1. Introduction
Since the 1980’s, extracorporeal shock wave lithotripsy (ESWL) has become the most common treatment for urinary lithiasis (1). ESWL, as a noninvasive method, has rapidly become the most widely used treatment for the management of renal and ureteral stones because of its ease of use, besides the high efficacy and availability of lithotripters. Although ESWL is a safe tool to treat stones, a localized iatrogenic injury can allow bacteria in urine to enter the bloodstream and potentially cause complications. The predisposing factors for infectious complications following ESWL include preexisting urinary tract infections, infected kidney stones, multiple stones, staghorn stones, history of recurrent urinary tract infection, urinary obstruction, and instrumentation used during ESWL (2).
Here, we present the computed tomographic (CT) findings of a patient with necrotizing fasciitis along with abscess formation following ESWL, which rapidly invaded the neck, chest, and abdominal wall. To the best of our knowledge, this is the first case of necrotizing fasciitis with abscess formation after ESWL.
2. Case Presentation
A 67-year-old woman presented with persistent cough, intermittent nausea, and progressive right flank pain for one month after ESWL. Without anesthesia, she underwent ESWL with 3000 shock waves (13 - 16 kV for each wave), using a Ziel Zeus Extracorporeal Shock Wave Lithotripter (Ziel Medizintechnik GmbH, Germany) due to a right upper ureter stone, measuring 1.2 × 0.3 cm, with right hydronephrosis detected on abdominal X-ray and renal ultrasound. She reported no fever, chills, or dysuria, but had a history of Parkinson's disease, hypertension, and undiscovered type 2 diabetes mellitus (HbA1c 9.4%).
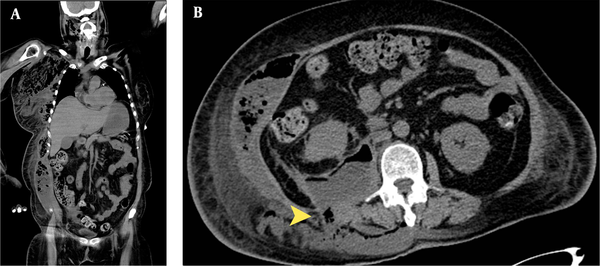
The initial abdominal CT scan showed perirenal and pararenal hematoma of the right kidney, and the serum level of hemoglobin decreased from 14.9 to 10.5 g/dL. After conservative treatment and antibiotic use for two weeks in a district hospital, her hemoglobin level decreased persistently to 8.3 g/dL, and she was transferred to our emergency department. On physical examination, knocking pain in the right flank was detected. The biochemical examination revealed a normal WBC count (9,000/uL) with bandemia (band count, 12%). A contrast abdominal CT scan in the emergency department showed perirenal and pararenal hematoma of the right kidney, extending to the right posterior pararenal space, right psoas muscle, and right paraspinal region (Figure 1). We prescribed empiric antibiotic treatment and antihemorrhagic agents and controlled her blood sugar.
A 67-year-old woman presented with persistent cough, intermittent nausea, and progressive right flank pain for one month after extracorporeal shock wave lithotripsy (ESWL). The CT scan of the abdomen indicates right perirenal and pararenal hematoma, measuring 12.8 × 9.4 cm along the right psoas muscle and the right paravertebral region after ESWL.
After one week of conservative treatment at our hospital, a follow-up CT scan showed necrotizing fasciitis, involving the muscle groups in the right lateral and posterior abdominal and thoracic walls, right axillary region, supra- and infra-clavicular regions, right breast, right arm, bilateral upper anterior chest wall, and right side of the neck (Figure 2). The abscess was immediately drained surgically through a retroperitoneal incision and three fasciotomies from the axillary fossa and the right abdominal wall. The hemorrhagic purulent material was drained, and a microbiological examination showed that Escherichia coli was the pathogenic agent. Four weeks after the surgical intervention which was performed three times, the inflammatory process almost resolved. After three months, the abscess almost completely resolved.
A, The follow-up CT scan from the neck to pelvis shows perirenal and pararenal hematoma of the right kidney with abscess formation, involving the right psoas muscle and the right paraspinal region after one week of conservative treatment. Necrotizing fasciitis involves groups of muscles in the right lateral and posterior abdominal wall, right axillary region, supra- and infra-clavicular regions, right breast, right arm, bilateral upper anterior chest wall, and right side of the neck. B, The perirenal and pararenal abscess spreads to the paraspinal region (yellow arrowhead) and invades the subcutaneous tissue. Necrotizing fasciitis occurs through upward and downward invasion to the adjacent structures.
3. Discussion
Minor complications have been reported following ESWL, including renal colic (40%), gross hematuria (32%), urinary obstruction (30.9%), and perirenal or subcapsular hematoma (4.6%). Symptomatic bacteriuria has been also reported in 9.7% of cases (3). Moreover, some rare major complications have been reported, such as abscess formation (4, 5), acute pancreatitis with abscess (6), and splenic rupture (7). However, to the best of our knowledge, this is the first case of necrotizing fasciitis with abscess formation after ESWL.
Cavitation is thought to be the most important force in ESWL. Nonetheless, tear and shear stress and cavitation activity generated by shock waves can cause damage to thin-walled vessels in the kidneys and adjacent tissues. The most common clinical presentations of renal trauma after cavitation include gross hematuria and hematoma (2). Treatment of ESWL-related hematoma is conservative in most cases, and it often spontaneously resolves within two years (8). Clinicians should closely monitor the patients’ blood pressure, renal function, and signs of infection or abscess formation. Our patient had perirenal and pararenal hematoma after ESWL, which rapidly progressed to abscess formation. The abscess invaded the posterior to paraspinal regions and then migrated upward to the chest wall, axillary, supra-clavicular, and infra-clavicular regions, arm, breast (Right side), and neck, with downward damage to the abdominal wall, causing necrotizing fasciitis.
Generally, necrotizing fasciitis is an uncommon and potentially fatal infection, which can involve the fascia and subcutaneous tissues (9). It is associated with a high mortality rate (20.5%), a long hospital stay, and multiple surgical interventions (10). The primary goal of the first surgical debridement is delineating the extent of infection and complete surgical excision of necrotizing soft tissue. Extensive surgical debridement may result in large raw wounds, and intensive post-excision wound care plays an important role in minimizing sepsis and hemorrhage (11). Overall, the development of necrotizing fasciitis after ESWL is rare. Abscess extension may occur rapidly and invade the adjacent structures. It is important to consider this fatal complication and perform a surgical intervention immediately.