1. Background
Shoulder pain is one of the most common musculoskeletal complaints that people need treatment for (1). The shoulder is one of the most common pain sites, ranking third among musculoskeletal pains in the general population. Shoulder pain usually leads to decreased active and passive range of motion. Depending on this decrease, activities performed at work or home may be negatively affected, leading to functional limitations (2). Limitation in the shoulder range of motion is usually caused by various shoulder pathologies and manifests at more than one site.
The stability provided by the trunk is needed for normal shoulder function. This is also related to balance. The shoulder joint complex should increase movement speed and/or strength to compensate for decreased core stability and/or impaired coordination of the lower extremity, trunk, or scapula (3). It is still unclear whether balance problems contribute to or are a consequence of shoulder pathology in patients with shoulder pathologies (4). Myers et al. observed that another factor that may cause limitations in the shoulder's functionality is somatosensory deficits in the trunk or lower extremities (5).
Any disorder in perceiving pain might cause balance problems (6). These balance problems can be observed due to muscle inhibition during pain perception and because the structures involved in balance control have common pathways (7). Presynaptic inhibition of muscle afferents may develop due to pain (8). Pain in the muscles around the temporomandibular joint can affect central modulation by causing changes in the proprioceptive mechanism (9). Neuronal speed and muscle inhibition may be negatively impacted by pain, impairing balance. Luoto et al. reported that the information processing speed of central neural mechanisms decreased in individuals with lumbar pain (10). It is unclear, though, if pain contributes to balance impairments, given how it affects the proprioceptive, muscular, and central nervous systems.
One of the crucial muscles involved in the lateral flexion movement of the trunk is the latissumus dorsi muscle. According to myofascial connections, this muscle transmits the force from the gluteus maximus muscle to the upper extremities (11). Serratus anterior muscle activation can be enhanced by the myofascial connections of the gluteal muscles and the lateral flexors of the trunk (12). Therefore, it was revealed that deterioration in the performance of trunk muscles might contribute to the development of pain and shoulder injury by affecting the activation of the serratus anterior (13).
One of the conditions that cause upper extremity malalignment is the disruption of the force transmission chain that develops due to decreased core endurance. It is necessary to use effective treatment interventions by controlling the pain level to increase the shoulder range of motion and function in patients with shoulder pain. There are various treatment methods for shoulder pain and no standardization (14). Despite the clinical guidelines developed to guide practices, there is still no optimal treatment for shoulder pain (15). Conservative shoulder treatment includes traditional rehabilitation therapy such as range of motion and stretching exercises, therapeutic modalities, manual therapy, and exercise prescription (16, 17).
2. Objectives
Our study evaluates the postural stability and balance status of individuals with shoulder pain and investigates the effects of conventional treatment for shoulder pain on postural instability and balance parameters.
3. Methods
Twenty patients who applied to the Physiotherapy and Rehabilitation Clinic of our university with the complaint of shoulder pain and 20 healthy individuals were included in the study. The criteria for inclusion in the treatment group were: Having been suffering from shoulder pain for at least 3 months, and the participants in both groups had to be between the ages of 19 and 60. The exclusion criteria were: Having undergone a surgical operation in the last 6 months and having cognitive problems that would prevent exercise participation. The individuals included in the study were assigned to two groups: The treatment group and the control group. After initial measurements and evaluations, a 24-session physiotherapy program was applied to those in the treatment group. The conventional physiotherapy program the patients in the treatment group followed included 20 minutes of hot-pack application, 20 minutes of conventional TENS (COMPEX Rehab 400), and ultrasound (Chattanooga Intelect Ultrasound) of the shoulder joint with a 1 MHz frequency and 1.5 W/cm2 intensity for 5 minutes. The treatment program was applied 3 times a week. The exercise program was designed to last approximately 40 minutes. An exercise program was applied, including active assistive and active range of motion exercises, stretching exercises aimed at the shoulder muscles at the pain limit, and posture exercises. Following the decreased pain intensity, strengthening exercises aimed at the rotator cuff and scapular muscles were implemented. At the end of the treatment program, the participants were reevaluated, and the effects of the conventional physiotherapy program on individuals with shoulder pain were examined. The sample size of the study was calculated based on the range of motion value in the study conducted by Salamh PA et al. (18). Using the G Power software (version 3.1.9.7), the effect size was calculated with a power of 95% and a type 1 error of 0.05, resulting in 20 participants for each group, and a total of 40 participants.
Consent was obtained from the individuals included in the study, and information was given about the study. The Numerical Rating Scale (NRS) assessed individuals' pain. On a line drawn from 0 to 10 on the NRS, participants are asked to mark the appropriate range for pain intensity (19). A universal goniometer was used to evaluate the active range of motion. The biodex balance system (BBS) evaluated postural stability and balance. Biodex balance system has been in use as an assessment tool in a range of different populations (20).
The postural stability of the participants was tested on the dynamic platform in BBS. The fall risk assessment was performed on the dynamic platform, with its mobility progressively increasing from level 12 to level 6, with eyes open and closed. During the test, the participants were asked to look at a fixed point at eye level. The test was performed 3 times, and the average value was calculated. A 15-second rest period was given between each repetition.
3.1. Statistical Analysis
The statistical program statistical package for social sciences (SPSS) SPSS 21.0 was used to analyze the obtained data. The tables present the arithmetic means as mean ± SD (standard deviation) numerical values in the study. The normal distribution tests were performed with the Shapiro-Wilk test. Intra-homogeneity tests were performed with an independent sample t-test for continuous variables and a chi-square test for discontinuous variables. Pearson correlation analysis was performed to find the correlation of the data. P < 0.05 was considered statistically significant in all analyses.
4. Results
No statistically significant difference was found between the ages, body mass indices, and genders in both groups in our study (P > 0.05) (Table 1).
| Treatment Group | Control Group | P | |
|---|---|---|---|
| Age | 42.20 ± 10.82 | 33.20 ± 7.75 | 0.005 |
| BMI | 26.14 ± 4.56 | 26.00 ± 4.37 | 0.921 |
| Gender | 9 female, 11 male | 10 female, 10 male | 0.752 |
| Dominant side | 18 right, 2 left | 15 right, 5 left | 0.00 |
| Affected side | 10 right, 10 left | - | - |
| Diagnosis | 10 RCS, 5 frozen shoulder, 3 impingement, 2 tendinitis |
Abbreviations: BMI, body mass index; RCS, rotator cuff syndrome.
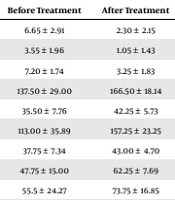
When the pre-treatment values of the treatment group were examined, differences were found in all values. However, a statistically significant difference was found in the pain and joint range of motion scores (P = 0.00; P = 0.02) (Table 2).
| Before Treatment | After Treatment | P | |
|---|---|---|---|
| NRS activity | 6.65 ± 2.91 | 2.30 ± 2.15 | 0.000 |
| NRS rest | 3.55 ± 1.96 | 1.05 ± 1.43 | 0.000 |
| NRS night | 7.20 ± 1.74 | 3.25 ± 1.83 | 0.000 |
| Flexion | 137.50 ± 29.00 | 166.50 ± 18.14 | 0.000 |
| Extension | 35.50 ± 7.76 | 42.25 ± 5.73 | 0.000 |
| Abduction | 113.00 ± 35.89 | 157.25 ± 23.25 | 0.000 |
| Adduction | 37.75 ± 7.34 | 43.00 ± 4.70 | 0.020 |
| Internal rotation | 47.75 ± 15.00 | 62.25 ± 7.69 | 0.000 |
| External rotation | 55.5 ± 24.27 | 73.75 ± 16.85 | 0.000 |
| Dynamic overall | 1.16 ± 0.60 | 0.92 ± 0.43 | 0.223 |
| Dynamic AP index | 0.81 ± 0.54 | 0.67 ± 0.38 | 0.377 |
| Dynamic ML | 0.64 ± 0.34 | 0.60 ± 0.38 | 0.645 |
Abbreviations: NRS, Numerical Rating Scale; AP, anterior-posterior; ML, medial-lateral.
When the results of the post-treatment balanced assessment of the two groups were analyzed, statistically significant differences were observed in all scores except for the dynamic balance of the medial-lateral balance (P = 0.014; P = 0.016) (Table 3).
| Treatment Group | Control Group | P | |
|---|---|---|---|
| Dynamic overall | 0.93 ± 0.43 | 1.49 ± 0.88 | 0.014 |
| Dynamic AP index | 0.67 ± 0.38 | 1.01 ± 0.49 | 0.016 |
| Dynamic ML | 0.59 ± 0.38 | 0.87 ± 0.80 | 0.176 |
Abbreviations: AP, anterior-posterior; ML, medial-lateral.
In addition, correlation analysis was performed between the parameters we evaluated. However, no significant correlation was found between the evaluation parameters (pain; balance r < 0.2).
5. Discussion
Comparing individuals with shoulder pain and healthy individuals, our study investigated their postural stability and balance. No study has examined conventional therapy's effects on postural stability and balance in individuals with shoulder pain. We observed statistically significant improvements in activity, rest, night pain, and all aspects of shoulder joint range of motion values of the individuals with shoulder pain to whom we applied conventional treatment. However, improvements were observed due to the BBS assessment, but no statistically significant results were found. As a result of the dynamic balance assessment between the groups, a statistically significant difference was found between the individuals with shoulder pain and healthy individuals.
Daily activities of individuals with shoulder pain may be adversely affected (21). Evidence suggests that conservative approaches are not only as effective as surgical treatments but are also associated with fewer risk factors (22). Exercise applications are one of the prominent methods among conservative approaches. However, there is insufficient evidence in the literature regarding the positive effects of exercise on shoulder pain (23). Successful rehabilitation of musculoskeletal pain requires a combination of multiple treatments rather than a single treatment method. Conservative therapy, which includes electrotherapy and exercise therapy, can effectively reduce pain associated with musculoskeletal pain (24). For this reason, we aimed to create a more effective treatment program by implementing electrotherapy methods, heat agents, and exercise applications.
Igrek and Colak divided patients with shoulder pathology into 3 groups and investigated the effects of different combined treatment methods on pain, range of motion, function, and muscle strength (25). It has been reported that applications in addition to conventional treatment effectively achieve better results. In addition to conventional treatment in our study, we applied a joint range of motion, stretching, strengthening, and posture exercises in combination.
Daghiani et al. found that comprehensive physiotherapy applications positively affect pain, disability, and quality of life (26). Comparing different physical therapy methods in patients with shoulder pain, Gunay Ucurum et al. investigated the effectiveness of hot packs, exercise, and TENS applications (27). It was observed that ultrasound and TENS applications applied in addition to exercise therapies have positive effects on pain, function, and quality of life, but they do not have superiority. We also implemented a combined treatment method in our study and achieved similar results.
The effects of TENS and soft tissue massage on individuals with shoulder pain were studied by Badaru (28). Badaru showed that both methods positively affect pain control, but the TENS application yields better results (28). Similarly, we recorded positive improvements in pain control through conventional TENS application in our study.
Examining the effectiveness of ultrasound application in patients with shoulder pathology, a review study found that ultrasound applications combined with other physical modalities effectively reduce general pain (29). We observed improvements in pain control by applying ultrasound therapy in addition to exercises and TENS.
Exercise therapy should be one of the first options that come to mind for pain control and better mobility in individuals with subacromial shoulder pain. However, more studies are needed on exercise therapy's type, frequency, and duration (30).
Exercise was reported to be an effective treatment strategy for various chronic musculoskeletal problems to reduce pain and increase function in patients' daily activities (31). The good function of the shoulder mostly depends on trunk stability. Therefore, it is closely related to balance control.
Eker and Belgen Kaygisiz examined balance and postural stability in patients with shoulder pathology. They concluded that balance and postural stability are related to shoulder pain (32). Park et al. investigated the effects of stabilization exercises performed in different shoulder joint ranges of motion on static and dynamic balance in healthy adults. There was no difference in balance between the exercises performed at different shoulder angles (33).
Baierle et al. compared healthy adults and those with shoulder problems regarding balance and postural stability. There was no relationship between pain intensity and balance but decreased balance and postural stability in individuals with shoulder problems (3). Similarly, there was no correlation between the scores of pain and balance, but a decline in balance skills in individuals with shoulder pain.
In another study involving individuals with shoulder pain and healthy individuals, balance and walking performance were evaluated. Romberg test, timed unipedal stance test, and timed up-and-go tests were used as evaluation methods. No statistically significant difference was found between the groups in the study. We believe using field balance assessment methods instead of an objective assessment method called BBS might have led to this result (34).
Dynamic balance was evaluated through the Star Excursion Balance test and Y Balance test in a cross-sectional study examining baseball pitchers with and without shoulder pain. Loss of balance was observed in those with shoulder pain in the study. More loss of balance was observed in the posterolateral direction (35). Loss of balance was higher, mainly in the posterolateral direction in our study. A statistically significant difference was found in the results of the dynamic balance assessment between the groups.
Yorukoglu et al. examined the core stabilization of healthy adults and those with rotator cuff syndrome. All participants were of similar ages. Core stabilization and neuromuscular control were negatively affected in those with rotator cuff syndrome (36). Although there was no statistically significant difference between the individuals with shoulder pain and healthy individuals, the postural stabilization skills of the former were found to be lower.
Kim et al. investigated the effects of shoulder stabilization exercises and stretching exercises aimed at the pectoralis muscle on balance in healthy individuals with rounded shoulder postures (37).
The results showed that static and dynamic balance improved in both groups. Our study aimed to increase recovery by applying a program that included both stretching and stabilization exercises to the treatment group. The treatment program led to decreased pain levels, increased joint range of motion, and improved postural stability in the study (37). Alqarni et al. investigated the physiological and pathological causes of limited internal rotation of the glenohumeral joint. Compared to the group without shoulder pain, those with shoulder pain had a less internal rotation of the glenohumeral joint. The total range of motion values between the shoulder pain group and the group without shoulder pain were found to have a statistically significant difference. However, no significant relationship was found between the pain intensity and the joint's range of motion (38). Pain intensity in an activity, at rest, and night was assessed in our study. No significant relationship was found between pain levels and range of motion values.
In a review study investigating the effectiveness of physiotherapeutic applications in individuals with shoulder pathology, therapeutic exercises were reported to be effective in reducing pain and increasing the range of motion. It was found that electrotherapy applications play a role in short-term pain control but do not improve the joint's range of motion, and deep heat agents could be used to provide pain control and increase the range of motion of the joint (29). We observed improvements in the range of motion of the shoulder joint thanks to the exercise applications and the use of deep heat agents in our study.
5.1. Limitations
The sample of the study was forty. Studies with bigger sample sizes might give more accurate findings. In addition, we also included healthy people in one group. Considering the mentioned limitations, clinical studies should be done.
5.2. Conclusions
The postural stability and balance status of individuals with shoulder pain were evaluated, and no statistically significant difference was found between healthy individuals and those with shoulder pain. However, it was observed that conventional shoulder pain treatment positively affects postural instability and balance parameters. In conclusion, it was revealed that therapeutic agents applied in addition to exercise in individuals with shoulder pain are a safe method that can be used to improve the parameters of pain, mobility, balance, and postural stability.