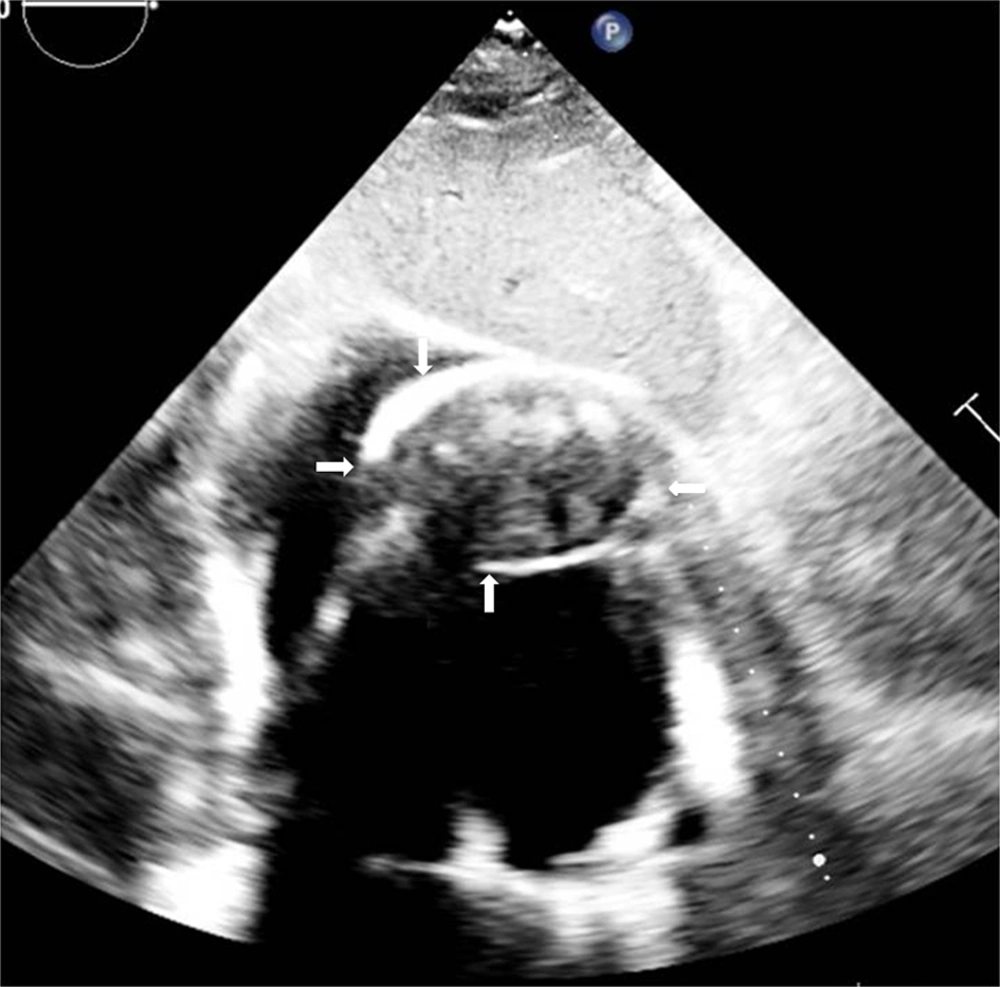
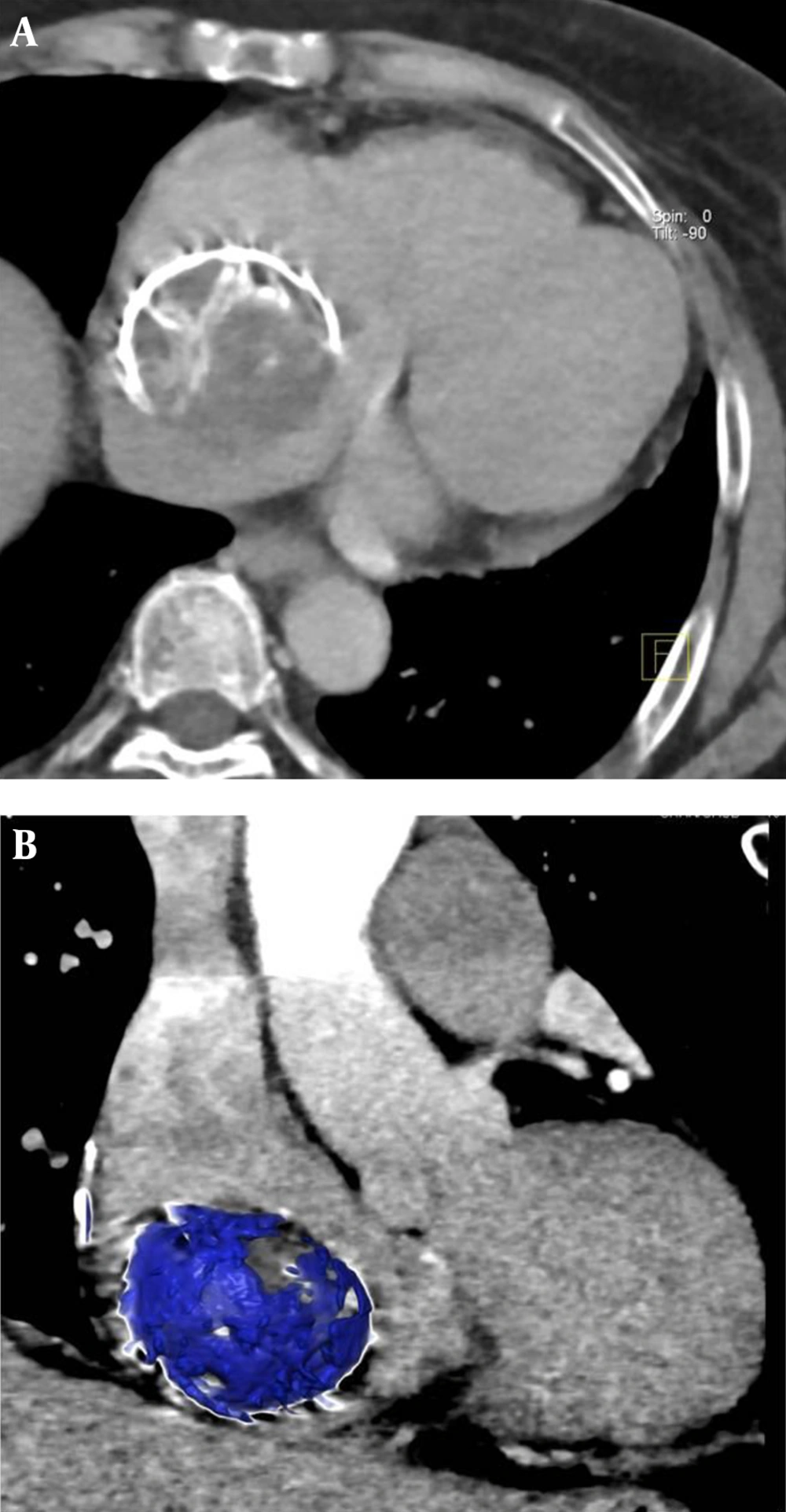
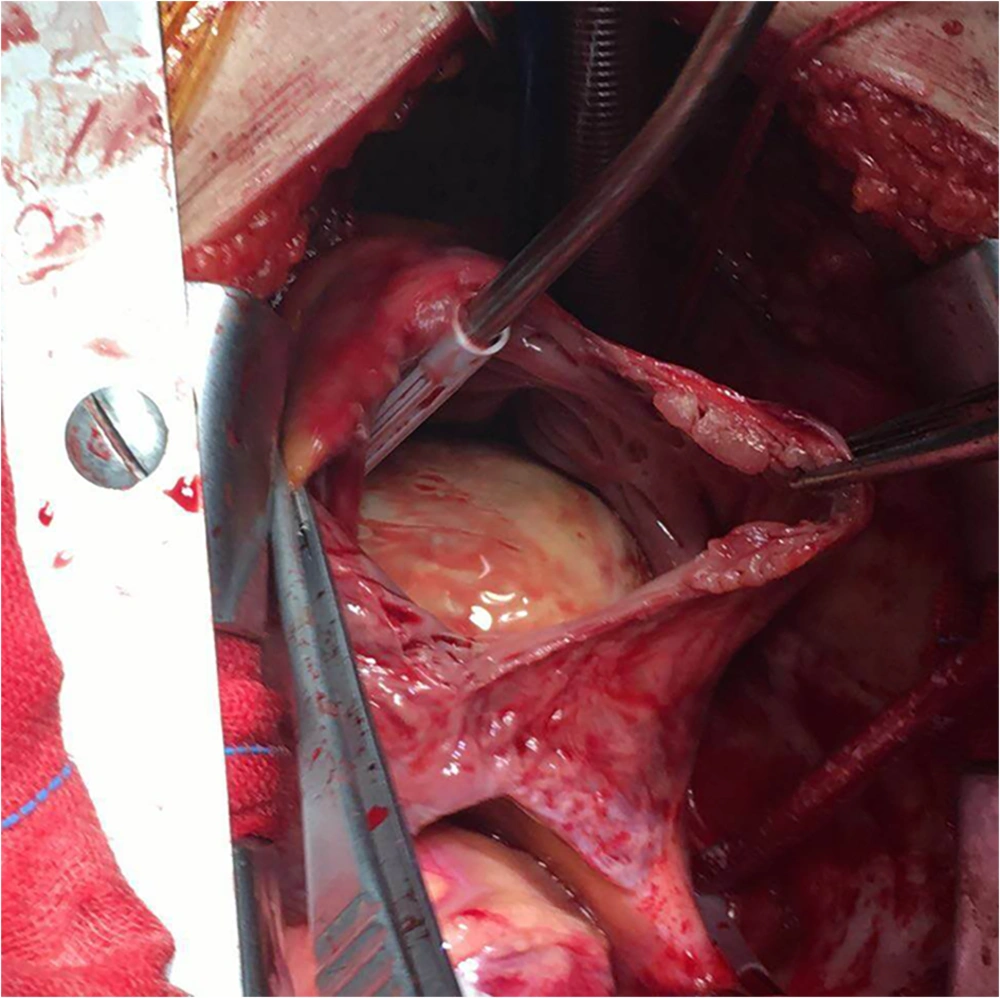
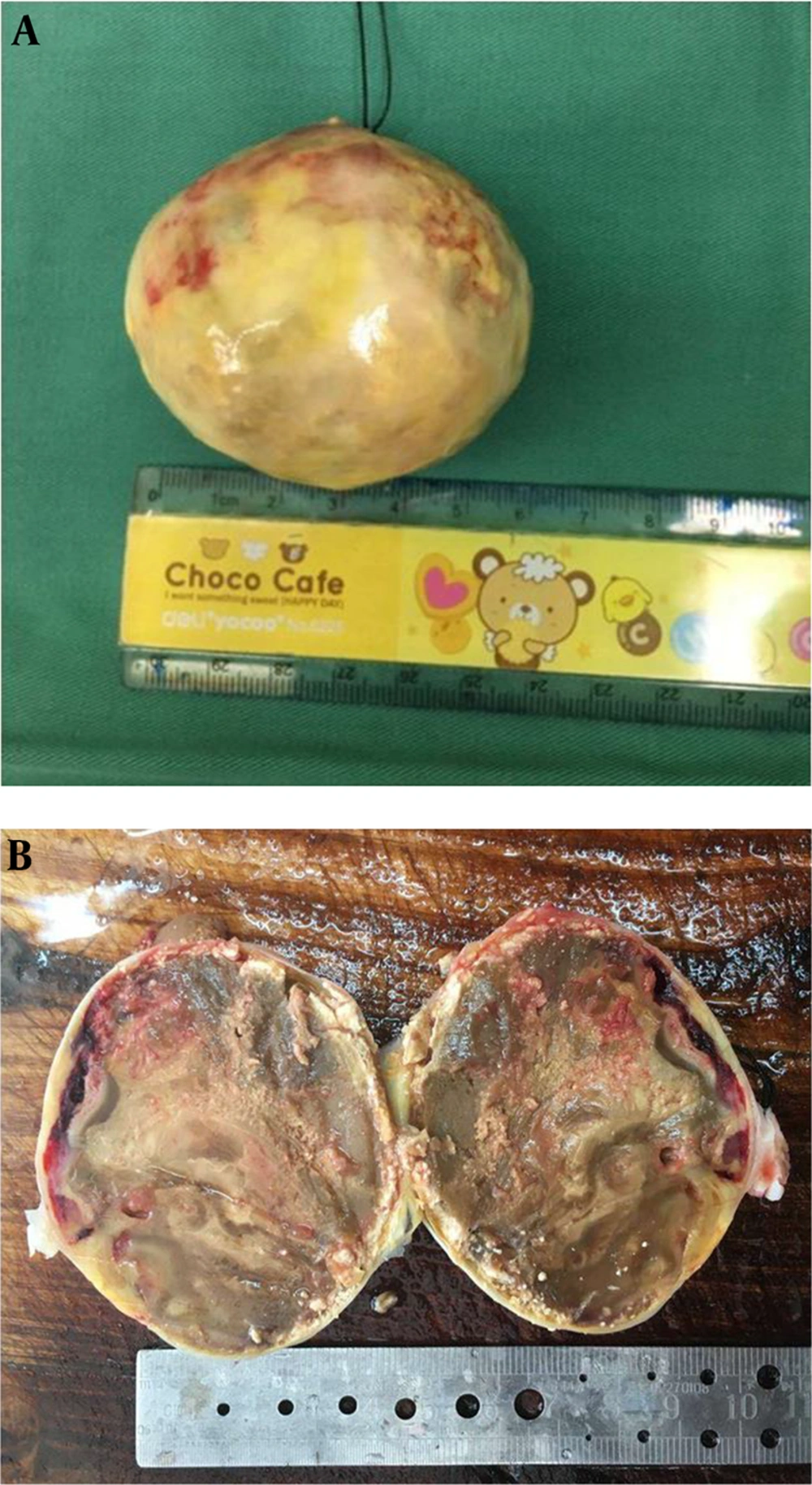
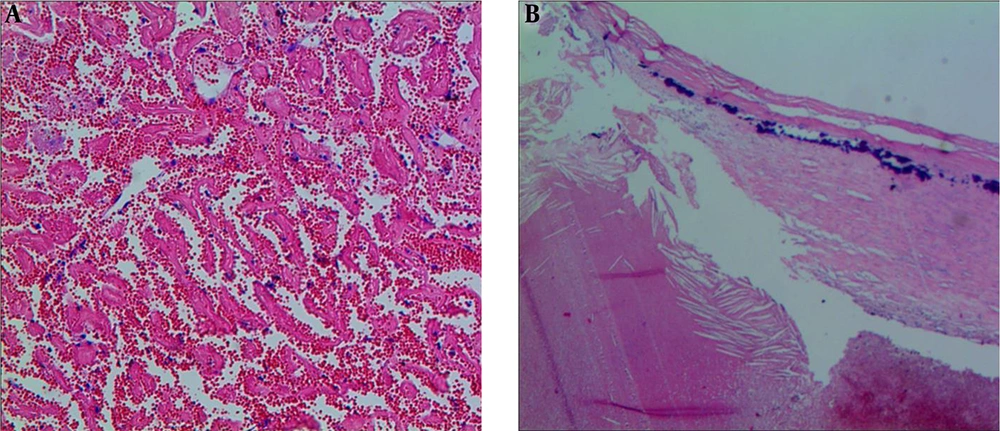
B-mode ultrasound revealed an isoechoic area of about 6 × 5.2 cm2 in the right atrium, with uneven echo isoechoic inside and annular calcifications peripherally. A connection through a tiny pedicle was found between this area and the mid-segment of the atrial septum. Moreover, there is no obvious abnormal blood flow in the upper or lower heart chambers. Mild tricuspid regurgitation was noted with a regurgitation pressure of 32 mmHg (Figure 1). With MRI claustrophobia and a long waiting time, this patient underwent CT examination. Contrast enhanced computed tomography (SOMATOM Definition Flash, Siemens Healthineers, Forchheim, Germany) found a 6 cm non-enhanced round mass with a CT value of approximately 30 HU in the right atrium. Shell-like calcifications were depicted in the mass margin (Figure 2). Based on symptoms mentioned above, the mass was considered a solid space-occupying lesion in the right atrium with suspected myxoma. Histopathological examination confirmed a 0.5 cm × 6.0 cm faint yellow, completely capsuled oval mass in the right atrium. The pedicle of the mass was attached to the atrial septum (Figure 3). The tumor was completely resected. The pathological examination showed a 6.0 cm × 5.5 cm × 4.5 cm faint yellow mass, with multiple gray spots and a smooth hard surface. On cross-section, the yellowish areas resemble necrotic tissue in the center regions, while the dark red areas are thrombotic-like tissues in the local marginal regions of the mass (Figure 4). Microscopic findings indicated nodule in a calcified fibrous capsule, necrotic tissues in the intranodular contents, thrombotic-like tissues in the margins, and the faint red nonstructural platelets constituting the trabeculae of the thrombi, which contained fibrin nets trapping a massive amount of red blood cells (Figure 5). The pathological diagnosis was right atrium thrombus with fibrous capsule and calcification. Postoperative anticoagulant medication with warfarin was prescribed to the patient, and no complication was found on discharge. During the two years of follow-up, the patient had no discomfort and was able to live independently.
A 72-year-old female with chest tightness and bilateral lower extremity edema for over three days. B-mode ultrasound indicating an oval isointense mass (white arrow) of 6 × 5.2 cm2 inside the right atrium, and this mass, with annular calcifications peripherally, was connected to the atrial septum via a tiny pedicle.
3. Discussion
Occupying lesions of the right atrium are rare, and the general causes may include vegetation, tumor, and thrombosis. Their early clinical diagnosis is difficult because corresponding clinical symptoms and/or signs may appear only when cardiac hemodynamic change, embolism following detachment of the thrombotic or tumor fragments, or tumor invasion of the pericardium occurs. Tricuspid vegetations look like the masses of the right atrium, but they are generally connected to the valve leaflets. Tumors of the right atrium may be either secondary or primary. Secondary tumors are usually metastatic, which means malignancies will spread to the right atrium along the inferior vena cava. However, primary tumors are mainly myxomas, and comprise of all the cardiac myxomas. The characteristic manifestation of right atrium myxomas is that they are attached to the atrial septum.
Thrombi in the right atrium are less common and found mainly in patients with severe right heart dysfunction, antiphospholipid syndrome, central venous catheterization, cardiac pacemaker implantation, and following repair or patch closure of atrial septal defect (2-5). Atrial fibrillation is the most dangerous factor for atrial thrombosis. The possibility of thrombosis in the right atrium is significantly lower than that in the left atrium, with an incidence rate of 0.75%. Thrombi in the right atrium are usually located at the atrial appendage or atrial wall and usually depict gelatinous or a stripe-like shape. Ball thrombi in the right atrium are uncommon, and those with calcifications are rarer. The patient in this study had a history of atrial fibrillation. However, whether this history was correlated with her current thrombus is unknown.
Pathogenesis of ball thrombus is still unclear. Grandmougin (6) found that ball thrombus in the left atrium might result from an initial free-floating or mural microthrombus, and the mass was enlarged by an accretion phenomenon. Calcification is more common in left atrium thrombi (6, 7) compared to right atrium thrombi. There are three reports of right atrium thrombi with calcifications. One was given in a patient with constrictive pericarditis complicated with atrial fibrillation (8). The second report was found in an autopsy for a patient with an indwelling central venous catheter and long-term intravenous phosphate infusion to treat osteomalacia. The result of autopsy showed multiple calcified thrombi in the superior vena cava, right atrium, and pulmonary artery. These thrombi might result from the locally excessive phosphate, leading to calcium deposition inside the thrombi (3). Besides, the third case, reported by Yamane and colleagues (9), the calcified mass was attached to the interatrial septum. They found that the calcification might degenerate from the primary tumor in the atrial septum therefore, becoming the basis of the thrombus. Moreover, the thrombus gradually increased and shaped into a ball with a smooth surface as the blood flowed inside the right atrium. In this case, a tiny pedicle from the ball thrombus was connected to the atrial septum, and shell-like calcifications appeared in the margins of the thrombus. Compared with cases reported previously, this case is valuable for the following reasons: first, after the floating thrombosis in the atrial septum, the thrombus gradually increased and shaped into a ball due to the accretion phenomenon and blood flowed into the right atrium. Second, there is a mixture of fresh and old thrombi and which were partial necrotic. Third, when the necroses were not dissolved, absorbed, or completely organized, a fibrous capsule was emerged at the surface, followed by massive calcium deposition.
The imaging manifestations described in the previous studies (3, 8, 9) were combined with this case. The calcified ball thrombus in the right atrium was characterized by the nonspecific features of the spherical shape and calcifications, and there was a higher calcification frequency in the right atrial myxoma than in the left atrial myxoma (10). Therefore, an accurate preoperative diagnosis for the right atrial ball thrombus was rather difficult as it was generally misdiagnosed as myxoma (9). In this case, the preoperative diagnoses from both the B-mode ultrasound and CT examinations for the patient indicated a high possibility of myxoma.
In summary, thrombus in the right atrium is a rare disease. We report multimodality imaging findings of thrombus in right atrium in an old woman. When a soft-tissue-like space occupying lesion in right atrium is encountered, especially with ring-like calcification, thrombus could be considered as one of the differential diagnosis.