1. Background
Local anesthetics in awake patients are an appropriate alternative to general anesthetics for infants undergoing lower abdominal, urinary tract, and lower extremity surgeries. Its benefits include a low incidence of postoperative apnea and avoiding exposure to anesthetics that may increase the incidence of neuro-apoptosis and unwanted neurological outcomes (1). Adding epinephrine to local anesthetics in the caudal block is one of the common methods; however, hemodynamic changes and cardiovascular parameters induced by epinephrine in this method have not been studied well. Epinephrine can prolong the duration of caudal block and can act as an indicator to avoid intravascular injection (2).
Caudal anesthesia has many advantages over general anesthesia in children undergoing inguinal hernia repair surgery (3). Topical anesthesia for surgical procedures in newborns has many benefits, including maintaining the patient's respiratory conditions and rapid return to nutrition (4). Many factors contribute to optimizing pediatric pain management. Recent evidence suggests that severe pain can affect children more significantly than adults (5). Local anesthetics and analgesics have improved the patients' outcomes of surgical treatment and may be the preferred method for premature neonates and infants, pediatric patients with neuromuscular disorders, or feeding children candidates for emergency surgeries (6).
The complications of caudal block in children are based on the findings from an observational study on the use of local anesthesia in children, including unsuccessful blocking, accidental rupture of vessels or dura mater, intravascular injection of the test dose, seizure, cardiac arrest, sacrum pain, and neurological symptoms (7). The systemic toxic effect of local anesthetics is rare but potentially life-threatening, primarily due to incorrect intravascular injection. High blood levels of local anesthetics can lead to cardiovascular and central nervous system toxicities. Intravascular injection occurs in about 1.3 to 10.000 caudal blocks. Lipid emulsions are used to treat local anesthetic toxicity (8).
2. Objectives
This study aimed to evaluate the cardiovascular effects of epinephrine in caudal epidural injection by assessing ECG, heart rate, and blood pressure to ensure the safety of epinephrine injection in the caudal epidural block.
3. Methods
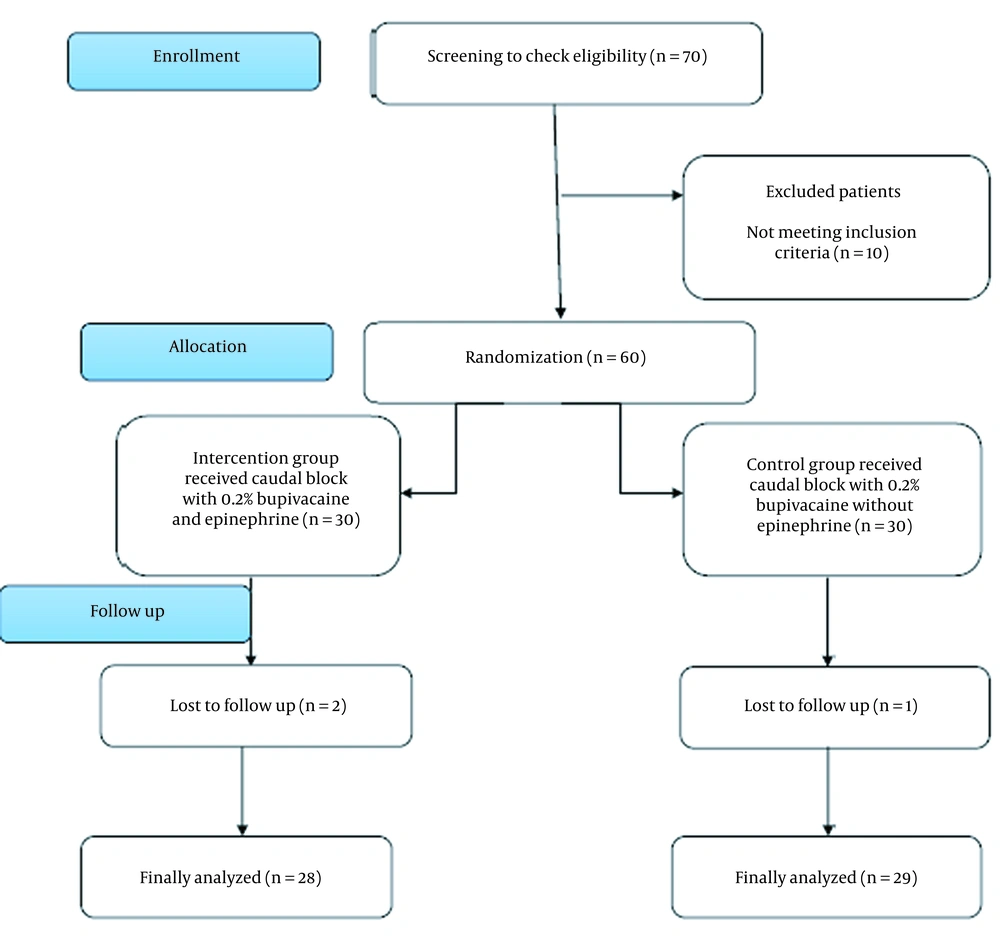
This double-blind, randomized clinical trial was conducted on pediatrics aged under six with ASA I and II who were candidates for elective sub-umbilical surgery (including lower abdominal surgery and urinary tract) in a children's hospital in Tabriz. Exclusion criteria were children with ASA III or more and patients who were candidates for emergency inguinal hernia repair surgery. Patients were allocated randomly into two equal groups of 30 using random allocation software. The intervention group received a caudal block with epinephrine, and the control group received a caudal block without epinephrine under general anesthesia with midazolam 0.05 mg/kg, fentanyl 1 µg/kg, lidocaine 1 mg/kg, and propofol 3 mg/kg. Laryngeal mask airway (LMA) with suitable size was inserted for patients to manage the airways. Anesthesia was maintained by assisted spontaneous ventilation with sevoflurane, oxygen, and N2O. Then, the patients were placed in the lateral decubitus position, and the caudal block with a Gauge 22 needle was performed from the space of the sacral hiatus. Patients in the intervention group were under the block with 1 mL/kg of the solution containing bupivacaine 0.2% and epinephrine 5 µg/kg at a concentration of 1/200000. In contrast, the control group was under the block with simple bupivacaine without epinephrine (Figure 1). The patients, their parents, and the anesthesiologist were blinded to grouping, and the drugs were prepared by anesthesia nurses. The ECG, heart rate (HR), and blood pressure (BP) were measured by monitoring the groups before the block. Then, the caudal block was performed. The ECG, HR, and BP were measured in both groups at the first, fifth, and 20th minutes after the caudal block. The data were collected in worksheets and then were statistically analyzed. The sample size was calculated based on the mean heart rate in a previous study (9) with 95% CI and 80% power. Finally, 30 patients were designated for each group.
The research followed the tenets of the Declaration of Helsinki. The Ethics Committee of Tabriz University of Medical Sciences approved the study with the code IRTBZMED.REC.1396.1236. Written informed consent was taken from all participants' parents before any intervention. This trial was registered in the Iranian registry of clinical trials (IRCT) with the code IRCT20100527004041N15.
3.1. Statistical Analysis
Continuous variables were presented as mean ± SD, and categorical variables as numbers and percentages. The baseline characteristics were compared between the intervention and control groups using the Person's chi-square test for categorical variables and the independent t-test for continuous variables. The mean hemodynamic variables in the first, fifth, and 20th minutes were compared using repeated measurements between the two groups. Data analysis was performed using SPSS version 17, and a P value < 0.05 was considered significant.
4. Results
This study aimed to determine the cardiovascular effects of adding epinephrine to local anesthetic drugs in 60 children under caudal epidural block for sub-umbilical surgeries that were equally divided into two groups of 30. Finally, 28 (93.3%) patients in the intervention group and 29 (96.7%) in the control group were analyzed (Figure 1).
As shown in Table 1, the groups did not differ in the age distribution (P = 0.07). Also, there was no statistically significant difference in the mean weight (P = 0.11) and ASA classification (P = 0.66) of children between the two groups.
| Variables | Intervention Group | Control Group | P Value |
|---|---|---|---|
| Age group | 0.07 | ||
| Less than 6 months | 4 (13.3) | 11 (36.7) | |
| 6 to 11 months | 4 (13.3) | 5 (16.7) | |
| 1 to 6 years | 22 (73.3) | 14 (46.7) | |
| Weight (kg) | 0.11 | ||
| 1 - 5 | 2 (6.7) | 6 (20) | |
| 6 - 10 | 12 (40) | 15 (50) | |
| > 10 | 16 (53.3) | 9 (30) | |
| ASA | 0.06 | ||
| I | 26 (86.7) | 20 (66.7) | |
| II | 4 (13.3) | 10 (33.3) |
Comparison of Demographic Characteristics Between Two Groups a
In Table 2, there were no significant differences between the groups at baseline in the mean systolic (P = 0.82), diastolic (P = 0.38), and arterial (P = 0.92) blood pressure and heart rate (P = 0.21).
| Intervention Group | Control Group | P Value | |
|---|---|---|---|
| Systolic blood pressure (mmHg) | 87.20 ± 8.27 | 86.60 ± 12.49 | 0.82 |
| Diastolic blood pressure (mmHg) | 48.43 ± 8.83 | 50.83 ± 12.11 | 0.38 |
| Mean arterial blood pressure (mmHg) | 11.01 ± 62.30 | 62.56 ± 11.79 | 0.92 |
| Mean heart rate (bpm) | 21.34 ± 131.20 | 138.86 ± 25.59 | 0.21 |
Comparison of Baseline Hemodynamics Between Two Groups
The mean systolic, diastolic, and arterial blood pressure (mmHg) and heart rate in the first, fifth, and 20th minutes are presented in Table 3. There was no significant difference in the mean arterial BP between the two groups. The heart rate in the first minute significantly differed between the two groups (P = 0.03). However, there was no significant difference between the groups in the mean heart rate in the fifth and 20th minutes after anesthesia.
| Variables and Time (After Anesthesia) | Intervention Group | Control Group | P Value |
|---|---|---|---|
| Systolic blood pressure (mmHg) | |||
| 1st minute | 84.60 ± 9.33 | 62.56 ± 11.79 | 0.92 |
| 5th minute | 80.90 ± 7.08 | 77.53 ± 8.00 | 0.09 |
| 20th minute | 77.73 ± 7.31 | 74.43 ± 7.94 | 0.1 |
| Diastolic blood pressure (mmHg) | |||
| 1st minute | 45.8 ± 8.37 | 47.60 ± 12.36 | 0.51 |
| 5th minute | 41.66 ± 3.45 | 41.66 ± 6.84 | > 0.999 |
| 20th minute | 37.93 ± 5.73 | 38.90 ± 7.19 | 0.56 |
| Mean arterial blood pressure (mmHg) | |||
| 1st minute | 58.23 ± 8.39 | 57.96 ± 6.82 | 0.89 |
| 5th minute | 57.96 ± 6.82 | 53.43 ± 6.19 | 0.51 |
| 20th minute | 50.46 ± 6.29 | 50.60 ± 6.70 | 0.93 |
| Mean heart rate (bpm) | |||
| 1st minute | 133.50 ± 13.47 | 125.70 ± 14.80 | 0.03 |
| 5th minute | 126.20 ± 16.36 | 117.63 ± 18.02 | 0.05 |
| 20th minute | 122.63 ± 15.81 | 116.23 ± 17.81 | 0.14 |
Hemodynamic Changes in the First, Fifth, and 20th Minutes After Anesthesia in Two Groups
Table 4 shows the frequency changes in sinus arrhythmia in the two groups. As shown, there was a significant difference between the two groups in the first minute (P = 0.001), but no significant differences were observed in the fifth and 20th minutes.
| Time (Minute) | Intervention Group | Control Group | P Value |
|---|---|---|---|
| 1st | 12 (40) | 0 (0) | 0.001 |
| 5th | 1 (3.3) | 1 (3.3) | 0.75 |
| 20th | 0 (0) | 0 (0) | 0.001 |
Frequency Distribution of Arrhythmias in the First, Fifth, and 20th Minutes in Two Groups a
5. Discussion
This study aimed to determine the cardiovascular effects of epinephrine addition to local anesthetic drugs in children under caudal epidural block for sub-umbilical surgery. Various studies have been conducted on different techniques of caudal epidural block and its effect on postoperative analgesia in children. This technique represents the most popular pediatric regional anesthetic in surgeries such as lower abdominal, urological, and lower extremities. Caudal epidural anesthesia is a simple and safe method for sub-umbilical surgeries shorter than 90 minutes in children (10). Block failure is observed in 3 - 5% of patients and is commonly reported in children over seven years old (11). In a study conducted on 750 cases of the caudal block, a block failure rate of 1% was reported in children under seven years old and 14.5% in older children (12). In most cases, lidocaine 1% or bupivacaine 0.25% are used. Bupivacaine has a longer half-life than lidocaine. The usual dose of bupivacaine is 2 mg/kg. Its effects start 15 - 30 minutes after administration and last 2.5 - 4 hours (11). In this study, bupivacaine 0.2% at 2 mg/kg dose was used. Epinephrine (1/200000) was added to the local anesthetic to improve the quality and duration of analgesia in the caudal epidural block.
The most common complication of the caudal block with local anesthetics is motor block and systemic toxicity of drugs. To solve this problem, it has been suggested that local anesthetics should be combined with other medications such as epinephrine, clonidine, midazolam, neostigmine, and various opioids (13). Opioids can also be used with local anesthetics to increase the duration of the block, with fentanyl being the most commonly used (14).
There was no significant difference between the two groups in mean systolic, diastolic, and arterial BP in the first, fifth, and 20th minutes after anesthesia. However, there was a significant difference in heart rate in the first minute after anesthesia, but no significant difference between the groups was detected in the fifth and 20th minutes after anesthesia. In a study by de Beer and Thomas, epidural clonidine was associated with bradycardia, decreased blood pressure, and prolonged analgesia, occurring within 15 - 30 minutes and lasting up to three hours (10). In another study, adding clonidine 1 - 5 µg/kg to the local anesthetic made no significant hemodynamic changes (15). In a study, a caudal block before surgery could reduce hemodynamic changes during surgery, which might also be due to the analgesic effects of the caudal block before surgery (16).
Our study showed that hemodynamic changes such as hypertension and tachycardia did not differ significantly between the two groups before epinephrine injection. Also, there was no significant difference in heart rate in the fifth and 20th minutes after caudal block between the two groups, but in the early minutes, there was a significant difference in heart rate between them, so in the early minutes, the heart rate was more in children receiving epinephrine than in the control group. The difference might be due to the incidence of sinus tachycardia in the study group in contrast to the control group because there was no significant difference in the incidence of sinus tachycardia between the two groups in the fifth and 20th minutes.
August et al. showed no significant difference in heart rate and mean arterial blood pressure between the two study groups (17), which is consistent with the results of our study. August et al. concluded that epidural epinephrine at low doses increases cardiac index (CI) and stroke volume (SV) and reduces peripheral vessels resistance (17), which is not comparable with our results due to the lack of CI and SV measurement in our study; we recommend to do so in future research.
In a study by Liu et al., 23 children were studied as the epinephrine-receiving group with local anesthetic and 17 children as the only local anesthetic group. No changes in heart rate and blood pressure in epinephrine recipients were observed compared to the control group within 15 minutes after injection. They did not observe any significant difference in the cardiac index and stroke volume between the epinephrine-receiving group and the control group, which is consistent with our study results in changes in heart rate and blood pressure. However, in children aged six months or more, the cardiac index and stroke volume significantly increased in the epinephrine-receiving group compared to the control group (2).
Our study showed no significant difference in systolic, diastolic, and mean arterial blood pressure between the two groups. However, in our study, children receiving epinephrine compared to the control group did not suffer from increased systolic or diastolic blood pressure. Liu et al. showed no significant changes in blood pressure in children receiving epinephrine with local anesthetics over 15 minutes after injection compared to the injection time (2). This finding is consistent with our study results.
Liu et al. observed no changes in the heart rate of infants less than six months old receiving epinephrine compared to the control group, while it increased in children aged six months or older (2). This finding is consistent with our study showing an increase in the first-minute heart rate among children in the study group compared to the control group. In a survey conducted by Abukawa et al. on rats, the administration of epinephrine into the epidural space was safe in young rats (18), which is consistent with the results of our study. Our findings are compatible with the results of Deng et al., showing the stability of hemodynamic variables during caudal anesthesia with bupivacaine and epinephrine-added bupivacaine in newborns (19).
5.1. Conclusions
According to our study results, epinephrine added to local anesthetic drugs makes no permanent changes and just increases the prevalence of sinus tachycardia, and this arrhythmia was not permanent; therefore, epinephrine as an additive to local anesthetic drugs is safe to use in children undergoing caudal blocks. Considering the few studies in this field and different results in this regard, it is recommended that this study should be conducted with more sample size and in a longer period by examining influential factors such as block level, injection site, age and sex of patients to make a better decision on the effects of epinephrine as an additive, along with local anesthetic drugs in children undergoing caudal blocks.