1. Background
In December 2019, China encountered a deadly respiratory disease caused by a new coronavirus, which spread worldwide in the first half of 2020. The virus was called Severe Acute Respiratory Syndrome Coronavirus 2 or SARS-CoV-2, which causes Coronavirus Disease-19 or COVID-19 (1, 2). The epidemic has had many social and economic consequences, especially for public health systems (3, 4), and the rapid spread of COVID-19 has affected many aspects of human life. Despite all efforts to control the pandemic, the disease has had a significant mortality rate. Iran is among the most affected countries, in which COVID-19 has infected approximately 5.6 million people and a death toll of 121 thousand (5). Managing this pandemic in Iran has been difficult due to recent economic crises and sanctions (6, 7). Right now, the best way to defeat COVID-19 is to get vaccinated, which we hope will effectively end the pandemic.
The level of acceptance and coverage has been evaluated in studies conducted worldwide and in Iran, which have shown that these two are the main and vital elements in creating the success of the immunization program (8, 9). Based on the research results, there are concerns and skepticism about vaccination among people in different communities (10), and the World Health Organization has defined them as refusing vaccination factors, despite the availability of safe vaccines (11). Hesitation in accepting the COVID-19 vaccine can have irreversible consequences. Health policymakers and managers need to address serious concerns about not achieving an acceptable level of immunity against COVID-19 and take action on effective policies on COVID-19 vaccination. According to research, the country origin of the vaccine production influences acceptance (12). A study conducted in Brazil shows high resistance to vaccines produced in China and Russia compared to vaccines manufactured in the United States and Britain (13).
Estimating the level of COVID-19 vaccine acceptance among Iranians is essential for policymaking. Additionally, the COVID-19 vaccine acceptance level and the reliance on the media sources used to obtain the pandemic information are important.
2. Objectives
The present study aimed to estimate the willingness to accept currently approved COVID-19 vaccines and the factors affecting it among Isfahan University of Medical Sciences students.
3. Methods
This population-based cross-sectional study was conducted on 342 Isfahan University of Medical Sciences students (medicine, dentistry, pharmacy, and bachelor's, master's, and Ph.D. students in various medical fields). They were chosen by convenience sampling, and data were collected using an electronic questionnaire in June-July 2021.
Inclusion criteria were age over 18 years and studying at Isfahan University of Medical Sciences. No consent was obtained as the data were collected and analyzed anonymously.
3.1. Study Variables
We questioned primary demographic information, including age, gender, degree, study field, academic year, marital status, socioeconomic status, number of family members, level of access to physicians and nurses, employment status, history of COVID-19 infection of themselves and their family, history of traveling or gathering in the past month with close and distant relatives, and source of information regarding COVID-19.
Participants were asked how much they agreed with the statements regarding COVID-19 protection protocols adherence, and the answers were scored based on a five-point Likert Scale: 1 = strongly disagree to 5 = strongly agree. In order to measure the socioeconomic status, we converted the 10-digit socioeconomic status score into four categories (less than 2, 2 - 6, 6 - 10, and more than 10 million Tomans). The power of COVID-19 infection risk estimation was assessed with two 3-point Likert questions (how likely are you to get COVID-19? How much are your peers at risk of COVID-19?). We used a previously validated short form (12 questions) to evaluate the level of vaccine acceptance, awareness of vaccines effectiveness from the students 'point of view, attitude and practice toward COVID-19 vaccines, and the level of hope for the control of COVID-19. Participants answered the questions on a five-point scale (1: strongly agree to 5: strongly disagree). The range of scores in this questionnaire was 12 to 60. The validity and reliability of this questionnaire have been shown in other studies (14-17). We used a previously validated short form of 16 questions (1: correct option - 0: incorrect options) to assess students' knowledge of COVID-19. One question in the awareness section was multiple-choice, which is why the score range obtained in the awareness questionnaire was 0 to 21.
3.2. Data Analysis
Descriptive statistics (frequency and percentage) were calculated for the demographic characteristics and acceptance of COVID-19 vaccines. For susceptibility analysis, weight analysis was performed for COVID-19 vaccine acceptance using student demographics.
Average and standard deviation were used to describe the characteristics of the participants for quantitative variables and frequency and percentage for qualitative variables. In analyzing two variables, according to the presuppositions of the parametric test - normality of the data and uniformity of variances - an independent t-test was used to test the continuous variables. The chi-square test was also used for class variables. Multiple logistic regression was used to estimate the adapted odds ratio (OR) and 95% confidence interval. According to the bivariate analysis results, age group, gender, level of education, marital status, employment status, perception of COVID-19 infection risk, travel in the last month, time spent in the last month with close relatives, and multiple logistics logs were entered in the regression model. The final model processing was evaluated using Hosmer-Lemeshow statistics. Data analysis was performed using SPSS software.
4. Results
Among 324 students who participated in this study, 60.9% were older than 20 years, 68% were female, 87.5% were single, 50.2% were members of the medical department (medicine, dentistry, and pharmacy), and 14.1% were employed. Additionally, 43.1% had a positive history of COVID-19 infection since the last month. The primary source of information in 86.2% of students was the internet or social networks, friends, or TV, while 13.8% of students mentioned scientific sources, including books, articles, university professors, or medical doctors and nurses. The mean ± SD scores of knowledge, attitude, practice, admissibility, and understanding of risk among all students were 11.5 ± 2.1, 8.2 ± 1.4, 25.0 ± 3.8, 10.8 ± 2.0, and 4.0 ± 1.1, respectively. Considering the maximum possible score in each scale, students had relatively high scores of attitude, practice, and understanding of risk, while low to moderate knowledge and admissibility scores.
Table 1 shows the average score of knowledge, attitude, practice, admissibility, and perception of risk among different study groups. Perception of risk was significantly higher in the male group (P < 0.001) and students with a doctoral degree (P = 0.001). Average scores of attitude and practice were higher in females (P = 0.004 and P = 0.001), and in the area of risk perception, the scores were higher in ages > 20 (P = 0.001).
| Groups | Knowledge | Attitude | Practice | Admissibility | Understanding Risk |
|---|---|---|---|---|---|
| Age | |||||
| ≤ 20 (N = 128) | 11.3 ± 2.1 | 8.3 ± 1.3 | 25.5 ± 3.6 | 10.6 ± 2.0 | 3.8 ± 1.1 |
| > 20 (N = 196) | 11.6 ± 2.1 | 8.1 ± 1.4 | 24.8 ± 3.8 | 10.8 ± 2.1 | 4.2 ± 1.1 |
| P-value b | 0.128 | 0.119 | 0.124 | 0.273 | 0.001 |
| Sex | |||||
| Female (n = 219) | 11.2 ± 2.0 | 8.4 ± 1.3 | 25.6 ± 3.3 | 10.8 ± 1.9 | 4.1 ± 1.1 |
| Male (n = 105) | 12.1 ± 2.2 | 7.9 ± 1.5 | 24.1 ± 4.3 | 10.7 ± 2.4 | 3.9 ± 1.2 |
| P-value b | < 0.001 | 0.004 | 0.001 | 0.841 | 0.085 |
| Education level | |||||
| Non-medical (n = 170) | 11.1 ± 2.0 | 8.3 ± 1.3 | 25.4 ± 3.8 | 10.8 ± 2.2 | 4.0 ± 1.1 |
| Medical c (n = 154) | 11.9 ± 2.1 | 8.1 ± 1.4 | 24.8 ± 3.6 | 10.6 ± 2.0 | 4.1 ± 1.1 |
| P-value b | 0.001 | 0.157 | 0.184 | 0.347 | 0.491 |
| Marital status | |||||
| Single (n = 286) | 11.5 ± 2.1 | 8.2 ± 1.4 | 25.2 ± 3.7 | 10.7 ± 2.1 | 3.9 ± 1.1 |
| Married/divorced (n = 38) | 11.7 ± 2.3 | 8.5 ± 1.3 | 24.0 ± 3.4 | 10.7 ± 1.9 | 4.8 ± .9 |
| P-value b | 0.596 | 0.241 | 0.057 | 0.994 | < 0.001 |
| Income | |||||
| < 2 M (n = 42) | 11.5 ± 2.3 | 8.0 ± 1.5 | 24.9 ± 4.3 | 11.2 ± 2.2 | 4.1 ± 1.2 |
| 2 - 6 M (n = 98) | 11.1 ± 2.1 | 8.2 ± 1.2 | 25.2 ± 3.6 | 10.5 ± 2.2 | 4.1 ± 1.1 |
| 6 - 10 M (n = 104) | 11.7 ± 2.0 | 8.2 ± 1.3 | 24.8 ± 3.7 | 10.9 ± 2.0 | 4.1 ± 1.1 |
| > 10 M (n = 80) | 11.7 ± 2.0 | 8.3 ± 1.5 | 25.4 ± 3.6 | 10.7 ± 2.1 | 4.0 ± 1.2 |
| P-value d | 0.246 | 0.740 | 0.672 | 0.221 | 0.934 |
| Job | |||||
| Yes (n = 46) | 11.6 ± 2.2 | 8.4 ± 1.4 | 24.4 ± 3.6 | 10.7 ± 2.0 | 4.6 ± 1.1 |
| No (n = 278) | 11.5 ± 2.1 | 8.2 ± 1.4 | 25.2 ± 3.7 | 10.7 ± 2.1 | 3.9 ± 1.1 |
| P-value b | 0.641 | 0.332 | 0.155 | 0.988 | 0.001 |
| Recent COVID | |||||
| Yes (n = 140) | 11.4 ± 2.2 | 8.1 ± 1.5 | 24.6 ± .1 | 10.7 ± 2.1 | 4.1 ± 1.1 |
| No (n = 184) | 11.5 ± 2.0 | 8.3 ± 1.3 | 25.5 ± 3.3 | 10.8 ± 2.1 | 4.0 ± 1.1 |
| P-value b | 0.632 | 0.360 | 0.023 | 0.708 | 0.821 |
| Source of information | |||||
| Scientific (n = 43) | 11.4 ± 2.3 | 8.4 ± 1.4 | 25.6 ± 3.2 | 10.5 ± 2.4 | 4.1 ± 1.1 |
| Others (n = 281) | 11.5 ± 2.1 | 8.2 ± 1.4 | 25.0 ± 3.8 | 10.8 ± 2.0 | 4.0 ± 1.1 |
| P-value b | 0.814 | 0.394 | 0.340 | 0.367 | 0.372 |
a Values are expressed as mean ± SD.
b Results of independent t-test.
c Medicine, pharmacy, dentistry.
d Results of ANOVA.
e Maximum possible score for: Knowledge: 20; attitude: 10; practice: 30; acceptability: 20; understanding risk: 6.
The frequency and percentage of acceptability are compared among various groups in Table 2. The percentage of acceptability was significantly higher in the medical students' group (P = 0.002). In addition, a significant correlation was observed between vaccine acceptability and admissibility (P < 0.001). However, no significant correlations were observed in any other subgroups.
| Groups | Acceptability a No. (%) | P-Value | |
|---|---|---|---|
| Yes | No | ||
| Age | 0.584 b | ||
| ≤ 20 | 116 (39.1) | 12 (44.4) | |
| > 20 | 161 (60.9) | 15 (55.6) | |
| Sex | 0.668 b | ||
| Female | 202 (68) | 17 (63) | |
| Male | 95 (32) | 10 (37) | |
| Education level | 0.002 b | ||
| Non-medical | 148 (49.8) | 22 (81.5) | |
| Medical | 149 (50.2) | 5 (18.5) | |
| Marital status | 0.342 c | ||
| Single | 260 (87.5) | 26 (96.3) | |
| Married/divorced | 37 (12.5) | 1 (3.7) | |
| Income | 0.806 d | ||
| < 2 M | 38 (12.8) | 4 (14.8) | |
| 2 - 6 M | 88 (29.6) | 10 (37) | |
| 6 - 10 M | 97 (32.7) | 7 (25.9) | |
| > 10 M | 74 (24.9) | 6 (22.2) | |
| Job | 1.000 c | ||
| Yes | 42 (14.1) | 4 (14.8) | |
| No | 255 (85.9) | 23 (85.2) | |
| Recent COVID | 0.892 b | ||
| Yes | 128 (43.1) | 12 (44.4) | |
| No | 169 (56.9) | 15 (55.6) | |
| Understanding risk | 0.909 b | ||
| Low | 71 (23.9) | 7 (25.9) | |
| Moderate | 156 (52.5) | 13 (48.1) | |
| High | 70 (23.6) | 7 (25.9) | |
| Source of information | 0.553 c | ||
| Scientific | 41 (13.8) | 2 (7.4) | |
| Others | 256 (86.2) | 25 (92.6) | |
| Knowledge | 0.167 b | ||
| Low | 7 (2.4) | 1 (3.7) | |
| Moderate | 266 (89.6) | 21 (77.8) | |
| High | 24 (8.1) | 5 (18.5) | |
| Attitude | 0.455 d | ||
| Low | 2 (0.7) | 0 (0.0) | |
| Moderate | 71 (23.9) | 9 (33.3) | |
| High | 224 (75.4) | 18 (66.7) | |
| Practice | 0.562 d | ||
| Low | 1 (0.3) | 0 (0.0) | |
a Willingness to get vaccinated.
b Results of chi-square test.
c Results of Fisher's exact test.
d Results of Freeman-Halton extension of Fisher's exact test.
Table 3 shows the multiple logistic regression model results for vaccine acceptability as an independent variable. Among all included factors in the model, only the level of education showed a significant association with the outcome of interest. Students with a higher level of admissibility had around 2.2 times higher acceptability adjusted for other associated factors (OR = 2.210; 95% CI: 1.647 - 2.966). The Hosmer-Lemeshow test showed the goodness of fit for the model (P = 0.727).
| Variables | P-Value | OR | 95% CI for OR | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age group | ||||
| ≤ 20 | - | - | - | - |
| > 20 | 0.308 | 0.629 | 0.258 | 1.534 |
| Sex | ||||
| Female | - | - | - | - |
| Male | 0.125 | 2.069 | 0.817 | 5.240 |
| Education level | ||||
| Non-medical | - | - | - | - |
| Medical | 0.001 | 0.153 | 0.049 | 0.479 |
| Marital status | ||||
| Single | - | - | - | - |
| Married/divorced | 0.237 | 0.262 | 0.028 | 2.419 |
| Income | ||||
| < 2 M | - | - | - | - |
| 2 - 6 M | 0.907 | 0.925 | 0.250 | 3.419 |
| 6 - 10 M | 0.496 | 0.624 | 0.160 | 2.430 |
| > 10 M | 0.988 | 1.011 | 0.244 | 4.182 |
| Job | 0.685 | 0.774 | 0.225 | 2.668 |
| Recent COVID-19 | 0.880 | 0.937 | 0.405 | 2.171 |
| Source of information | ||||
| Scientific | - | - | - | - |
| Others | 0.889 | 0.366 | 2.026 | 0.439 |
| Knowledge | 0.666 | 0.954 | 0.769 | 1.183 |
| Attitude | 0.169 | 0.788 | 0.562 | 1.106 |
| Practice | 0.827 | 1.016 | 0.883 | 1.168 |
| Admissibility | <0.001 | 2.210 | 1.647 | 2.966 |
| Understandingrisk | 0.368 | 0.832 | 0.557 | 1.242 |
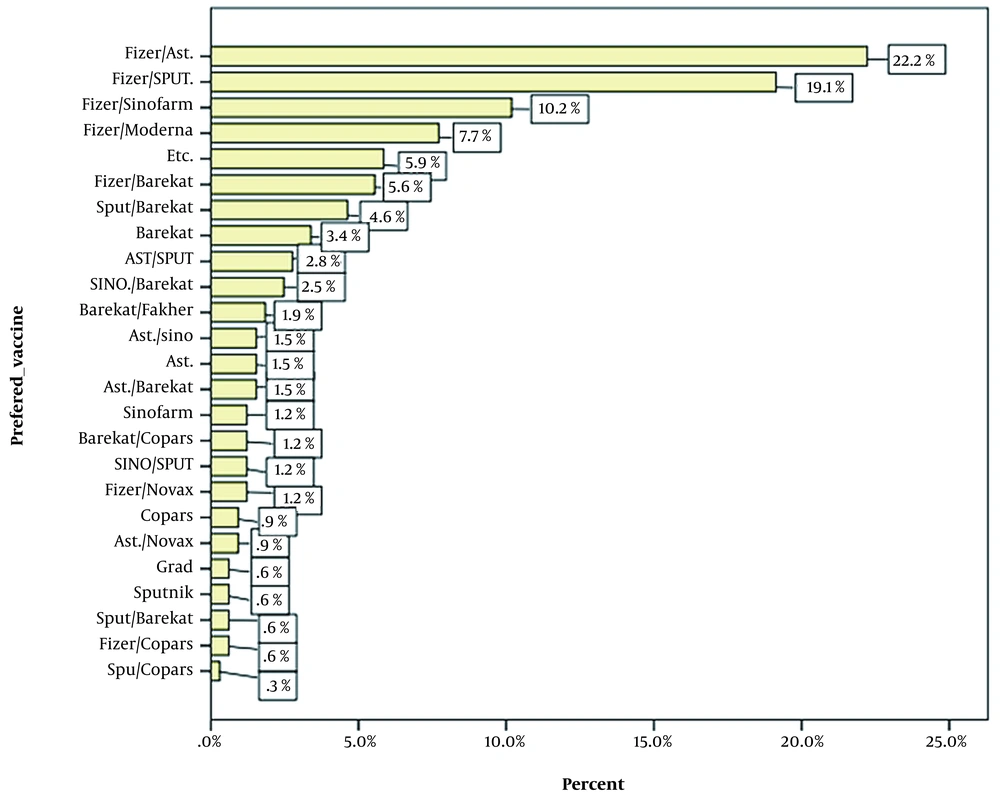
Figure 1 shows the willingness of participants to receive different vaccines. Participants could choose from a maximum of two options. The most popular was Pfizer-BioNTech COVID-19 vaccine (USA), and the least was Bharat Biotech's BBV152/Covaxin (India). According to our survey, the Oxford-AstraZeneca COVID-19 vaccine was reported to have the highest tendency to receive among the vaccines approved by the Ministry of Health and Medical Education of Iran.
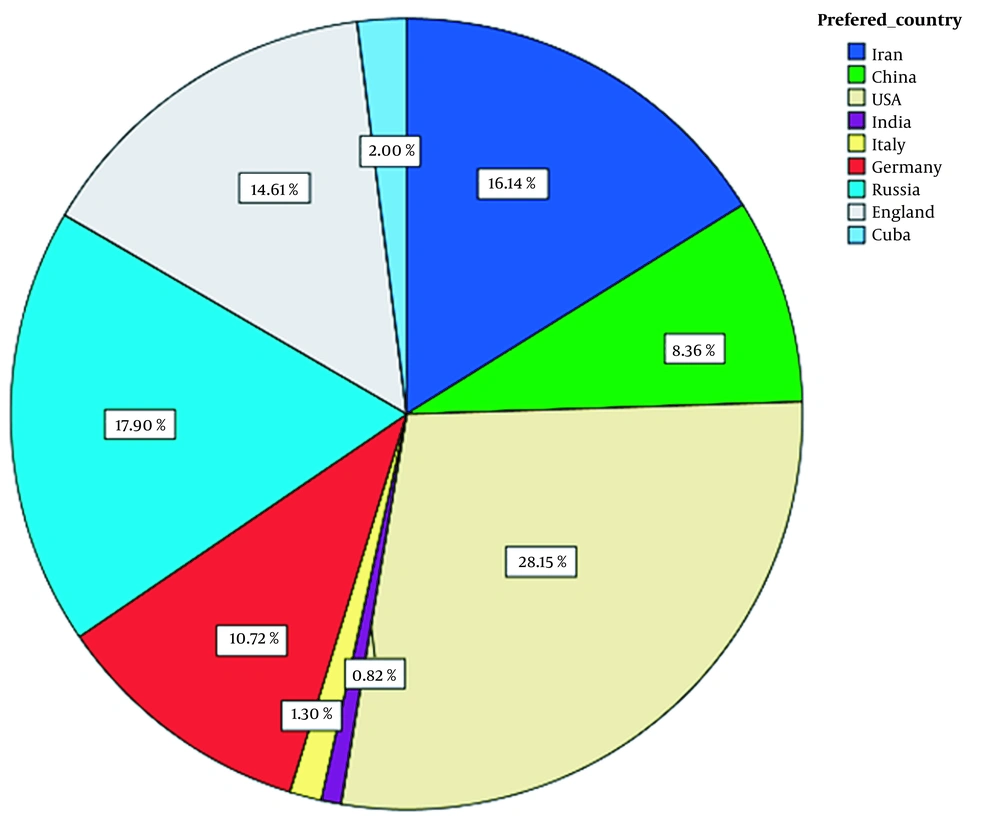
The study of participants' willingness to receive different vaccines based on their country of the manufacturer is shown in Figure 2. The rankings based on the country of the vaccine manufacturer were the United States (28.15%), Russia (17.90%), and Iran (16.14%), respectively. The lowest willingness was to receive vaccines developed in India (0.82%). Therefore, one of the reasons for the low willingness of participants to get Bharat Biotech's BBV152/Covaxin could be considered the low acceptance of the country of the manufacture.
5. Discussion
In our study, 91.7% of the participants were willing to accept COVID-19 vaccines for themselves and their families. Compared to the results of studies in Iran and other countries, the level of vaccine acceptance among Isfahan University of Medical Sciences students could be considered acceptable. According to a study conducted from February to April 2020 in the cities of Tehran and Kermanshah, the level of vaccine acceptance among the general population of these two cities was 66.47% (17). Most of the studies conducted worldwide are on the general population of different countries, where the highest frequency of COVID-19 vaccination has been observed in Ecuador (97%) (18), Malaysia (94.3%) (19), Indonesia (93.3%) (20), and China (91.3%) (21). It can also be concluded that the level of vaccine acceptance among students, who are a significant proportion of the Iranian population, has increased over the past year due to advances and scientific reports on COVID-19 vaccines. Therefore, considering the importance and effectiveness of this group in Isfahan, it can be stated that the high level of vaccine acceptance in the academic community is a promising sign for this province.
Some studies have shown a significant relationship between vaccine acceptance behavior and age (22, 23), but we did not find any significant relationship between the age of participants (18 - 45 years) and vaccine acceptance; so, we confirmed the results of a study conducted by Al-Mohaithef and Padhi (24) in April 2021 to July 2021, which stated that almost all age groups have the same chance of admission. Our data also confirmed other study results, including the lack of a significant relationship between participants' gender and vaccine acceptance behavior.
According to the results, the tendency to accept vaccines significantly correlates with education level and admissibility. Medical sciences students (including medical, pharmacy, and dental students) have become more conservative than non-medical students, which might be due to their clinical background and care more about their health, so they are more inclined to accept the vaccine. People's trust in healthcare providers is undeniable. Therefore, this group should know the benefits and risks of vaccination to advise patients, healthcare professionals, family, friends, and others. The COVID-19 pandemic has once again shown the importance of their role in people's education and adherence to medical procedures.
Examining the data, we found that participants were more likely to receive Pfizer-BioNTech and Oxford-AstraZeneca COVID-19 vaccines, in sequence. The high choice of the Pfizer-BioNTech COVID-19 vaccine could be attributed to the extensive research on vaccine, platform (mRNA-based), and higher efficacy against COVID-19 (25). This prioritization was also somewhat true in vaccine-producing countries, with the United States again in the lead.
5.1. Strengths and Limitations of the Study
The present population-based study describes the tendency to accept COVID-19 vaccines and related factors among Isfahan University of Medical Sciences students. In order to generalize the results of the present study to the entire population of medical students in Iran, the cultural differences in other cities and the students living in rural areas versus metropolitan areas should be considered. Considering the period of the study and the existence of contradictory news about the effectiveness and safety of the existing vaccines and considering the status of the incidence compared to the peak periods of the disease in Iran, we must consider the possibility of affecting the study results. Finally, due to the cross-sectional nature of the study design, causal inference cannot be deduced from the relationships obtained in the present study.
5.2. Conclusions
The study results showed the acceptable level of admissibility and willingness to accept COVID-19 vaccines among Isfahan University of Medical Sciences students (Table 3) and predicted that students could positively affect people's attitudes toward COVID-19 vaccines. For future studies, the followings are suggested: (1) assessing the willingness to accept the vaccine in specific and more broad groups of society; (2) identifying and evaluating other factors associated with the willingness to accept the COVID-19 vaccines; (3) identifying vulnerable subgroups of society to perform efficient and effective educational interventions; (4) using the vaccination prioritization strategy based on variables affecting the willingness to accept the vaccine to achieve the herd immunity in community faster, due to the continuous mutation of SARS-CoV-2 in a short time; and (5) preventing misinformation about COVID-19 vaccines in collaboration with the state-run mass media and cyberspace. Medical students are the community's medical staff, and they must continue to play a leading and educational role in combating the epidemic as the most reliable source for increasing vaccine acceptance in the community.