1. Introduction
In December 2019, a highly contagious disease broke out in Wuhan, China, which is named as the coronavirus disease 2019 (COVID-19) by the World Health Organization (1). There is currently no specific drug for this disease and it can only be treated symptomatically. Hypoxemia is a common clinical manifestation of severe patients. Treatment for hypoxemia is mainly oxygen therapy, including nasal catheters, masks, noninvasive and invasive mechanical ventilation, and extracorporeal membrane oxygenation (2). This article reports for the first time the computed tomography (CT) imaging dynamic changes in a 69-year-old male with severe type of COVID-19 treated by hyperbaric oxygen.
2. Case Presentation
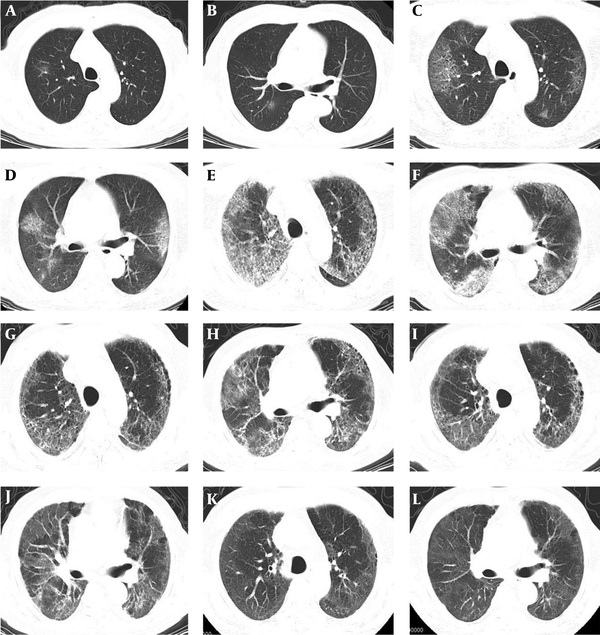
A 69-year-old male patient lived in Wuhan, Hubei Province, China for a long time and had a history of coronary atherosclerotic heart disease. The patient underwent coronary stent implantation in 2016 due to acute myocardial infarction. On January 22, 2020, the patient had chills and fever without any obvious cause, with a body temperature of 37.8°C, and he went to hospital for treatment. Emergency chest CT examination revealed multiple patchy ground-glass opacity (GGO) shadows in the S I and S II segments of the upper lobe of the right lung and the S I + II segment of the upper lobe of the left lung (Figure 1A and B). Pharyngeal swab real-time PCR detection was positive for nucleic acid of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The patient was hospitalized after confirmation of COVID-19 diagnosis. Physical examination at admission revealed the following findings: blood pressure 120/65 mmHg, body temperature 38.0°C, breathing 18 breaths/min, and pulse 80 beats/min. Laboratory examination revealed the following findings: white blood cell count 3.68 × 109/L (normal range: 3.5 - 9.5 × 109/L), lymphocyte count 1.47 × 109/L (normal range: 1.1 - 3.2 × 109/L), C-reactive protein 22.4 mg/L (normal range: 0 to 5 mg/L), D-dimer 0.28 mg/L (normal range: 0 to 0.55 mg/L), prothrombin time 11.3 s (normal range: 9 - 13 s), and partial thromboplastin activation time 28.2 s (normal range: 20 - 40 s).
Chest CT images of a 69-year-old man with severe COVID-19 treated by hyperbaric oxygen. A and B, First CT on the day of disease onset shows a patchy ground-glass opacity (GGO) shadow in S I and S II segments of the upper lobe of the right lung; C and D, Five days after the onset, re-examination of CT shows large patches of GGO shadows in S I, S II and S III segments of the upper lobe of the right lung and S I + II segments of the upper lobe of the left lung; E and F, Sixteen days after the onset, re-examination of CT shows diffuse lesions in both lungs, extensive exudation and consolidation of the lung parenchyma, and the crazy-paving sign; G and H, Twenty-seven days after the onset and 8 days after the hyperbaric oxygen treatment, re-examination of CT shows that the range of consolidation in both lungs has decreased, the lung interlobular septum has thickened, and fibrous cord shadows appear in the lower right lung; I and J, Thirty-eight days after the onset and 19 days after the hyperbaric oxygen treatment, re-examination of CT shows that the consolidation density in both lungs has reduced, but the range has not changed; K and L, Sixty-five days after the onset, follow-up CT examination shows diffuse GGO shadows in both lungs and the consolidation shadows and fibrous cord shadows have completely resolved.
After admission, the patient was given ceftriaxone sodium 3 g/d and abidor 0.2 g, three times/d, and continuous nasal cannula low-flow oxygen therapy. The body temperature of the patient returned to normal on January 25, 2020. On January 27, 2020, the patient developed panting after activity. Re-examination of CT showed that the range of GGO shadows in the S I, S II and S III segments of the upper lobe of the right lung and the S I + II segment of the upper lobe of the left lung was increased, and at the same time, new GGO shadows appeared in the S IV segment of the right middle lobe and the S X segment of bilateral lower lobes (Figure 1C and D). The patient was given high-flow mask oxygen. On February 7, 2020, the patient developed fever again, with a body temperature of 38.2°C. Re-examination of CT revealed diffuse lung lesions, extensive exudation, and consolidation of lung parenchyma, accompanied by the crazy-paving sign, the air bronchogram sign, and blood vessel thickening (Figure 1E and F). Blood gas examination showed arterial blood oxygen partial pressure (PO2) of 37 mmHg, arterial blood carbon dioxide partial pressure (PCO2) of 30.4 mmHg, and minimum finger-tip oxygen saturation (SO2) of 66%, which reached 88% after high flow oxygen inhalation. After obtaining informed consent from the patient and approval from the hospital ethics committee, the patient was given hyperbaric oxygen therapy on February 11, 2020 due to dyspnea and continuously exaggerated hypoxemia, with a total daily oxygen inhalation time of 95 minutes and an oxygen dose of 216 unit of pulmonary toxic dose (UPTD). On the morning of February 18, 2020, the patient received the last hyperbaric oxygen treatment. In the afternoon, blood gas examination showed a PO2 of 122 mmHg, PCO2 of 37.3 mmHg, and SO2 reaching 99%. The patient complained of significantly mitigated dyspnea and chest pain. Re-examination of CT showed that the area of consolidation in bilateral lungs decreased, the interlobular septum was thickened, and fibrous cord shadows appeared in bilateral lower lungs (Figure 1G and H). On February 19, 2020, the patient was switched to a nasal catheter for oxygen inhalation and was provided with the corresponding supportive treatment. Before discharge, two consecutive SARS-CoV-2 nucleic acid tests were negative, and reexamination of CT on February 29, 2020 showed that the density of bilateral lung consolidation lesions decreased, but the range did not change (Figure 1I and J). One month after discharge (March 27, 2020), follow-up CT examination showed diffuse GGO shadows in both lungs, while the consolidation shadows and fibrous cord shadows completely resolved (Figure 1K and L).
3. Discussion
CT is of guidance significance in the diagnosis of COVID-19 and the evaluation of the treatment efficacy. Based on the CT imaging evolution characteristics of the disease, it is divided into early stage, progressive stage, severe stage, and recovery stage (3). In the early stage, most patients show patchy and small sheet GGO shadows or simple ground-glass nodules in the peripheral zone of one lung or both lungs (4). In the progressive stage, the range of lesions increases, the proportion of consolidation increases, and interlobular septal thickening, crazy-paving sign, reversed halo sign, and blood vessel thickening may appear (5). In the severe stage, the area of the lesions is further expanded, with evident exudation, and the “white lung” manifestation may occur in patients with large-area involvement. In the recovery stage, the lesions may be partially absorbed, which is manifested by reduction in the lesion range and density, showing a ground-glass change. Over time, the lesions will gradually dissipate, and some of them may leave residual fibrous foci. In this report, the patient showed small patchy GGO shadows at three lung segments in the early stage. Sixteen days after disease onset, the lesions further expanded, the CT showed the “white lung” manifestation, and the patient’s hypoxia symptoms significantly aggravated. After eight sessions of hyperbaric oxygen treatment, CT showed that the density of the lung lesions was reduced, and fibrous cord shadows occurred. Although the lung lesions only partially resolved after hyperbaric oxygen treatment, SO2 was maintained within the normal range under the condition of nasal catheter oxygen inhalation, which suggests that hyperbaric oxygen therapy may directly interrupt the continuous accumulation of oxygen debt under the hypoxic state of tissues and organs in the entire body and the subsequent damage to important oxygen-consuming tissues and organs, providing a good systemic functional basis for the body to fight viral infections.