1. Introduction
Clinically diagnosed renomedullary interstitial tumors are rare findings, as they are usually small and asymptomatic. Accordingly, reports on the imaging findings of these tumors are scarce, and it is difficult to distinguish benign renomedullary interstitial cell tumors from renal malignancies preoperatively based on imaging findings. Therefore, in most clinical situations, nephrectomy is ultimately performed for differential diagnosis (1).
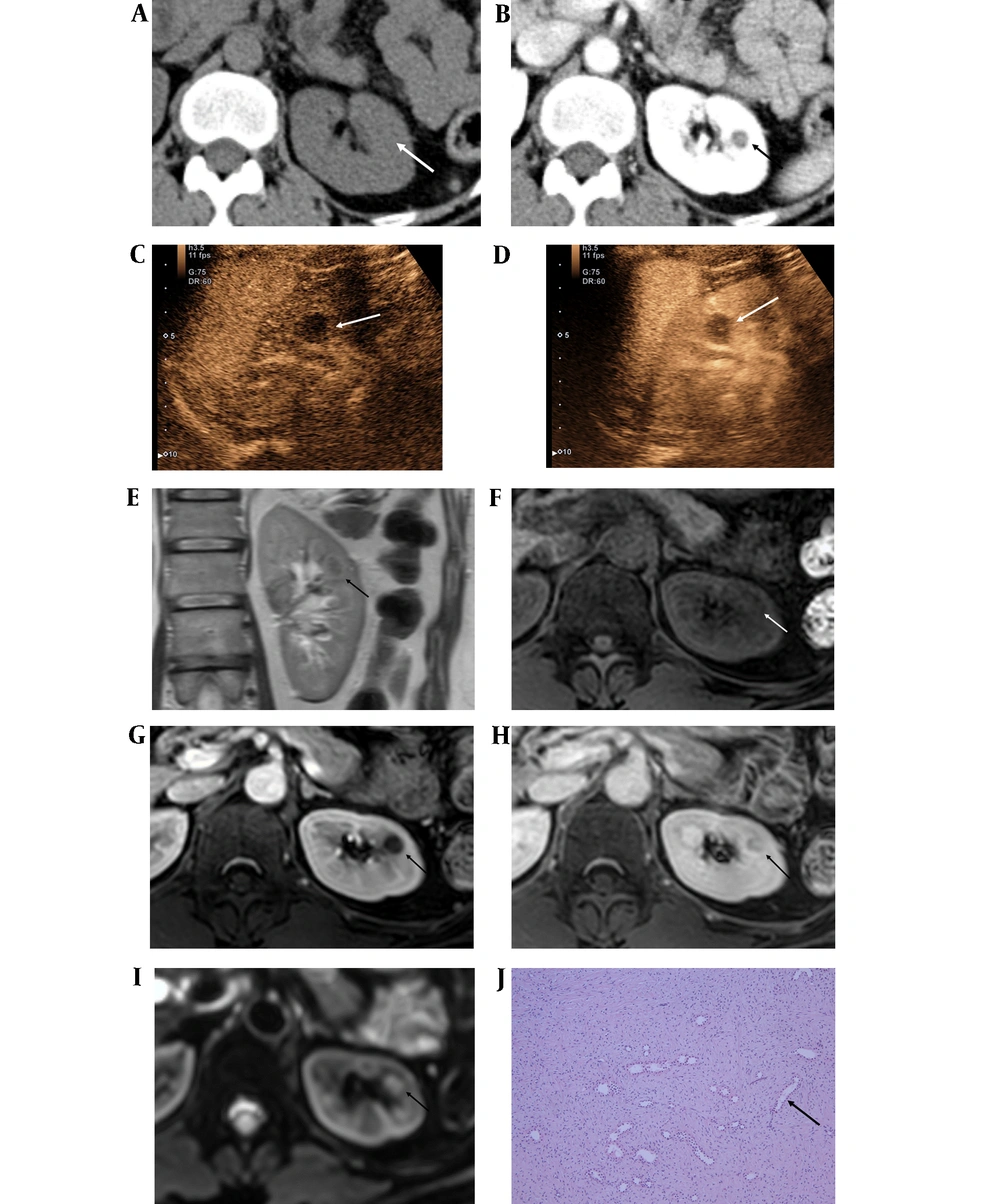
Herein, we report the imaging findings of a renomedullary interstitial cell tumor, which was incidentally detected in an imaging study and pathologically confirmed after surgical resection. The mass showed a low signal intensity on both T1- and T2-weighted images, and delayed enhancement was observed on dynamic magnetic resonance imaging (MRI) and contrast-enhanced ultrasonography (CEUS).
2. Case Presentation
A 54-year-old woman presented to our hospital with a complaint of hematuria. She had no medical history of any specific diseases. A peripheral blood test upon admission showed a slight increase in the white cell count (WBC, 11,000/uL), and a urine analysis showed hematuria and pyuria (RBC, 17552 µL/HPF; WBC, 3387 uL/HPF).
Contrast-enhanced abdominal computed tomography (CT) indicated bladder wall thickening and mucosal enhancement, which were correlated with the clinical symptoms and consistent with cystitis. Also, a well-defined mass, measuring approximately 1 cm, was found in the medullary portion of the mid-pole of the left kidney. The mass showed iso-attenuation to renal parenchyma in the pre-contrast image and hypo-attenuation in the portal venous phase; however, some enhancement was observed in the central portion of the mass (Figure 1A and B). No significant abdominal lymphadenopathy was observed. Therefore, the mass was initially regarded as a complicated cyst, such as a hemorrhagic cyst. The patient was discharged after completing treatment for cystitis.
After one year, CEUS with Sonovue® was performed on the left renal mass. It appeared as a hypoechoic and hypovascular mass in the arterial phase (30 seconds), and a slight septum-like enhancement was detected in the central portion of the mass in the venous phase (60 seconds) (Figure 1C and D). The patient underwent dynamic MRI for further evaluation of the renal mass. There was no change in the mass size. The mass was located in the medullary portion rather than in the cortex and was particularly well visualized and identified on coronal T2-weighted images.
A 54-year-old female with hematuria, diagnosed with a renal interstitial cell tumor. A, Pre-contrast axial CT scan shows a 1-cm mass with iso-attenuation (white arrow); B, Enhanced axial CT scan shows a well-defined mass with dot-like enhancement in the central portion of the mass (black arrow); C, A 1-cm hypoechoic and hypovascular mass in the left kidney in the arterial phase of contrast-enhanced ultrasonography (CEUS) with Sonovue® (white arrow); D, The mass shows septal enhancement in the central portion in the venous phase of CEUS (white arrow); E, On coronal T2-weighted image, the mass shows a low signal intensity in the medullary portion of the left kidney (black arrow); F, The mass shows a low signal intensity on axial T1-weighted MRI (white arrow); G, In the axial portal phase image, the mass shows suspicious enhancement in the central portion of the mass (black arrow); H, In the 10-min delayed image, the mass shows persistent enhancement (black arrow); I, The mass shows mild diffusion restriction on the diffusion-weighted imaging/apparent diffusion coefficient (DWI/ADC) image (black arrow); J, The histopathological examination shows stellate and spindle cells in a background of fibrous stroma with entrapped renal tubules (black arrow) (hematoxylin & eosin staining, 100X magnification).
On T1- and T2-weighted images, the mass showed a low signal intensity, and a delayed persistent enhancement was observed in the 10- and 15-minute delayed phases (Figure 1E - H). The lesion showed mild diffusion restriction (Figure 1I). Also, no signal drop was observed on the chemical shift image. Although there was no change in the size of the mass in the long-term follow-up, the mass showed enhancement in both ultrasound and MRI, and it was considered as a solid mass rather than the complicated cyst.
The patient underwent partial nephrectomy for the mass, because it was not possible to completely differentiate papillary renal cell carcinoma from other benign solid tumors based on the imaging findings. The surgical examination revealed an endophytic mass in the anterior aspect of the mid-pole of the kidney. A gray-white mass, approximately 1.2 cm in size, was observed in the excised tumor. According to the pathological findings, it was finally diagnosed as a renomedullary interstitial cell tumor. The microscopic examination also revealed small spindle or stellate cells in a background of loose fibrotic stroma with entrapped tubules (Figure 1J).
3. Discussion
Renomedullary interstitial cell tumors, also known as medullary fibromas, are rare benign renal mesenchymal tumors, arising from interstitial cells of the medulla. These tumors are usually asymptomatic, as they are commonly smaller than 5 mm in size (2). However, large tumors may have clinical symptoms, such as hematuria and abdominal pain (3, 4). According to gross pathology, renomedullary interstitial cell tumors are characterized by white or gray nodules in the renal pyramid, and in histological examinations, they are characterized by stellate spindle cells in the background of basophilic or fibrotic stroma (3, 4).
The preoperative diagnosis of renomedullary interstitial cell tumors is difficult, as most of these tumors are not clinically evident; consequently, there are only few studies on imaging reports. Additionally, these tumors often mimic malignancy. The imaging findings of renomedullary interstitial cell tumors may represent a small, less-enhancing, hypodense solid mass within the renal medulla on CT scans (5). Rarely, these tumors are larger or protruding polypoidal masses in the renal pelvis (6). In both T1-weighted and T2-weighted MRI, these tumors show a low signal intensity owing to their rich collagen content and low cellularity (7). In our case, the mass showed delayed enhancement in the 10- and 15-minute delayed phase of dynamic MRI, besides a low signal intensity on both T1- and T2-weighted images. The results of CEUS revealed a hypoechoic and hypovascular mass in the early phase, as well as a septum-like enhancement in the central portion of the mass in the delayed phase.
The differential diagnoses of renomedullary interstitial cell tumors are solid renal tumors, which may exhibit a low signal intensity on T2-weighted MRI, such as leiomyoma, angiomyolipoma (AML), and non-clear cell renal cell carcinoma (RCC). Renal leiomyoma is a rare benign tumor, arising from the smooth muscle cells of the kidney (3, 5). This tumor may be considered a differential diagnosis, as it shows a well-defined soft tissue density and represents as a homogeneous mass on CT scans, with a low signal intensity on both T1- and T2-weighted MRI (1).
Among malignancies, RCC can be considered a differential diagnosis for renomedullary interstitial cell tumors, especially papillary RCC (pRCC). Commonly, pRCC has a low signal intensity on both T1- and T2-weighted images, unlike clear cell RCC (cRCC), which shows a high signal intensity on T2-weighted images. Moreover, enhancement is less intense in contrast-enhanced CT and MRI, and progressive enhancement is reported in pRCC (8). In CEUS, slow wash-in, fast wash-out, and homogeneous hypo-enhancement at peak are regarded as the most common characteristics of pRCC (9). Although lipid-poor AMLs also show a low signal intensity on T2-weighted images, they tend to show avid enhancement following contrast administration and can show a signal drop in opposed-phase images (10). In our case, partial nephrectomy was performed, because RCC could not be completely ruled out.
Considering the correlation of radiological and pathological findings of renomedullary interstitial cell tumor, which is histologically based on fibrotic stroma, the fibrotic tissue in the background of the tumor explained why renomedullary fibroma showed a low signal intensity on T2-weighted MRI images and delayed enhancement on MRI and CEUS. Besides, the mass was located in the medulla rather than in the cortex of the kidney and was particularly well visualized on MRI. The location of the tumor could be also an important factor in the differential diagnosis.
In conclusion, the imaging findings of renomedullary interstitial tumors include low-signal-intensity masses in the renal medulla on T1- and T2-weighted MRI and delayed enhancement on CEUS and dynamic MRI. However, there are no reports about the above dynamic enhancement imaging findings, which suggests that unnecessary nephrectomy can be prevented in the diagnosis of renomedullary interstitial cell tumors.