1. Background
Pelvic fractures are one of the most severe injuries of the skeletal system, which are seen especially in the elderly and have high mortality and morbidity, requiring surgical intervention (1, 2). One of the most important side effects in this group of surgical procedures is pain accompanied by many unwanted side effects (3). Pain can result in unfavorable hemodynamic and metabolic responses (3, 4). Inadequate pain relief during and after surgery results in complications, such as a long recovery period, long hospitalization period, increased hospital costs, and decreased patient satisfaction (5). Nowadays, pain management is a part of the surgical process and not only reduces patients’ suffering but also the mortality rate. It also causes rapid recovery and early discharge from the hospital with low costs (6).
Regional anesthesia, such as femoral nerve block, can improve the anesthesia process and recovery time (7-9). However, the duration and extent of effectiveness and coverage of this block are not very high, and especially it does not include the obturator nerve (9-13). The anterior capsule of the hip is innervated by the obturator nerve (14). In general, the femoral nerve and the anterior obturator are considered the most important innervation systems in the pelvic region (15).
Recently, fascia iliaca compartment block (FICB) has been considered to reduce pain before and after hip surgery because this method is relatively fast. Due to the quick effect of this method, it can be used for the positioning of patients with hip fractures before surgery (16). Following the use of the above method in hip fracture surgery, the mean pain score decreases from 8.5 to 2.3 2 hours after the operation (17). Patients who were subjected to FICB during hip replacement surgery had a significantly lower need for morphine during the first 24 hours after surgery (18). Pericapsular nerve group (PENG) block is another block that can be used in pelvic surgeries (19), in which a case-series report revealed the excellent analgesia effects of this block (20). Today, much attention is paid to the well-being of patients in order to reduce pain during and after surgery, and many studies have been conducted in this field (21-24). Considering the importance of analgesia after hip fracture in patients who need to be in the right position to perform neuraxial anesthesia and there are limited and mostly case-series studies of the pericapsular block.
2. Objectives
In this study, a comparative analysis of analgesia was performed using PENG and FICB in the positioning of patients with hip fractures.
3. Methods
3.1. Design and Setting
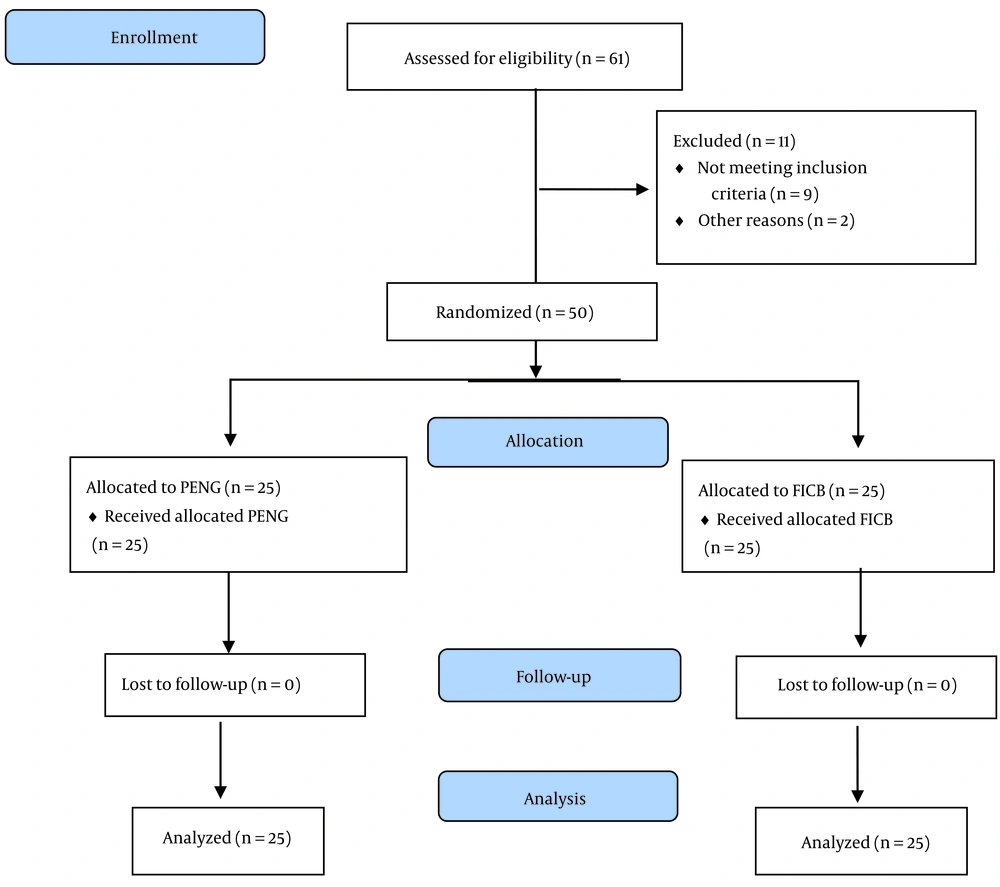
In this double-blind clinical trial study, 50 patients (each group as a pilot: 25 patients) who were candidates for femoral neck fracture surgery were referred to Imam Khomeini Hospital in Urmia. They were randomly assigned to 2 groups, including PENG and FICB. Due to the pilot nature of the study, it seems reasonable to recruit the minimum number of patients, and based on Hertzog’s study, the sample size in pilot studies is 25 people in each group (25). Random allocation software was used to allocate patients into 2 random groups. Visual Analogue Scale (VAS) score was used to assess analgesia (26). Allocation concealment was also observed in the process of conducting the study (Figure 1).
3.2. Eligibility Criteria
Inclusion criteria were age between 18 and 80 years, ASA class ≤ II, and absence of spinal deformity. Exclusion criteria were the presence of any anatomical anomaly in the spine, the presence of cardiovascular disease, sensitivity to local anesthetics, and coagulopathy disorders.
3.3. Intervention
In the pericapsular block, 20 mL of 0.25% bupivacaine is deeply injected between the muscle and the fascia, which is anterior to the psoas tendon and posterior to the ramus of the pubic bone, and the patient is in the supine position. In the fascia iliaca block, 20 mL of 0.25% bupivacaine is deeply injected into the iliac fascia and in the upper lateral part of the iliac muscle when the patient is in the supine position. The pain level of the patients was assessed before the block, 10 minutes after the block, and before positioning for neuraxial anesthesia using a VAS score.
3.4. Blinding
The patients were unaware of their allocation to the intervention groups, and the statistical analyzer was unaware of the assignment of the patients in the study groups and received the data as code A (for pericapsular block) and B (for fascia iliaca block). Therefore, the study was double-blind. The data were analyzed using SPSS version 16 software. The descriptive data were presented as frequency, mean and standard deviation (SD). The chi-square test was used to measure qualitative variables in the 2 groups, and independent t-test was used for quantitative variables. P-value < 0.05 was considered statistically significant.
3.5. Ethical Issue
After the approval of the Ethics Committee of the Urmia University of Medical Sciences (IR.UMSU.REC.1400.160) and registration in the clinical trial registry center (IRCT20170516033992N8), informed consent was obtained from all the patients to participate in the study.
4. Results
Regarding gender, 38% (N = 19) were female, and 62% (N = 31) were male. The mean age was 57.38 ± 8.49 years (range: 43 to 80 years), and no significant difference was observed between the 2 groups (P = 0.315). The mean body mass index (BMI) was 26.44 ± 3.77 kg/m2 (range: 19.53 to 34.7 kg/m2) and no significant difference was observed between the 2 groups (P = 0.123). The mean pain was not significant in both groups before the intervention, but 10 minutes after the block, the pain score was 1.72 ± 0.73 in the pericapsular group and 3.92 ± 0.86 in the fascia iliaca group, and a significant difference was observed between the 2 groups (P < 0.001). The mean pain difference was significant in the pericapsular and fascia iliaca groups before and after the block, so the pericapsular group showed a greater reduction in pain (P < 0.001) (Table 1).
| Variables | Mean ± SD | t | P-Value |
|---|---|---|---|
| Age | 1.016 | 0.315 | |
| Pericapsular block | 58.60 ± 10.20 | ||
| Fascia iliaca block | 56.16 ± 6.33 | ||
| BMI | -1.183 | 0.243 | |
| Pericapsular block | 25.81 ± 3.16 | ||
| Fascia iliaca block | 27.07 ± 4.26 | ||
| Pain score 10 minutes after block | -9.697 | < 0.001 | |
| Pericapsular block | 1.72 ± 0.73 | ||
| Fascia iliaca block | 3.92 ± 0.86 | ||
| Pain score difference before and after block | -6.983 | < 0.001 | |
| Pericapsular block | -8.32 ± 0.62 | ||
| Fascia iliaca block | -7.00 ± 0.70 |
Abbreviations: BMI, body mass index; SD, standard deviation.
The intensity of pain was homogeneous in the pericapsular and the fascia iliaca groups before the block. The pain was often classified as severe, and no significant difference was observed between the 2 groups (P < 0.999). Also, the intensity of pain was different in the pericapsular and the fascia iliaca groups 10 minutes after the block, and there was no pain in the moderate classification in the pericapsular treatment group, while 16 patients (64%) in the fascia iliaca group had moderate pain (P < 0.001) (Table 2).
a Pain score 4 - 7.
b Pain score 8 - 10.
c Pain score 0 - 3.
5. Discussion
This clinical trial study aimed to compare the analgesic effect of pericapsular nerve block and iliac fascia with ultrasound in positioning patients with hip fractures for neuraxial anesthesia as a pilot study. Patients with hip fractures, due to the location of the fracture, have a very low level of cooperation in the implementation of spinal anesthesia, which is due to the excruciating pain of the fracture and movement during the anesthetic procedure, so it is possible to provide acceptable analgesia with methods such as pericapsular block. The patient should cooperate to continue the process of spinal anesthesia, such as epidural. Due to randomization, the study groups had a homogeneous mean age, BMI, and gender frequency in both groups, making it comparable.
The mean pain in the pericapsular group was about 2 units less than the fascia iliaca group 10 minutes after the block, and a significant difference was observed between the 2 groups. The intensity of pain before the block was homogeneous in the pericapsular group and in the fascia iliaca, and the pain was often classified as severe. The intensity of pain was different in the 2 groups 10 minutes after the block, and there was no pain in the moderate classification in the pericapsular treatment group, while 64% of the patients in the fascia iliaca group had moderate pain with a statistically significant difference.
It should be noted that the mean pain score in the pericapsular group was insignificantly higher than in the fascia iliaca group before the block, but despite this, more pain reduction was seen in this group, which shows that the pericapsular method is more effective. Therefore, this study shows that the pericapsular block may provide better analgesia for positioning in comparison to the fascia iliaca block in patients with hip fractures. The intensity of pain was homogeneous in the pericapsular group and in the fascia iliaca before the block, the pain was often classified as severe, and no significant difference was observed between the 2 groups (P < 0.999).
Also, the intensity of pain was different in the pericapsular and fascia iliaca groups 10 minutes after the block, and there was no pain in the moderate classification in the pericapsular treatment group, while 16 patients (64%) in the fascia iliaca group had moderate pain. It should be noted that the pericapsular block showed better results than the fascia iliaca block method, and this does not mean that the fascia iliaca block method is ineffective, and fact, the fascia iliaca block is superior to some other blocks, e.g., in a study by Yu et al. (27), they indicated that the mean score of analgesia in the femoral block group was 1, and in the iliac fascia group was 0.5.
Femoral block analgesia was better in the medial part of the thigh, and the fascia iliaca block showed better analgesia conditions in the lateral part of the thigh. Both methods of anesthesia were suitable for hip reduction surgery (27). One of the important and fundamental limitations of this study is the low sample size, which makes it difficult to decide on a rough clinical finding.
5.1. Conclusions
This study showed that pericapsular block may provide better analgesia for positioning in comparison to fascia iliaca block for patients with hip fractures. However, it is recommended to conduct further investigations with a larger sample size to generalize the results of this pilot study.