1. Introduction
Mucoceles are mucus cavity lesions associated with both the minor and the major salivary glands; they are among the most common benign soft tissue masses of the oral cavity (1). When located in the floor of the mouth, they are referred to as ranula because the resultant swelling resembles the air sacs of a frog (2). Although minor salivary glands are found in most parts of the oral cavity (except the gingiva), the prevalence of mucoceles varies depending on the specific location. In the tongue, mucoceles usually appear on the ventral surface (3). Mucoceles appearing on the tongue base are extremely rare; there are only a few such cases in the available literature on PubMed. We report one such rare case of a mucocele located on the base of the tongue.
2. Case Presentation
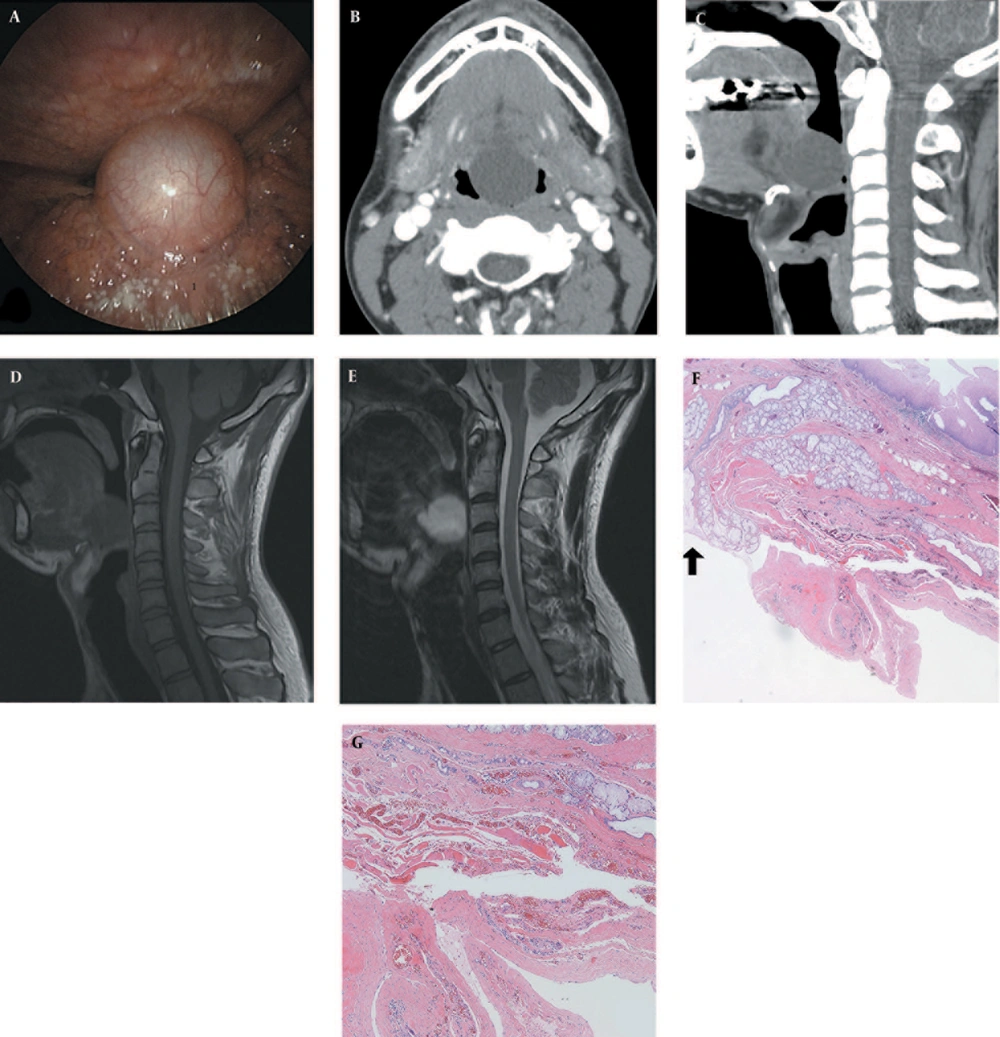
A 32-year-old man presented with a mass on the base of the tongue that was found on C-spine MRI incidentally. He smoked about 2.5 packs per day, but he had no clinical symptoms of dysphasia or hoarseness. Laryngoscopic examination revealed a soft movable cyst protruding from the midline of the tongue base without tenderness (Figure 1A). On the enhanced computed tomography (CT) scan of the neck, a thin-walled cystic mass (10 to 20 Hounsfield units [HUs]) was noted without an enhancing solid component, measuring 2.8 × 2.5 × 2.8 cm (Figure 1B and C). There was no connection between the cyst, the hyoid bone, and the thyroid gland. The cervical spine magnetic resonance imaging (MRI) scan, obtained at another hospital, showed high signal intensity on the T2-weighted image and slightly low signal intensity on the T1-weighted image when compared with the intrinsic tongue muscles (Figure 1D and E). The MRI revealed no solid component or fat in the lesion. We diagnosed the lesion as a thyroglossal duct cyst and performed mass excision under general anesthesia. The cyst has no epithelial lining or malignant cells, which was consistent with the appearance of mucoceles on microscopic examination (Figure 1F and G). The lesion healed completely without complications or recurrence on follow-up.
A 32-year-old man with a tongue-base mucocele. A, Laryngoscopy showed a smooth-margined, movable cyst at the midline of the tongue base; B and C, Enhanced CT scan depicted a well-defined cystic mass, mildly protruding between the genioglossus muscles on both sides without connection with the hyoid bone; D, and E, Lesion showed a slightly low signal intensity on the T1-weighted image and high signal intensity on the T2-weighted image without the fatty component on the fat suppressed image (not shown); F, Histopathologic examination revealed a large cystic space in the vicinity of minor salivary gland acini and ducts (hematoxylin and eosin stain, × 40). Extravasation of mucus from a salivary duct was noted (indicated by an arrow); G, The cystic space containing a mucus pool had no epithelial lining surrounded by fibrotic connective tissue (hematoxylin and eosin stain, × 100).
3. Discussion
We reported a case of a tongue-base mucocele that presented as a thin-walled, well-defined cystic mass. It showed T2 high signal intensity/T1 low signal intensity on MRI scans, similar to mucoceles presenting elsewhere in the oral cavity. MRIs of the mucoceles in the floor of mouth (ranula) usually show high signal intensity on T2-weighted images and low signal intensity on T1-weight images, although a high protein content in the cystic fluid may cause high signal intensity on T1-weighted images as well (4, 5).
Mucoceles are classified as mucous extravasation cysts or mucous retention cysts depending on their development mechanism (6). Extravasation cysts consist of extravasated mucus with surrounding connective tissue, whereas retention cysts represent mucus retained by the epithelial lining. Extravasation cysts are caused by physical trauma, such as biting or laceration; thus, the lower lip is a frequent site of these cysts, followed by the cheek, the ventral surface of the tongue, the floor of the mouth, and the retromolar pad area. They are common in teenagers and children (1, 7, 8). Most oral cavity mucoceles are extravasation cysts, particularly those found in the minor salivary glands. However, retention cysts result from a narrowed ductal opening caused by a sialolith or a mucus plug (2). They are usually found in the upper lip, the palate, or the floor of the mouth (7). They are common in older patients and less common than extravasation cysts.
The minor salivary gland of the human tongue is composed of three main groups: the von Ebner glands, the Weber glands, and the Blandin–Nuhn glands. The von Ebner glands, located in association with the circumvallate and the foliate papillae, are serous glands; the Weber glands, located along the lateral border of the tongue and posterior aspect of the dorsum of the tongue, are mucous glands; and the Blandin–Nuhn glands, located in the musculature of the anterior ventral surface of the tongue, are mixed mucous and serous glands (9). Jinbu et al. (2) described 26 cases of tongue mucoceles; all of them arose on the ventral surface of the tongue within the glands of Blandin–Nuhn. At the tongue base, Weber glands are responsible for mucoceles, but there are only two previous reports of mucoceles arising on the dorsal surface of the tongue (10, 11). This is the third report of mucoceles that originated from the Weber glands.
Differential diagnoses of tongue-base mucoceles include cystic lesions of the tongue base such as thyroglossal duct cysts as well as dermoid and epidermoid cysts. Thyroglossal duct cysts are found along the thyroglossal duct from the foramen cecum to the thyroid gland. If a thyroglossal duct cyst occurs at the tongue base, it can be difficult to distinguish from a mucocele, even with radiological scans. However, dermoid and epidermoid cysts in the oral cavity have a predilection for the root of the tongue and the floor of the mouth, and they appear as either intralesional fat (dermoid cysts) or diffusion restrictions (epidermoid cysts) on diffusion weighted images, which offers a way to differentiate them from mucoceles (12).
Clinical symptoms of oral mucoceles vary from asymptomatic to non-specific symptoms, including discomfort, interference with speech, and mastication and swallowing abnormalities, depending on the lesion’s size and location.
Surgical excision of lesion, with removal of the involved minor salivary gland, has been suggested as a treatment for medium-sized to large mucoceles (1, 13). According to Baurmash (1), the goal of surgery is to completely unroof the lesion along its entire periphery to both visualize and remove all of the glands present, thereby promoting healing without complications or recurrence. Small mucoceles are completely excised and primarily closed; in these cases; healing is rapid and uneventful. However, when only marsupialization is performed, the lesion can re-occur as soon as the draining site is repaired. Ellis et al. reported lesion recurrence after marsupialization, requiring additional surgical intervention (14). Alternative treatment methods include laser ablation, cryotherapy, electrocautery, and intralesional corticosteroid injections (13).