1. Background
Pelvic radiography is a common imaging modality in pediatric orthopedics. Pelvic radiographs are essential in the diagnosis and follow-up of many pediatric orthopedic problems, including developmental dysplasia of the hip, Legg Calve Perthes disease and slipped capital femoral epiphysis.
The posterior-anterior (PA) projection as a dose reducing technique has been reported in several studies (1-4). Also the British Institute of Radiology suggested PA projection should be obtained in preference to an anterior-posterior (AP) view in order to reduce radiation exposure of gonads (5).
However, pelvic radiographs in PA projection are rarely used in daily practice due to the concern that it is not possible to shoot in the convenient position. In our literature review, we did not find any studies investigating whether pelvic radiographs obtained by PA projection in children are suitable for radiological evaluation.
2. Objectives
In this study, the aim was to determine whether PA projections meet the radiological criteria of correct positioning as AP projections.
3. Patients and Methods
For our prospective study, approval was obtained from the Institutional Review Board. All parents were followed up with a detailed description of the purpose of the research and written consent was obtained. Patients aged 5 years and younger, referred to the Pediatric Orthopedics Outpatient Clinic from May 2018 to April 2019 were included in the study. Exclusion criteria are as follows: patients with hip or knee flexion contracture above 30 degrees (they could cause increased pelvic gradient in both prone and supine positions), patients with known or clinically significant sagittal plan deformity in the spine patients scheduled for surgery (to avoid side confusion during surgery), patients whose parents refused to participate in the study.
If pelvic radiographs were required, it was decided to perform randomly with AP or PA projections. For randomization, the patients who were born on odd days of the month (including 1, 3, and 5) were scheduled to obtain pelvic radiography in the PA projection, while the patients born on even of days (including 2, 4, and 6) were planned to obtain AP projection. Age, gender, diagnosis and treatment recommendations of the patients were recorded. On physical examination, hip flexion contracture was evaluated and the amount was recorded.
The patients were divided into four groups by their age as 6 - 12 months, 1 - 2 years, 2 - 3 years and 3 - 5 years. The number of patients in the groups was determined by power analysis in order to make a proper statistical evaluation. Therefore, 20 patients in each group were found to be sufficient for the study.
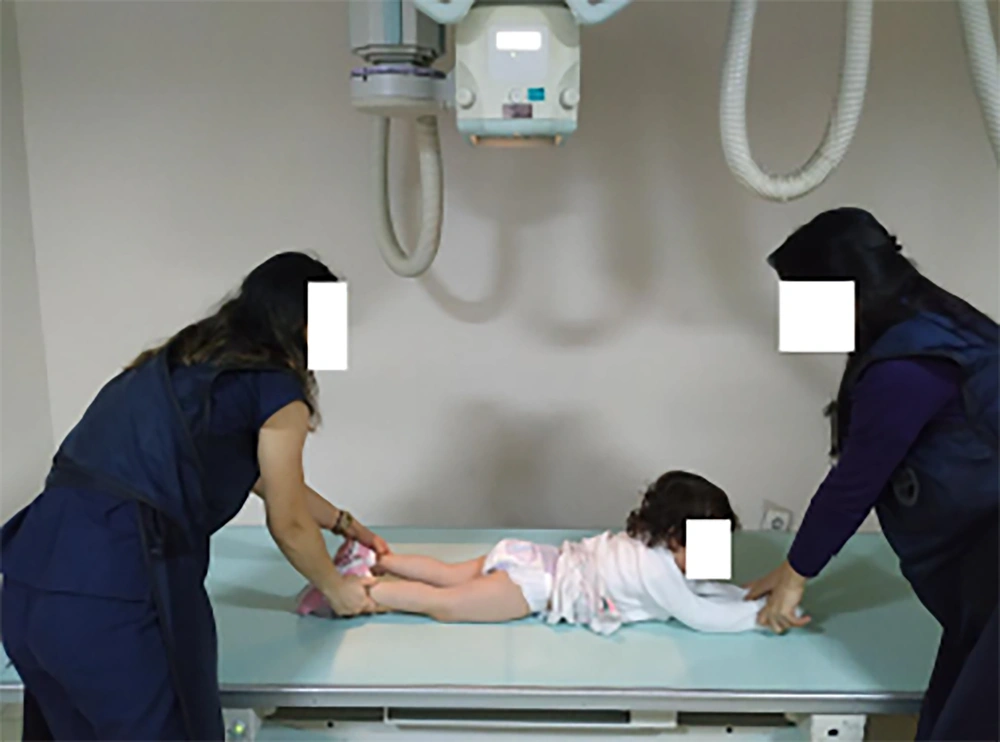
In all patients, the radiographs were taken in the standard lying down position. Patients were placed in the supine position on the cassette for AP projection and in the prone position for PA projection. The patients’ legs were held on their knees, with both lower extremities in extension and parallel to each other. The rotation of the lower extremities was adjusted to the knees and the patella parallel to the frontal plan. The patient’s trunk and legs were held in a fixed position during the shooting so that they would remain inactive (Figure 1).
In order to evaluate whether the pelvic radiographs were suitable for radiological evaluation, the criteria of “radiographic indicators of correct positioning” were used defined by Tonnis, Brunken, Ball and Kommenda (5). In order to evaluate the criteria, the rotation and tilt amount of the pelvis were determined. Accordingly, the amount of pelvic rotation was evaluated by the pelvic rotation index (PRI) and pelvic inclination was measured by the symphysis ischium angle (SIA) and pelvic inclination index (PII).
Before the measurements were made, all the information on the side of the radiographs and the projection signs and the birth dates of the patients were removed from the radiography images. Radiographs meeting all criteria were classified as ‘acceptable’ and radiographs that did not meet any of the criteria were considered as ‘unacceptable’. The radiography eligibility criteria are shown in Table 1.
| Evaluation of Pelvic Rotation | Evaluation of Pelvic Inclination | ||
|---|---|---|---|
| Parameter | Normal Range | ||
| Pelvic Rotation Index (PRI) | 1.8 - 0.56 | Symphysis Ischium Angle (SIA) | 6 - 12 months: 100 - 130 |
| 1 - 2 years: 95 - 128 | |||
| 2 - 3 years: 90 - 125 | |||
| 3 - 5 years: 85 - 115 | |||
| Pelvic Inclination Index (PII) | 1.2 - 0.75 | ||
The Pelvic Rotation Index (PRI): The ratio of the horizontal width of the obturator foramens to each other should be between 1.8 and 0.56 (Figure 2).
The Symphysis Ischium Angle (SIA): The symphysis of the upper arm and the symphysis point on both sides should be within the following limits. (Figure 3) (I) 6 - 12 months: 100° - 130°; (II) 1 - 2 years 95° - 128°; (III) 2 - 3 years 90° - 125°; (IV) 3 - 5 years 85° - 115°.
Pelvic Inclination Index (PII): The distance between the vertical width of the obturator foramen and the distance between the symphysis pubis and the Hilgenreiner line should be between 1.2 and 0.75 (Figure 4).
Statistical tests were performed with IBM SPSS (IBM Statistics for Windows, IBM Corp., released 2011, Armonk, NY). Distribution of the data was analyzed with Kolmogorov-Smirnov test. Spearman’s correlation analysis was used to evaluate the relationship between non-normally distributed variables. For intraclass correlation coefficient, values at 0.5 and below were assumed as poor, 0.5 - 0.75 as moderate, 0.75 - 0.90 as good, and 0.90 and above were assumed to be excellent agreement. The level of signi?cance was set at P < 0.05.
4. Results
A total of 160 pelvic radiographs were included in the study, 20 for each group, AP and PA projection. The mean age of the patients was 25.52 ± 15.45 (range, 6 - 60) months, and the sex distribution was 98 female and 62 male. The indications for graphs were developmental hip dysplasia in 96 (59.3%) children, pain, disability and various gait problems in 43 (26.9%) children, and Legg Calve Perthes disease, proximal femur deformities, trauma in 22 (13.7%) children. There was statistically excellent agreement in the acceptability of the pelvic radiographs taken from AP and PA projection in all age groups according to “radiographic indicators of correct positioning”.
In patients between 6 and 12 months, 16 of the radiographs in AP projection were considered as acceptable and four of the radiographs as unacceptable while 18 of the radiographs in PA projection were considered as acceptable and two of the radiographs as unacceptable (Table 2).
| AP | PA | ICC | |
|---|---|---|---|
| Acceptable/ unacceptable | Acceptable/ unacceptable | ||
| 6 - 12 months | 16/4 | 18/2 | 0.66 |
| 1 - 2 years | 16/4 | 16/4 | 1.00 |
| 2 - 3 years | 18/2 | 20/0 | 0.99 |
| 3 - 5 years | 19/1 | 18/2 | 0.99 |
Abbreviations: AP, anterior-posterior; ICC, intraclass correlation coefficient; PA, posterior-anterior.
aIntraclass correlation coefficient (ICC) = 0.95, 95% confidence interval (CI) = 0.90 - 0.98.
In patients between 1 and 2 years, 16 of the radiographs in AP projection were considered as acceptable and four of the radiographs as unacceptable; while, 16 of the radiographs in PA projection were considered as acceptable and four of the radiographs as unacceptable (Table 2).
In patients between 2 and 3 years, 18 of the radiographs in AP projection were considered as acceptable and two of the radiographs as unacceptable; while, all radiographs in PA projection were considered as acceptable (Table 2).
In patients between 3 and 5 years, 19 of the radiographs in AP projection were determined as acceptable and one as unacceptable; while, 18 of the radiographs in PA projection were determined as acceptable and two of the radiographs as unacceptable (Table 2).
5. Discussion
Radiological imaging methods are widely used in the diagnosis and follow-up of diseases in medicine. Nowadays, despite the fact that magnetic resonance imaging is like radiation-free and high-quality diagnostic tools, conventional X-ray imaging is still widely available due to its advantages such as being easily accessible, fast and inexpensive. However, radiation exposure is the most important cause of avoidance in the use of conventional methods (6). Children are more susceptible to the effects of radiation than adults due to the progressing of organ and tissue development, the small size of the body and the cumulative characteristic of radiation (7, 8). Several studies have been done to reduce radiation exposure by reducing the radiation dose or by using various barriers (9-11). A systematic review and meta-analysis by Karami et al. (12) showed that the rate of using gonad protective barrier was 58% and only 34% of these were correctly positioned. It has been reported that gonad protectors that are not properly positioned may complicate the evaluation of radiography, and therefore, the patient could be exposed to more radiation with repeated graphical shots.
The most effective way to reduce radiation exposure without additional costs is the imaging with optimized projections (1). Chaparian et al. (1) reported a decrease in radiation exposure in PA pelvic graph compared to AP graph of 25% in ovaries, 56% in the colon, 84% in the bladder, 52% in the stomach and uterus, 69% in prostate, and also showed a 60% reduction in the risk of radiation-related cancer.
An ideal graph should help to diagnose, determine the amount of pathology and guide the treatment plan. It is very important that the pelvic radiographs are taken in the convenient position to evaluate the many pathologies of the hip joint in the frontal plane and to perform various radiological measurements.
In our study, developmental hip dysplasia constitutes a large proportion of causes of pelvic radiography (59.3%). The parameters used during the diagnosis and treatment of developmental hip dysplasia, such as acetabular index, sourcil angle, and center-edge angle are significantly affected by the positioning of the graph. For example, an increase in pelvic inclination causes the acetabular index to be measured at a lower level, while its reduction leads to a higher measurement (13). Therefore, before a pelvic radiograph could be used for diagnosis and treatment, it should be evaluated whether the radiograph is convenient or not.
The criteria of “radiographic indicators of correct positioning” is generally accepted and widely used in evaluating the suitability of the pelvic radiograph. In our study, we preferred to use these criteria to evaluate the suitability of the pelvic radiographs. In our study, there was no difference in the convenience of pelvic radiographs between AP and PA projection, suggesting that in daily practice, PA projection can be used safely in child pelvic radiographs.
Changing a common practice always involves a number of risks and challenges. The biggest problem that may be encountered during pelvic radiographs is the risk of causing side error. In order not to cause a side fault, the markers indicating the side of the graph should be placed correctly and completely. Informing the radiology technicians about the patient positioning in the PA projection of the pelvis, and making the necessary changes to the pelvic radiograph in the PA projection in the digital hospital information management systems will make this practice easier to enter into daily practice.
As a result, pelvic radiography in PA projection in children is a method that reduces radiation exposure and radiation-related cancer risk significantly and does not have any disadvantage compared to AP projection. The use of PA projection of pelvic radiograph should be encouraged and increased in daily practice.